Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP A-009
Insights and Outcomes of PCI in a Sri Lankan Tertiary Care Center: A Real-World Study
By M.B.Faslur Rahuman, Nimali Fernando, Chathurika Kempitiya, Anushka Peiris, Pasan Abeysenevi, Amanda Nawarathna, Reeni Robert, Pubudu De Silva
Presenter
M.B.Faslur Rahuman
Authors
M.B.Faslur Rahuman1, Nimali Fernando1, Chathurika Kempitiya1, Anushka Peiris1, Pasan Abeysenevi1, Amanda Nawarathna1, Reeni Robert1, Pubudu De Silva2
Affiliation
National Hospital of Sri Lanka, Sri Lanka1, Ministry of Health, Sri Lanka2
View Study Report
TCTAP A-009
ACS/AMI
Insights and Outcomes of PCI in a Sri Lankan Tertiary Care Center: A Real-World Study
M.B.Faslur Rahuman1, Nimali Fernando1, Chathurika Kempitiya1, Anushka Peiris1, Pasan Abeysenevi1, Amanda Nawarathna1, Reeni Robert1, Pubudu De Silva2
National Hospital of Sri Lanka, Sri Lanka1, Ministry of Health, Sri Lanka2
Background
Outcomes of percutaneous coronary intervention (PCI) varies across different regions of the world. Due to the lack of comprehensive data on the clinical aspects and outcomes of PCI in Sri Lanka, this study was conducted at a cardiac center in Colombo to assess the rates of failure, complications, re-infarction, consecutive revascularization, and mortality associated with PCI. The findings of this study can contribute to improving the management of CAD patients in Sri Lanka and serve as a valuable resource for healthcare policymakers at both national and regional levels, providing up-to-date benchmarks for PCI practices.
Methods
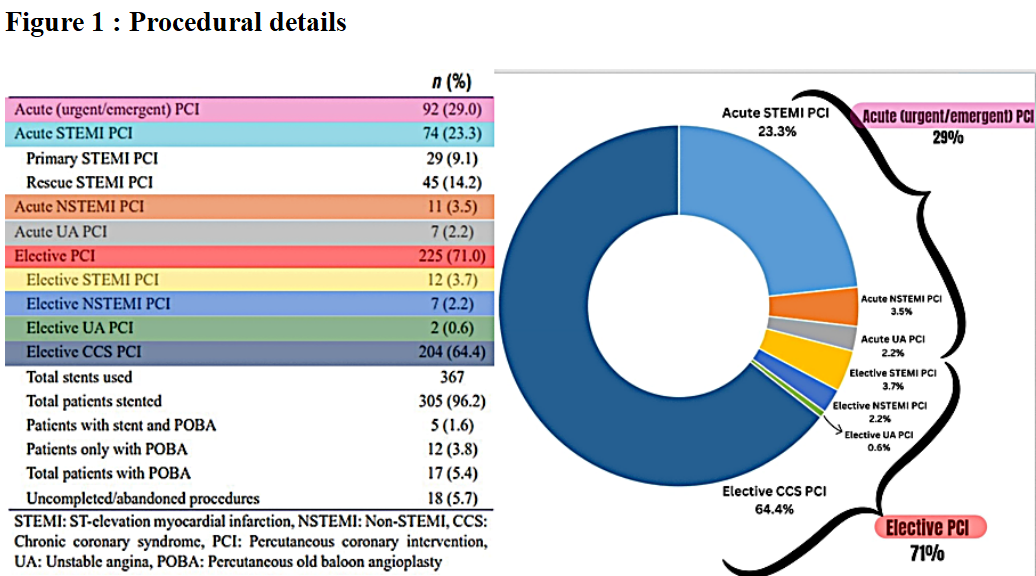
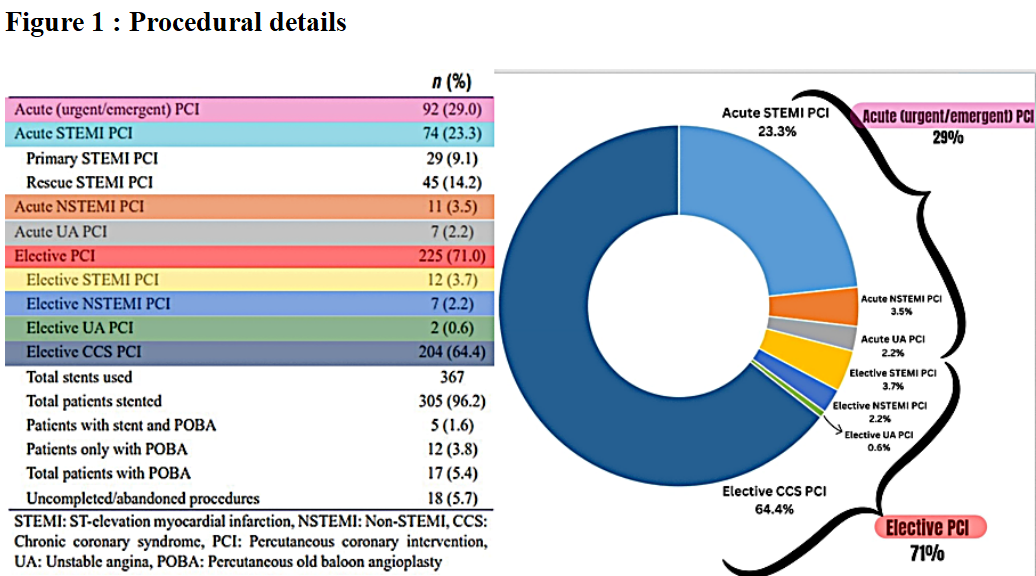
This prospective descriptive study included all patients who underwent PCI at one unit of National heart center in Colombo, between March to December 2022. Primary information was collected from the clinic and angiographic records using data sheets. These included socio demographic features, clinical features of acute coronary syndrome (ACS) and chronic coronary syndrome (CCS), CAD risk factors, comorbidities, results of non invasive tests for evidence of inducible ischemia, treatment, procedural details, complications, hospital outcomes and survival information for one, three and six months.Acute PCI comprises of both emergency PCI (emergent procedure that needs to be performed preferably within 24 hours) and urgent PCI (urgent procedure that needs to be performed preferably within 72 hours). Elective PCI is a non urgent type of revascularization performed electively. Those who received prior thrombolysis at the first contact point for the current STEMI event underwent rescue PCI while those who did not receive prior thrombolysis at the first contact point underwent primary PCI. Patients who underwent PCI with preplanned date which are not included in acute, primary or rescue PCI are considered as elective PCI. Ethical clearance was obtained from the Ethical Review Committee of National Hospital of Sri Lanka (NHSL).
Results
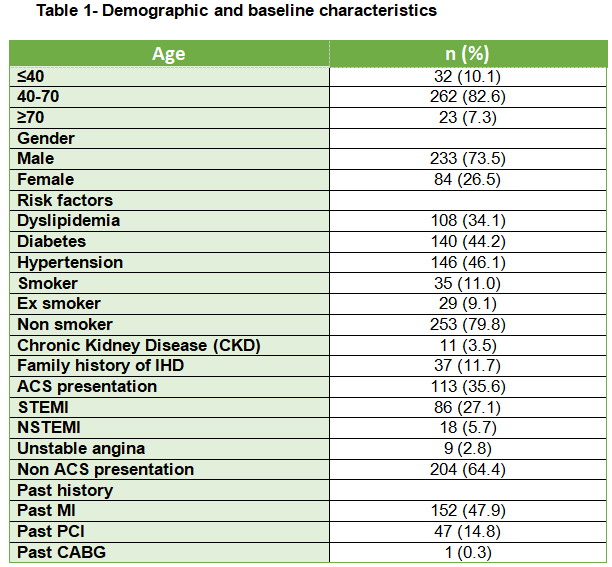
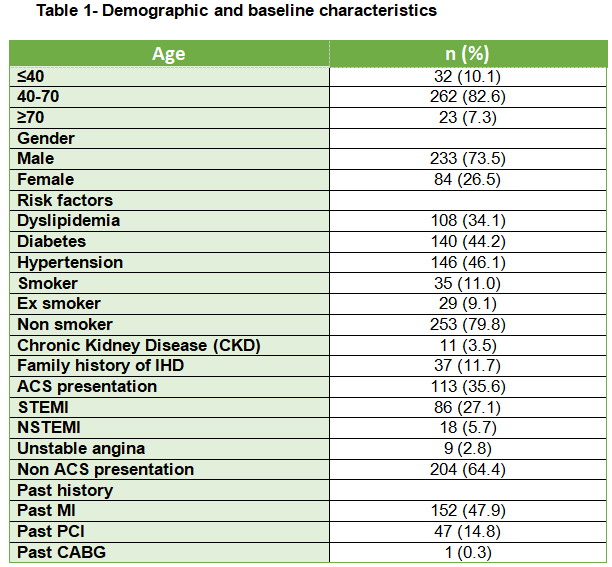
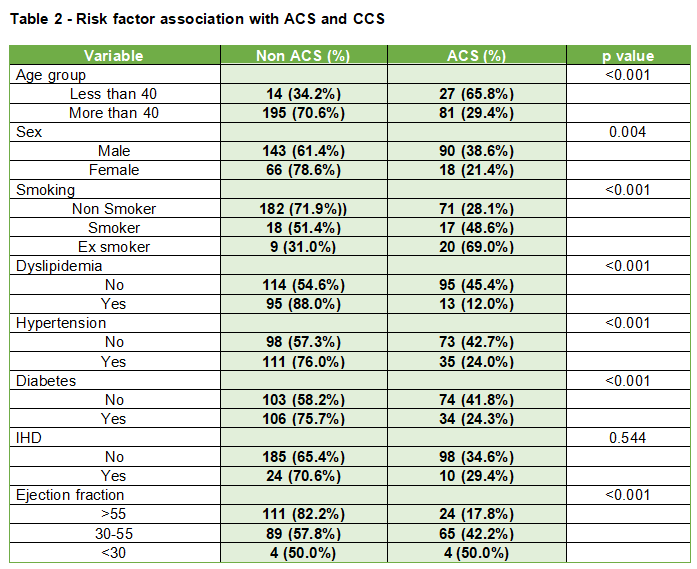
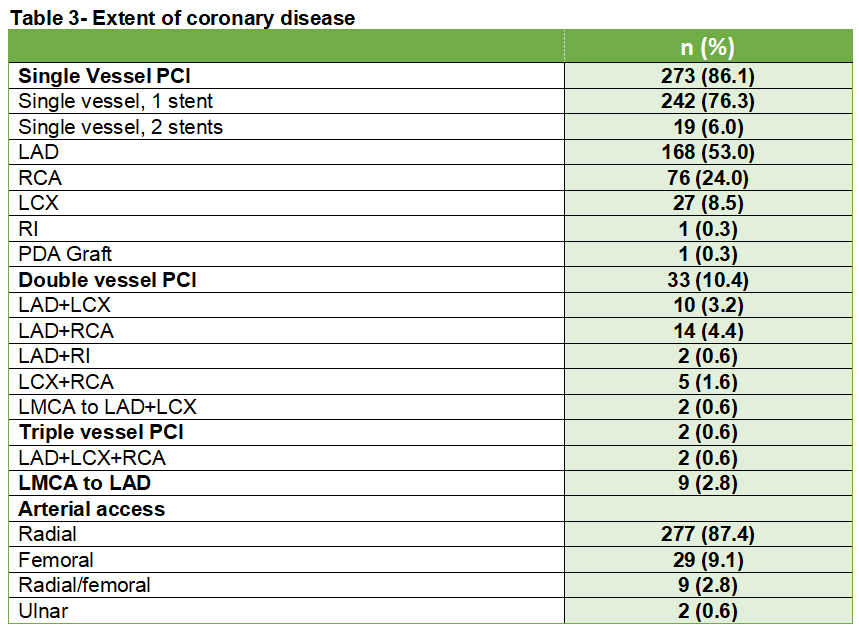
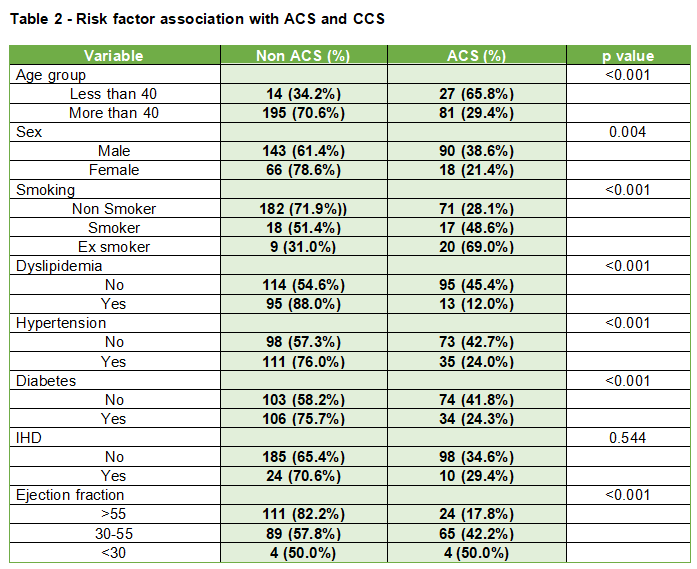
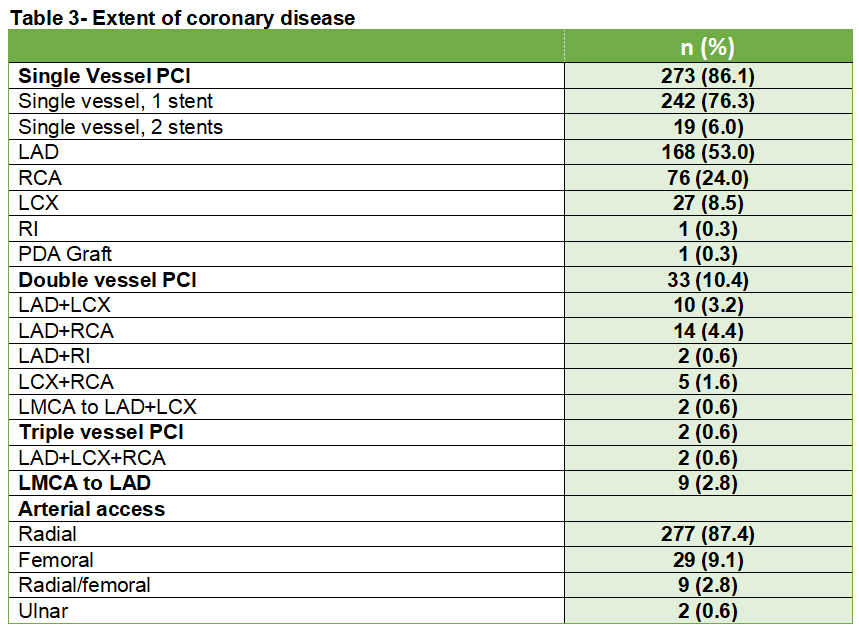
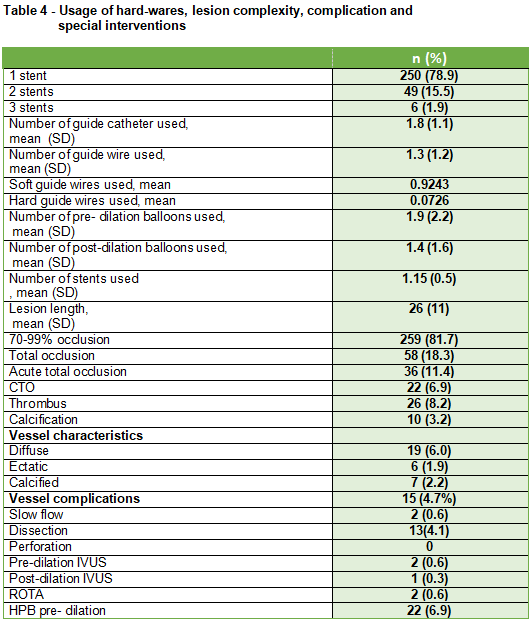
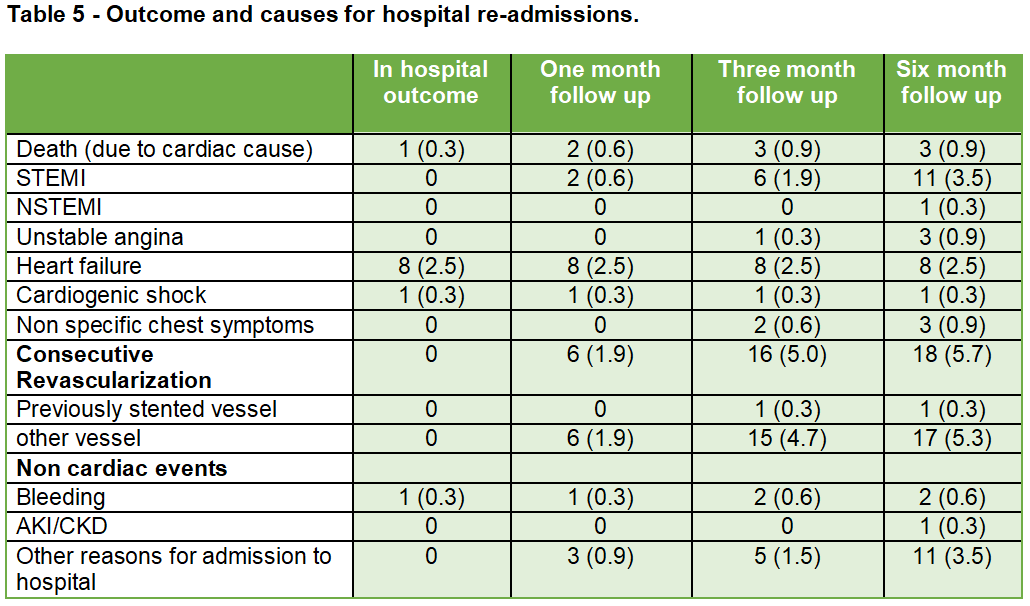
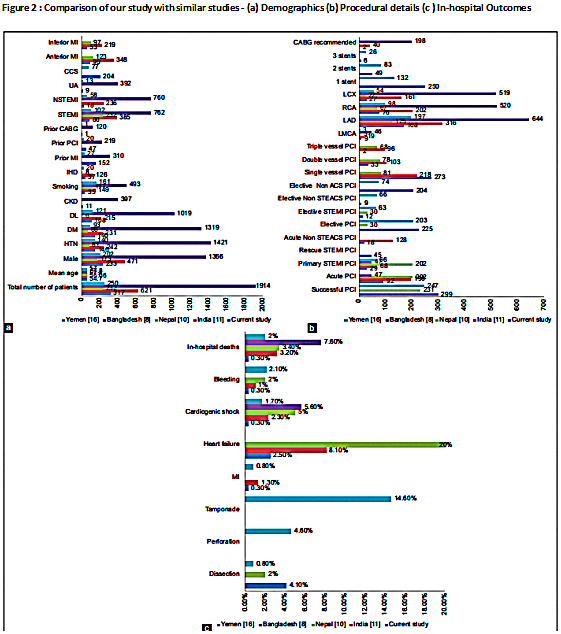
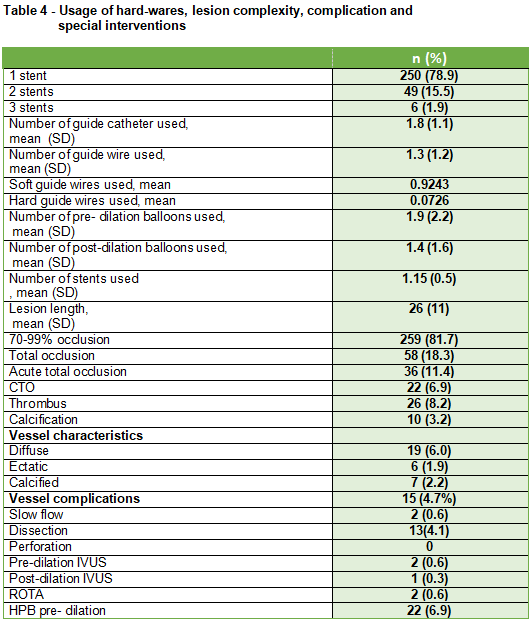
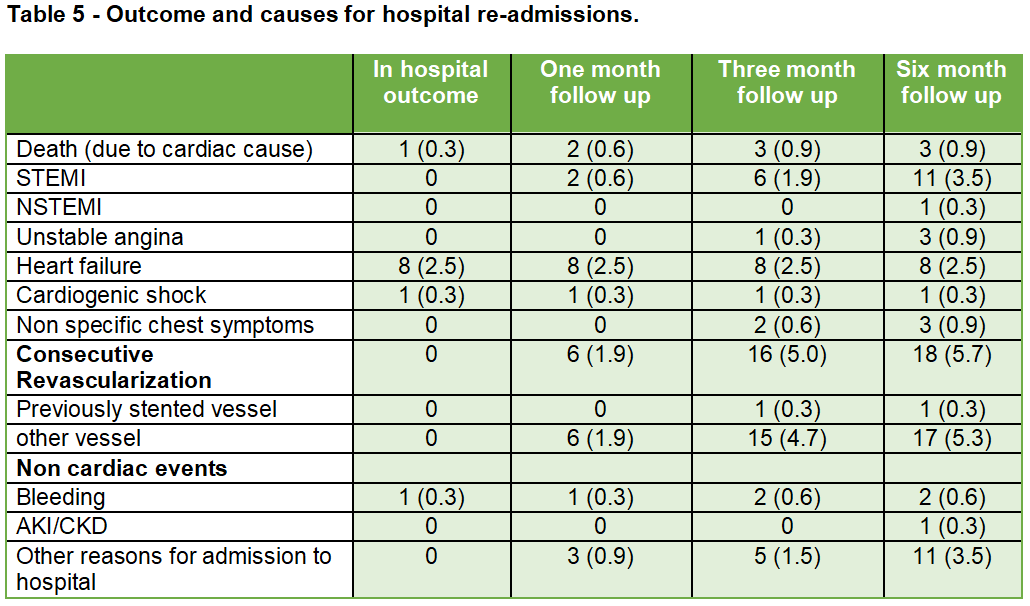
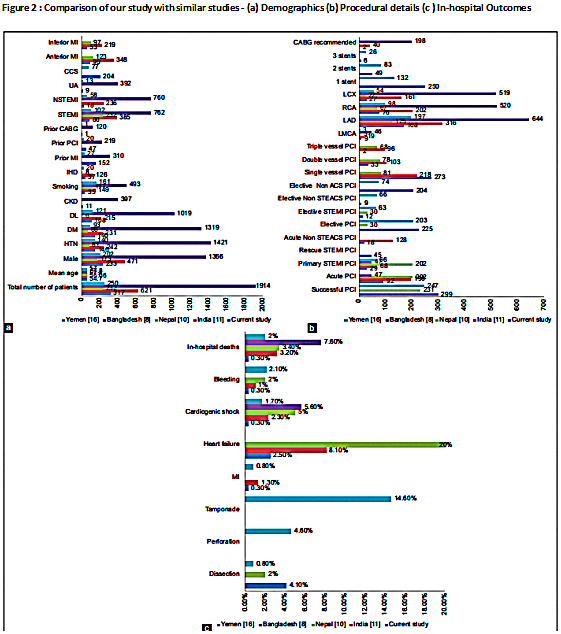
Among 317 patients included in the analysis, 89.9% were ≥40 years old, with a mean age of 54.7 (SD 11) and 73.5% were male. Multiple risk factors were seen in 53 (16.7%), and 69 (21.8%) had 2 risk factors. Hypertension was the most common and Chronic Kidney Disease (CKD) is the least common risk factor observed. The most common presentation was Chronic Coronary Syndrome (CCS), 65.9% with 6.9% chronic total occlusion (CTO) cases. Within Acute Coronary Syndrome (ACS) cases, the highest percentage (27.1%) was attributed to ST Elevation Myocardial Infarction (STEMI), with 18.3% being anterior MI, suggesting the Left anterior descending (LAD) artery was most commonly affected. The LAD artery was treated with PCI in 168 (53.3%), whereas the right coronary artery was treated in 76 (24.0%) and the left circumflex artery in 27 (8.5%). Anterior STEMI (90, 28.4%) was the most common followed by inferior STEMI (53, 16.7%), as a current event in the ACS group or past event in the CCS group. Of the anterior STEMI cases, 58 (18.3%) presented as ACS, while the remaining 32 (10.1%) were reported as a past history in the CCS group. In the case of inferior STEMI, 28 (8.8%) presented as ACS, and the remaining 25 (7.8%) were reported as a past history in the CCS group. Approximately 273 (86.1%) patients had single vessel PCI. Double vessel disease (DVD) PCI was performed in 33 (10.4%) patients, triple vessel disease (TVD) PCI in 2 (0.6%) patients, while 9 (2.8%) patients underwent left main PCI. Transradial access was obtained in 87.4%. Despite a 6.9% CTO, a high procedural success rate of 94.3% was observed. The in-hospital mortality rate was low at 0.3%, and the 6-month mortality rate was 0.9%.Comparing our study with other South Asian and Middle Eastern countries (figure 2), Sri Lanka stands out with the lowest mean age, number of smokers, and total cases of ACS presentation. Our study has the lowest STEMI cases, hence primary PCI is also lowest compared to regional studies which mainly include ACS patients. In our study, there was a significant predominance of SVD, whereas in other regions, the common angiographic outcome was a combination of SVD and DVD.
Conclusion
Despite the limited sample size, our study provides valuable insights into the current practices and outcomes of PCI in Sri Lanka. Despite the constraints of limited resources, we observed a high success rate and minimal complications. Attention to optimize the ACS care in Sri Lanka is a current necessity to cover more primary and rescue PCI in a timely manner.


