Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP A-043
Comparing the Predictive Value of Different Nutritional Assessment Tools for Mortality Risk in High Risk Elderly Patients Undergoing Percutaneous Coronary Intervention
By Kailun Yan, Jiawen Li, Kexin Zhang, Menglu Liu, Jinqing Yuan, Xueyan Zhao
Presenter
Kailun Yan
Authors
Kailun Yan1, Jiawen Li1, Kexin Zhang1, Menglu Liu1, Jinqing Yuan1, Xueyan Zhao1
Affiliation
Fuwai Hospital, China1
View Study Report
TCTAP A-043
High-Risk Intervention (Diabetes, Heart Failure, Renal Failure, Shock, etc)
Comparing the Predictive Value of Different Nutritional Assessment Tools for Mortality Risk in High Risk Elderly Patients Undergoing Percutaneous Coronary Intervention
Kailun Yan1, Jiawen Li1, Kexin Zhang1, Menglu Liu1, Jinqing Yuan1, Xueyan Zhao1
Fuwai Hospital, China1
Background
Nutritional status is crucial for assessing frailty in elderly patients undergoing percutaneous coronary intervention (PCI). Accurate nutritional assessment may aid in managing complications and improving prognosis in this high risk population. Commonly utilized objective nutritional assessment tools include the Prognostic Nutritional Index (PNI), Geriatric Nutritional Risk Index (GNRI) and Controlling Nutritional status (CONUT) score. However, there is a lack of systematic comparison of these tools in elderly PCI patients.
Methods
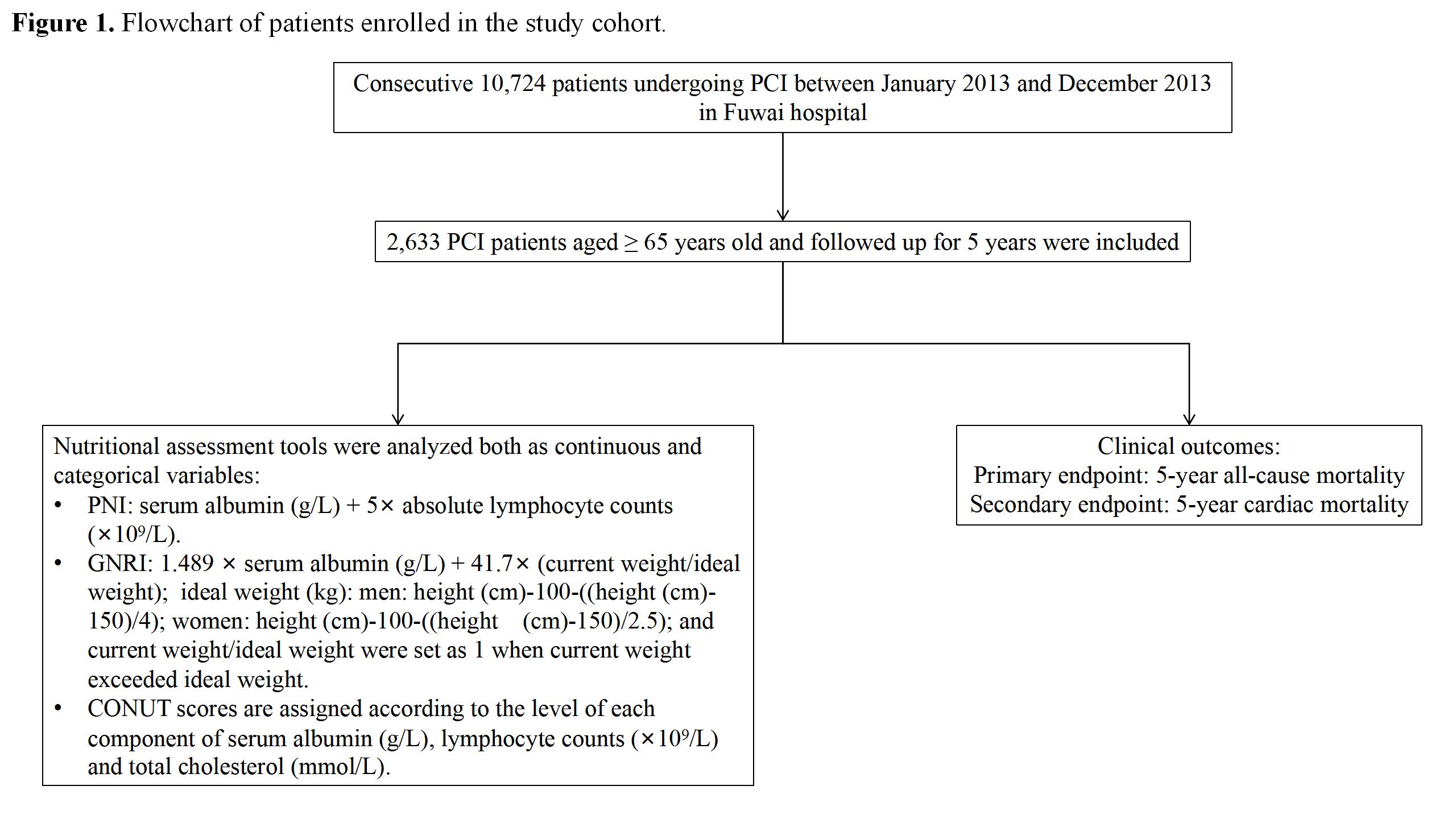
This prospective cohort study enrolled 10,724 consecutive patients who underwent PCI at Fuwai Hospital (National center for cardiovascular disease, Peking Union Medical College) between January 2013 and December 2013. Among them, 2,633 patients aged 65 years or older were followed for 5 years. PNI, GNRI, and CONUT were analyzed as continuous and categorical variables, which were categorized into normal, mild or moderate-severe malnutrition based on their clinical cutoff points. The primary endpoint was all-cause mortality and the secondary endpoint was cardiac mortality (Figure 1).
Results
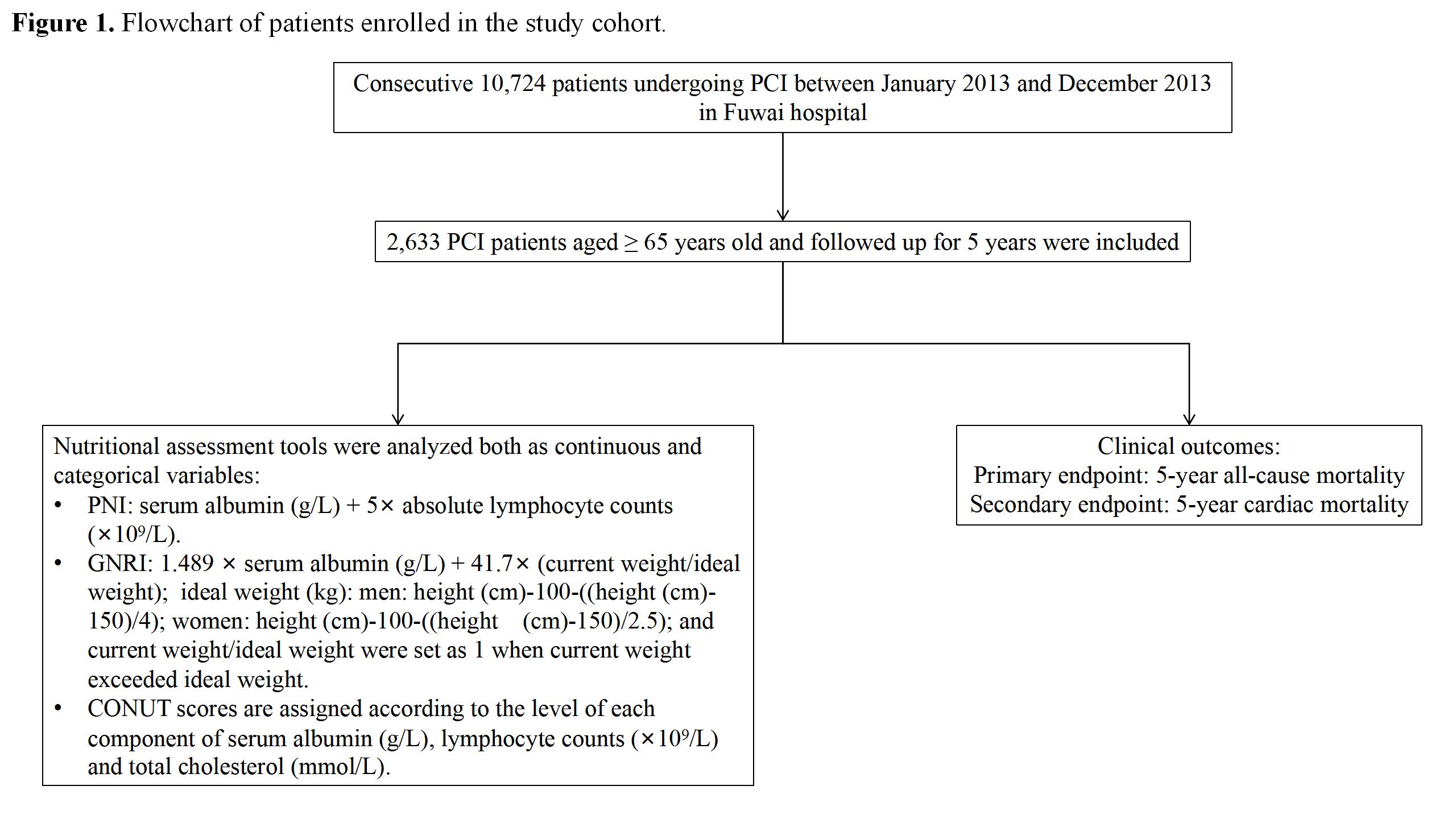
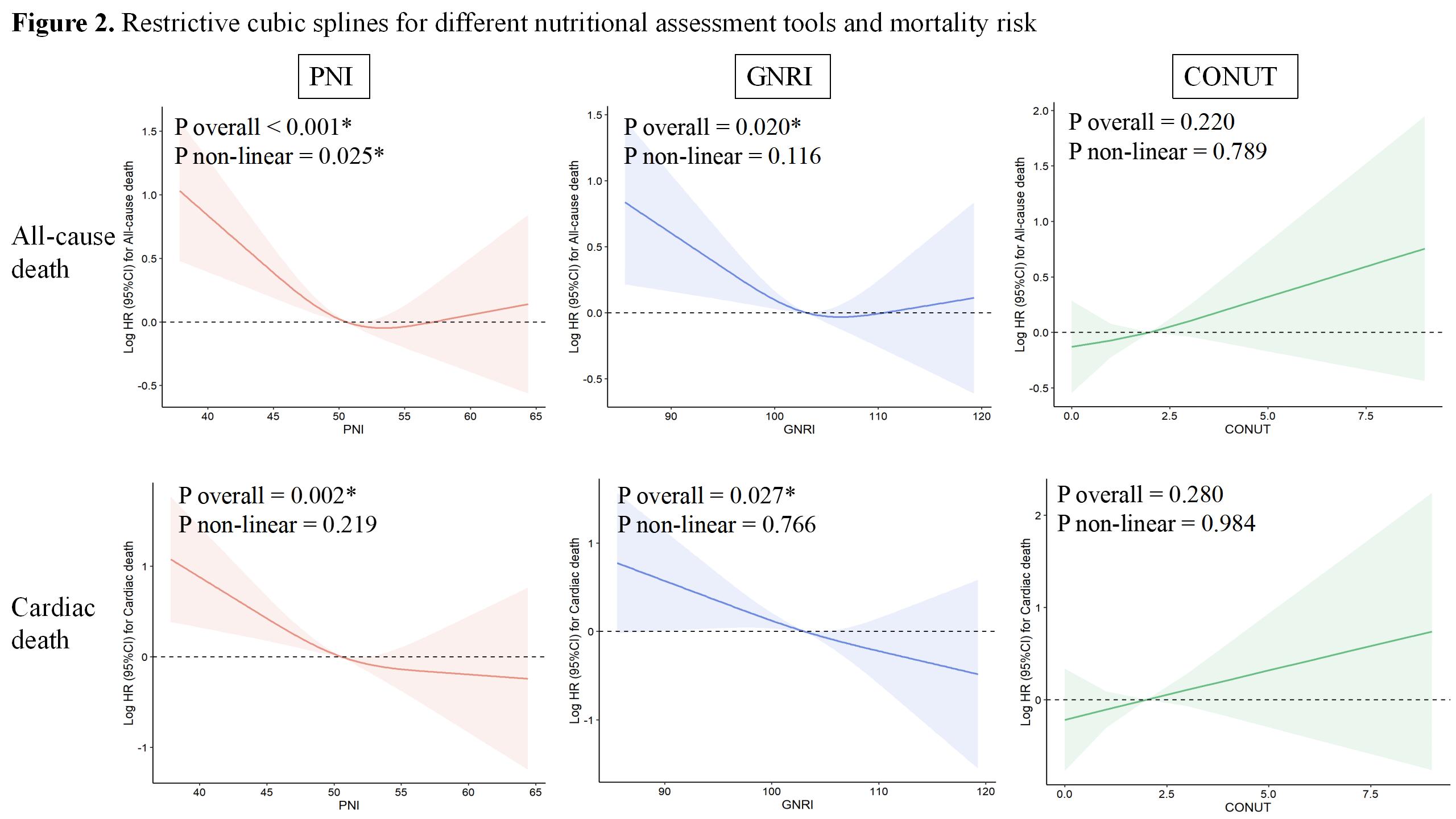
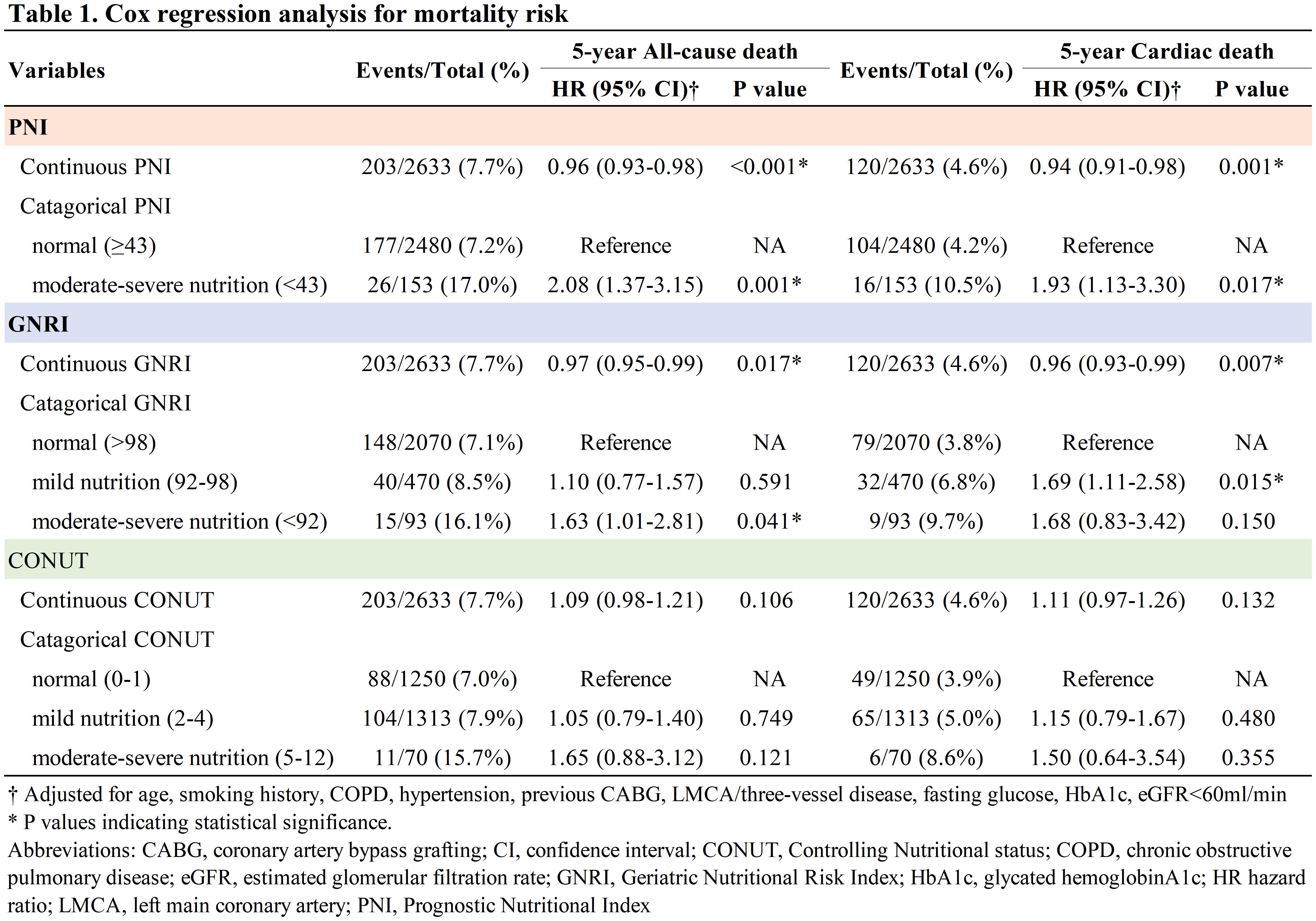
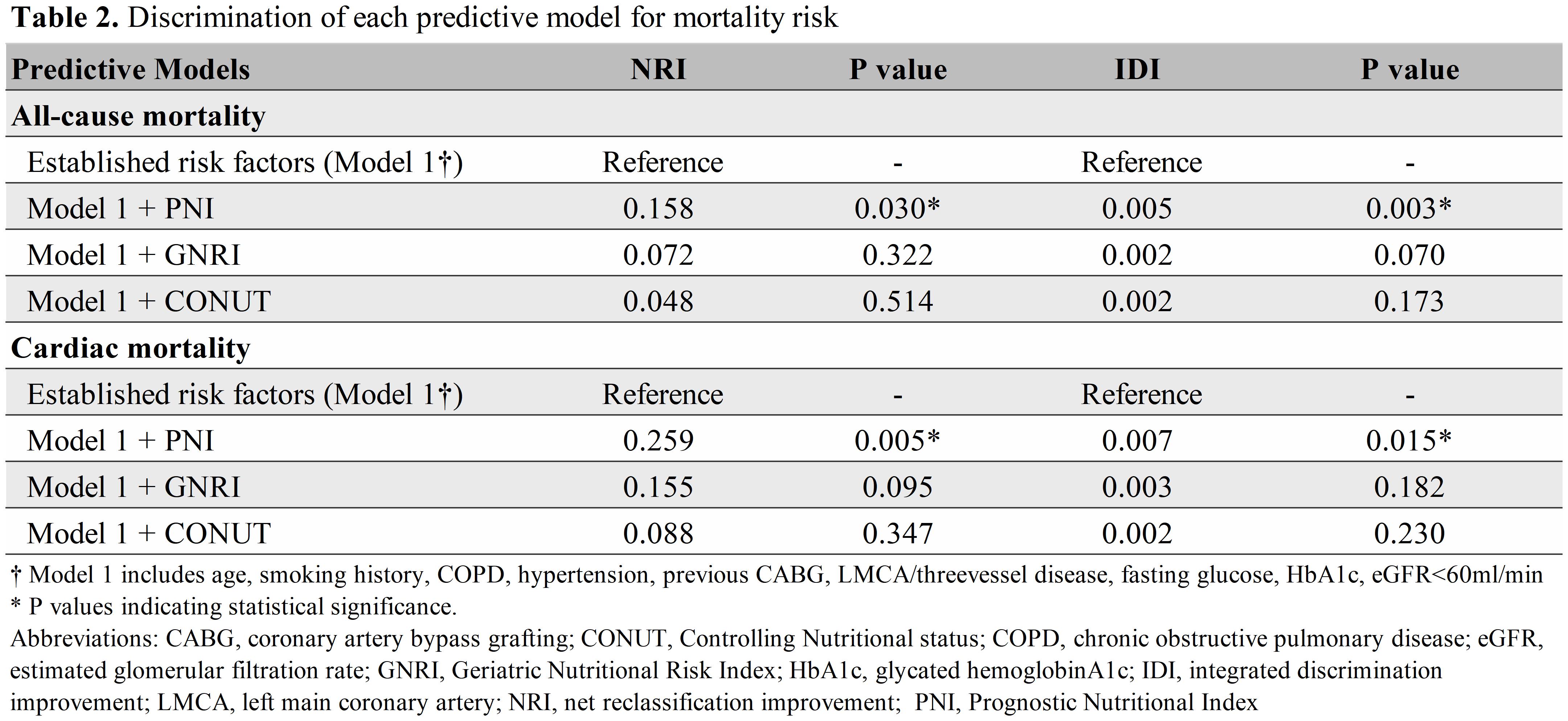
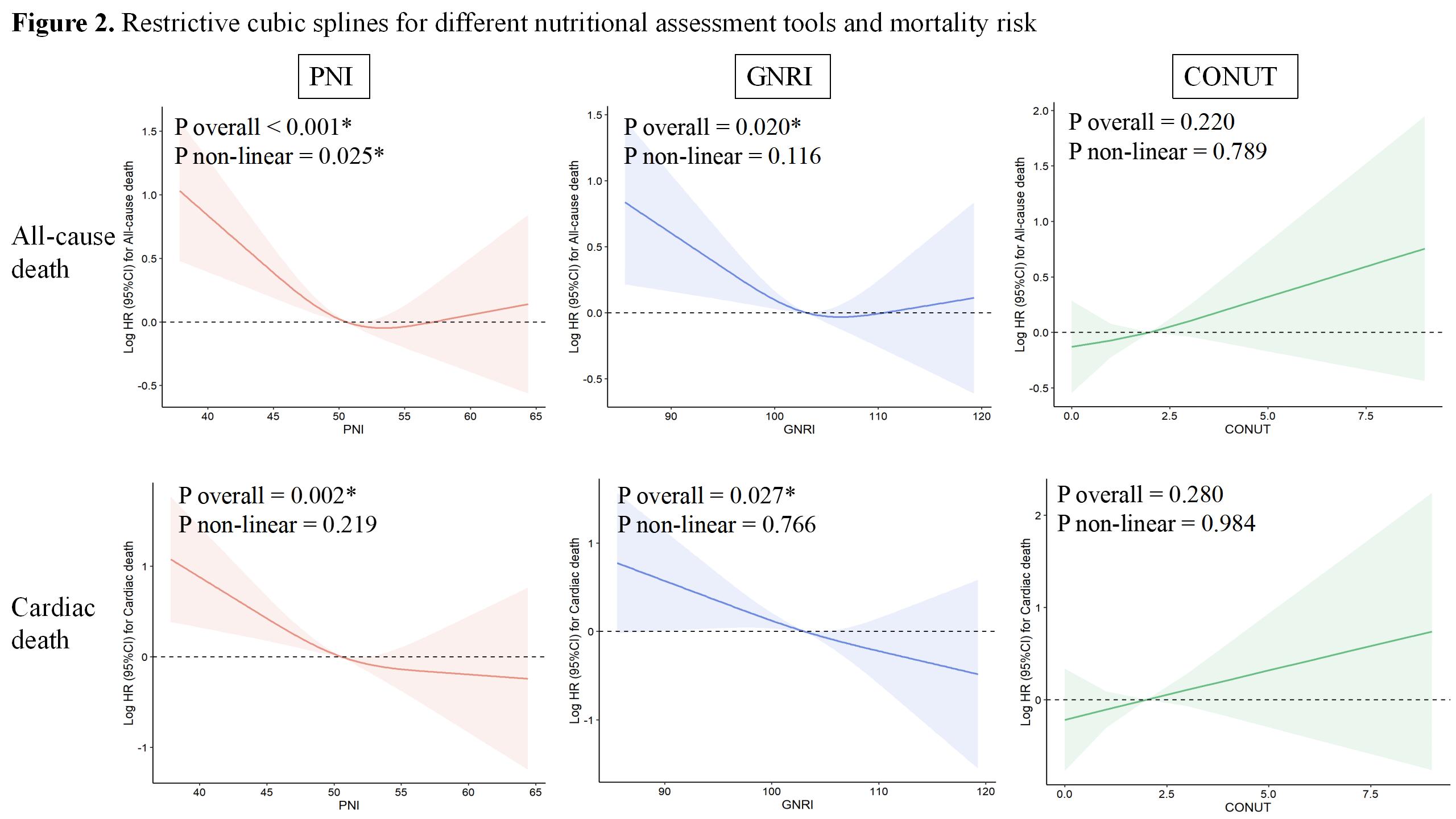
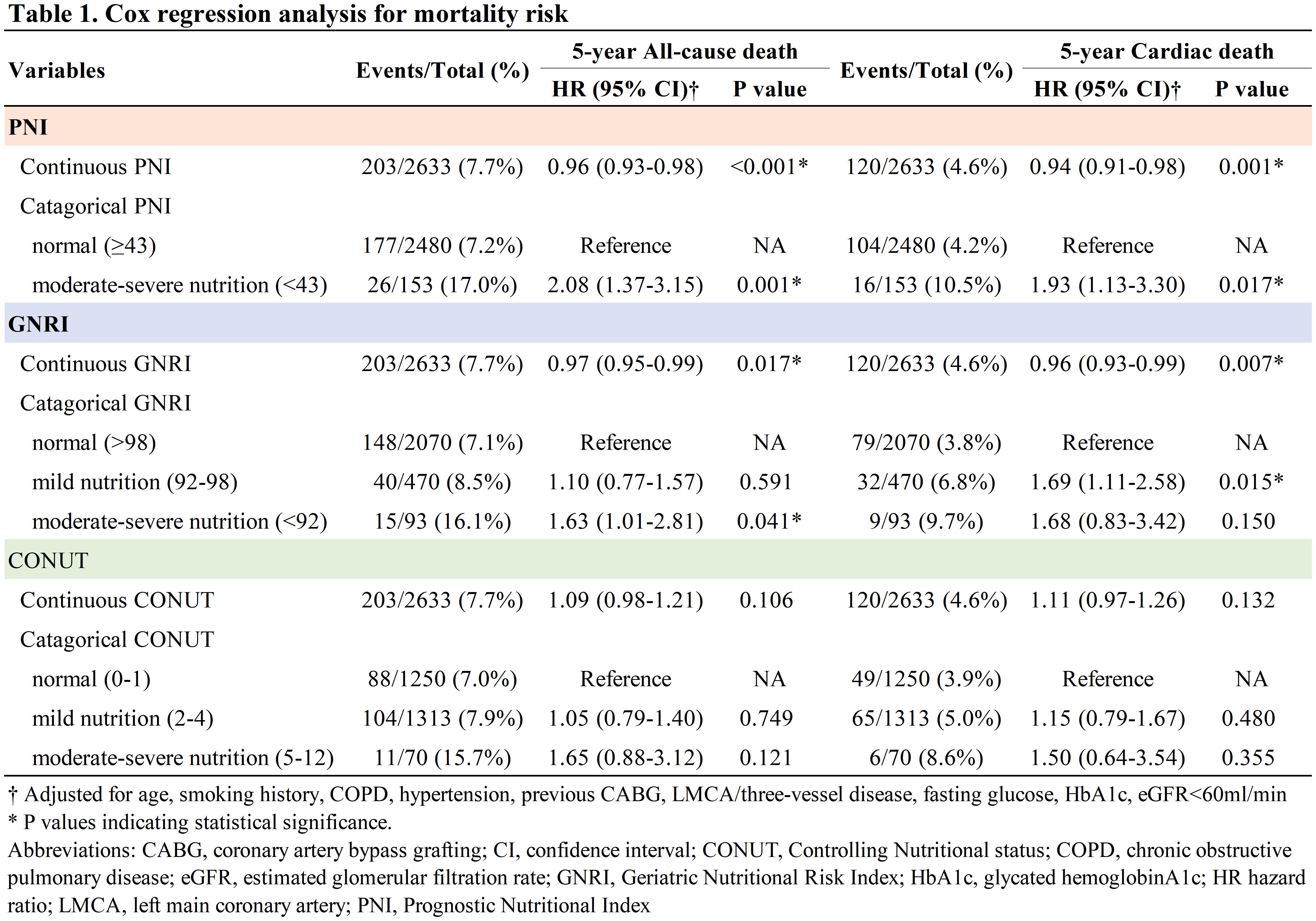
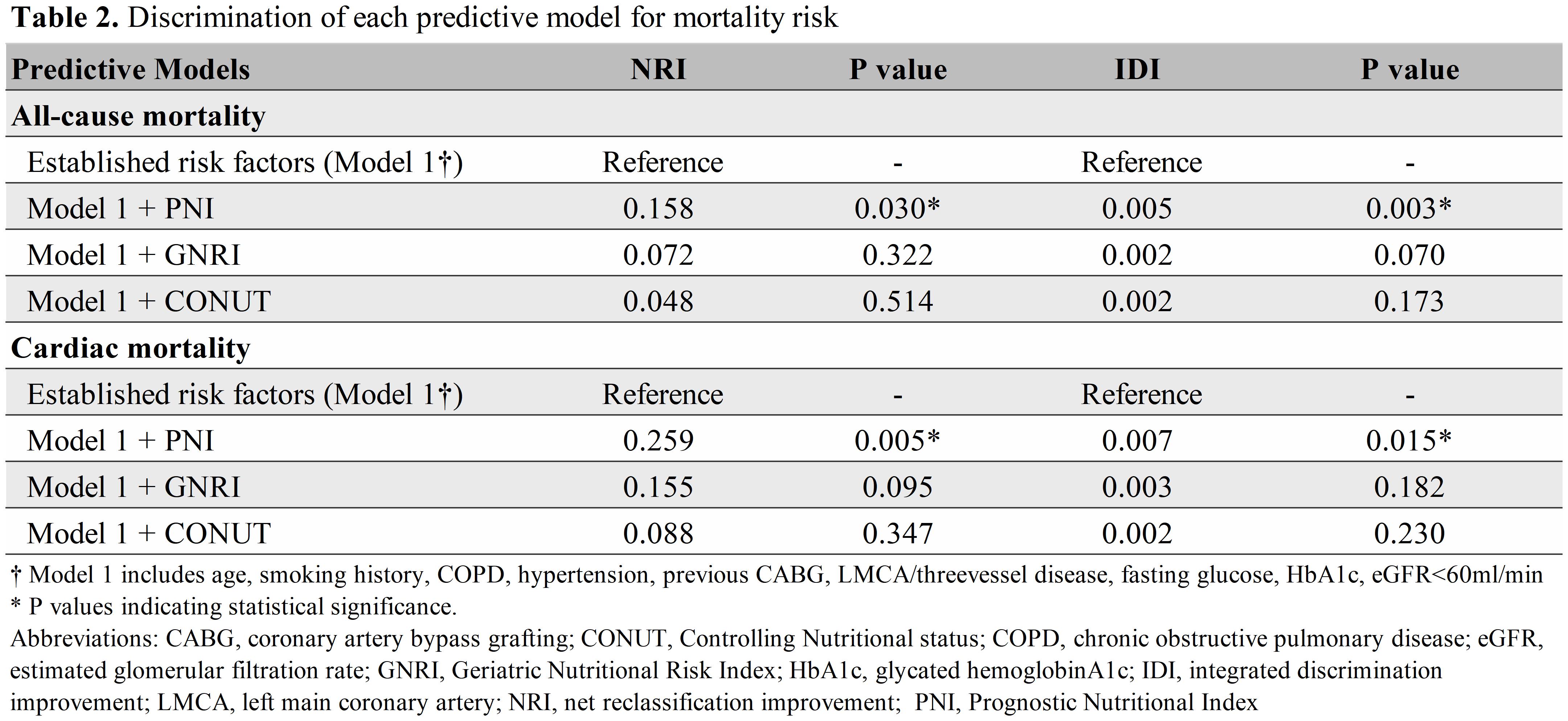
A total of 2,633 PCI patients, aged 70.9 ± 4.6 years on average, with 63.6% male, were followed. Over 5 years, 203 (7.7%) all-cause death and 120 (4.6%) cardiac death occurred. Restrictive cubic splines indicated that declining PNI and GNRI were associated with increased all-cause and cardiac mortality (both p < 0.05), while CONUT was not (Figure 2). Multivariate Cox regression analysis revealed that moderate-severe malnutrition as defined by PNI was significantly associated with a 2.08-fold increase in all-cause mortality (HR 2.08, 95% CI 1.37 - 3.15) and a 1.93-fold increase in cardiac mortality (HR 1.93, 95% CI 1.13 - 3.30) (Table 1), while malnutrition defined by GNRI and CONUT did not show similar associations. Additionally, the inclusion of PNI to the model established with traditional risk factors significantly improved the discrimination and reclassification for the prediction of all-cause mortality (net reclassification improvement [NRI] 0.158, p = 0.030; integrated discrimination improvement [IDI] 0.005, p = 0.003) and cardiac mortality (NRI 0.259, p = 0.005; IDI 0.007, p = 0.015), whereas GNRI and CONUT did not (Table 2).
Conclusion
PNI and its classified malnutrition status revealed superior value for predicting long-term mortality risk compared to GNRI and CONUT, making PNI a valuable nutritional assessment tool in clinical management for high risk elderly PCI patients. Incorporating PNI in clinical assessments may facilitate early identification of patients at elevated risk due to malnutrition, enabling more individual management and improving long-term survival outcomes.


