Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP A-015
Residual Cholesterol and Inflammatory Risk and Its Association With Recurrent Cardiovascular Events in East Asian Patients After Percutaneous Coronary Intervention
By Ang Gao, Tingting Guo, Zhiqiang Yang, Xue Li, Hong Qiu, Runlin Gao
Presenter
Ang Gao
Authors
Ang Gao1, Tingting Guo1, Zhiqiang Yang1, Xue Li1, Hong Qiu1, Runlin Gao1
Affiliation
Fuwai Hospital, China1
View Study Report
TCTAP A-015
ACS/AMI
Residual Cholesterol and Inflammatory Risk and Its Association With Recurrent Cardiovascular Events in East Asian Patients After Percutaneous Coronary Intervention
Ang Gao1, Tingting Guo1, Zhiqiang Yang1, Xue Li1, Hong Qiu1, Runlin Gao1
Fuwai Hospital, China1
Background
Owing to the aging population and the increasing prevalence of cardiometabolic risk factors, cardiovascular deaths have become the leading cause of mortality in China. Statins has been recognized as the cornerstone of secondary prevention. However, statin-treated coronary artery disease patients still suffer from recurrent cardiovascular events even after an early revascularization strategy, an issue commonly ascribed to the problem of ‘residual risk’. Residual cholesterol risk and residual inflammatory risk were both shown to be important predictors for the prognosis of patients and therapies targeting at residual cholesterol and inflammatory risk also delivered positive results. However, there’s a lack of measurements of inflammatory and cholesterol levels during follow-up and the relative importance of inflammatory risk and cholesterol risk after taking lipid-lowering medications remained elusive. Besides, the inflammatory level, especially in East Asian patients, is generally lower than in Western populations. Whether the Western standard (high sensitive C-reactive protein ≥ 2mg/L) used for evaluating residual risk could also be applied in East Asian patients was still unknown. Lastly, previous studies have found limited evidence about increased risk for recurrent vascular events caused by inflammatory burden in populations with achieved cholesterol levels after percutaneous coronary intervention treatment. The current study aimed to explore the high-risk high sensitive C-reactive protein cutoff value for percutaneous coronary intervention-treated patients in East Asian and evaluated the effect of residual inflammatory and cholesterol risk on the prognosis of that population after taking lipid-lowering treatment.
Methods
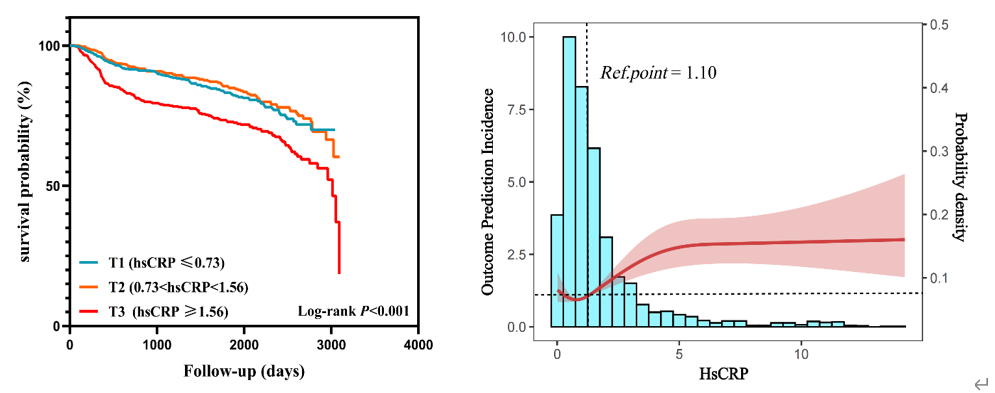
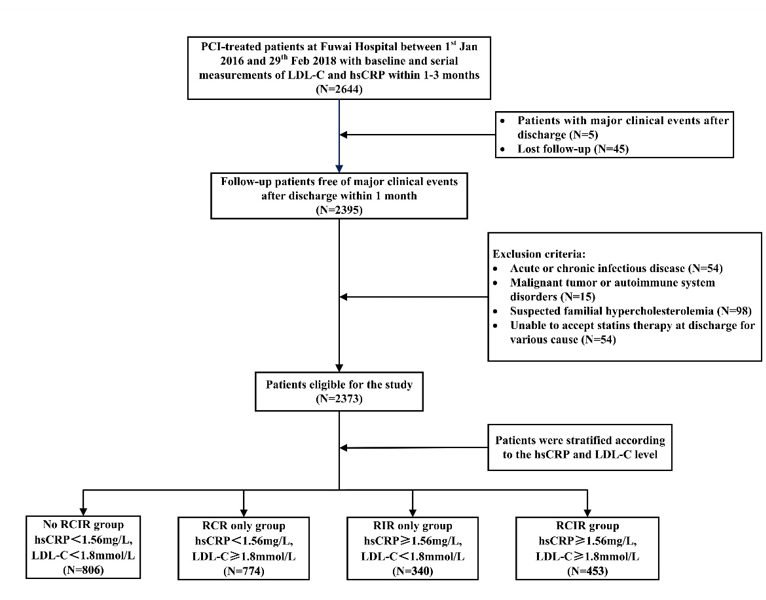
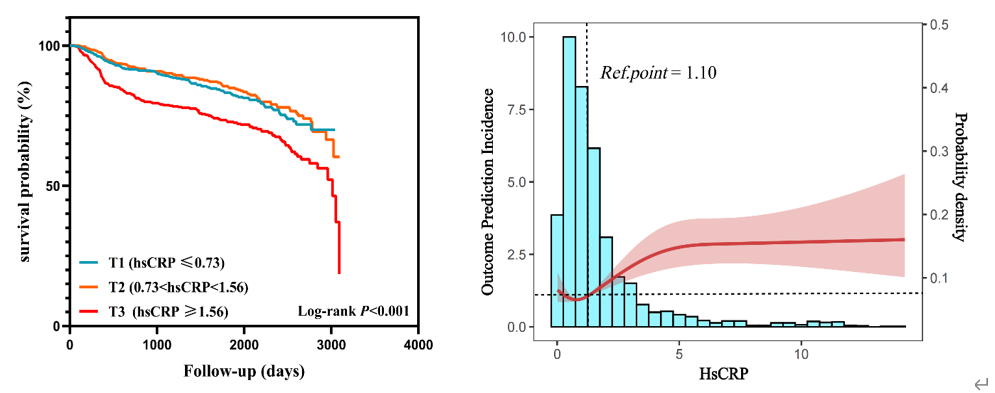
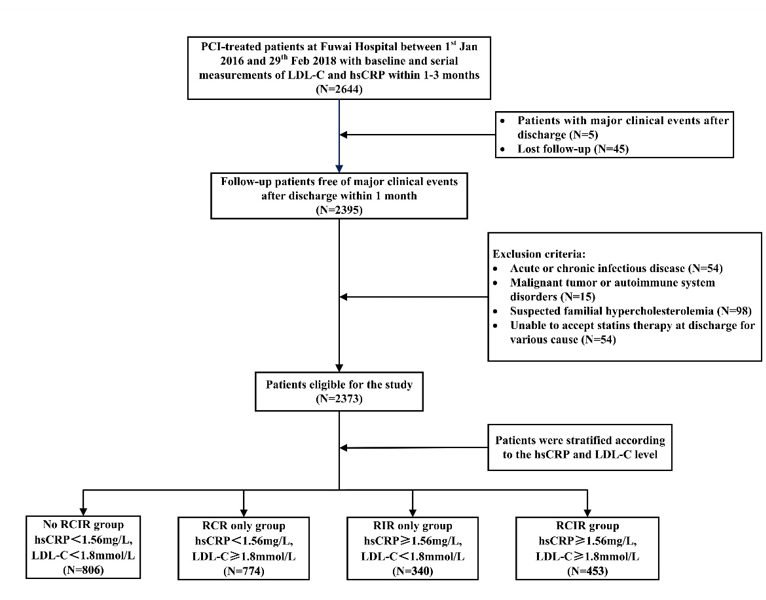
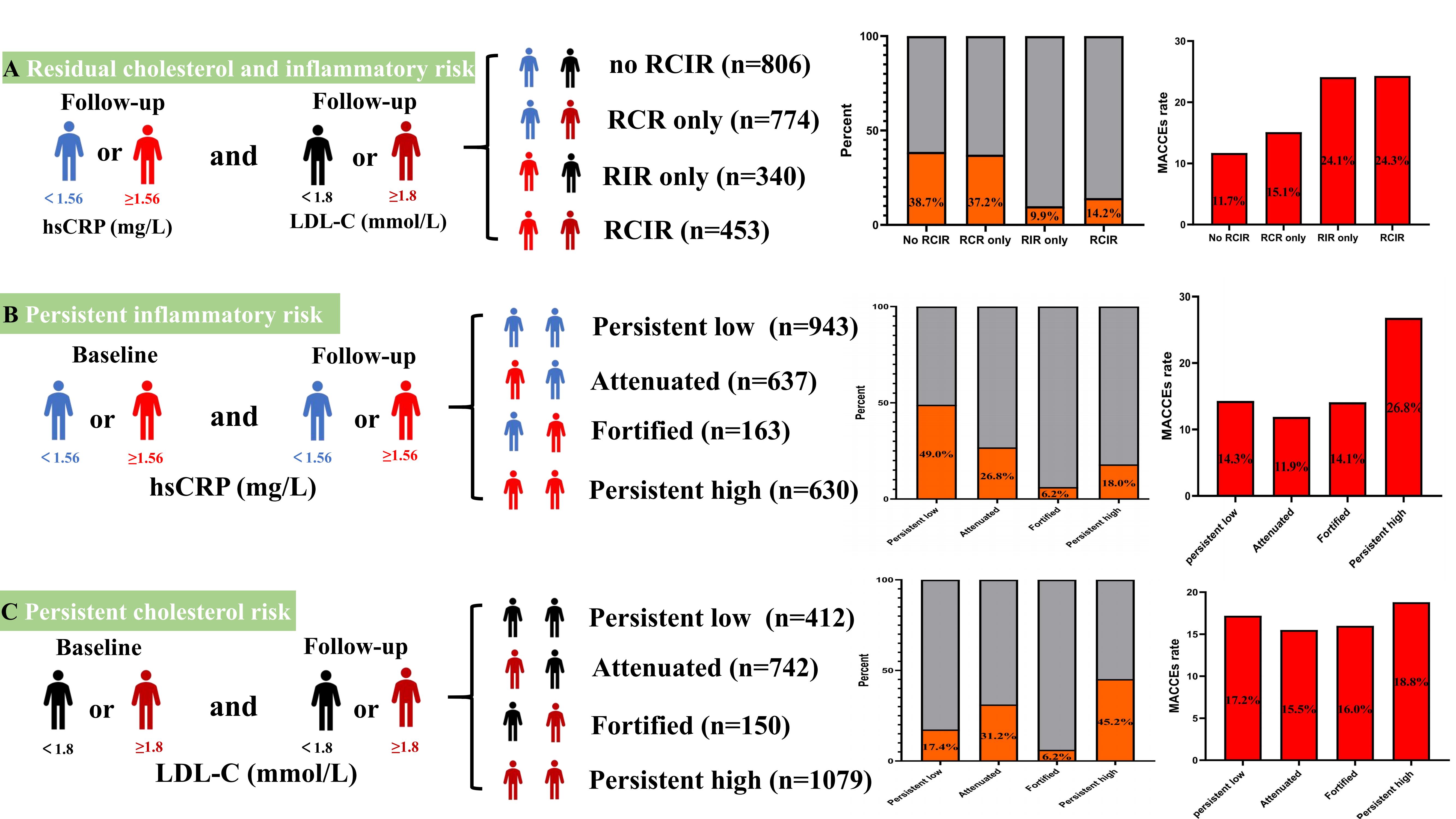
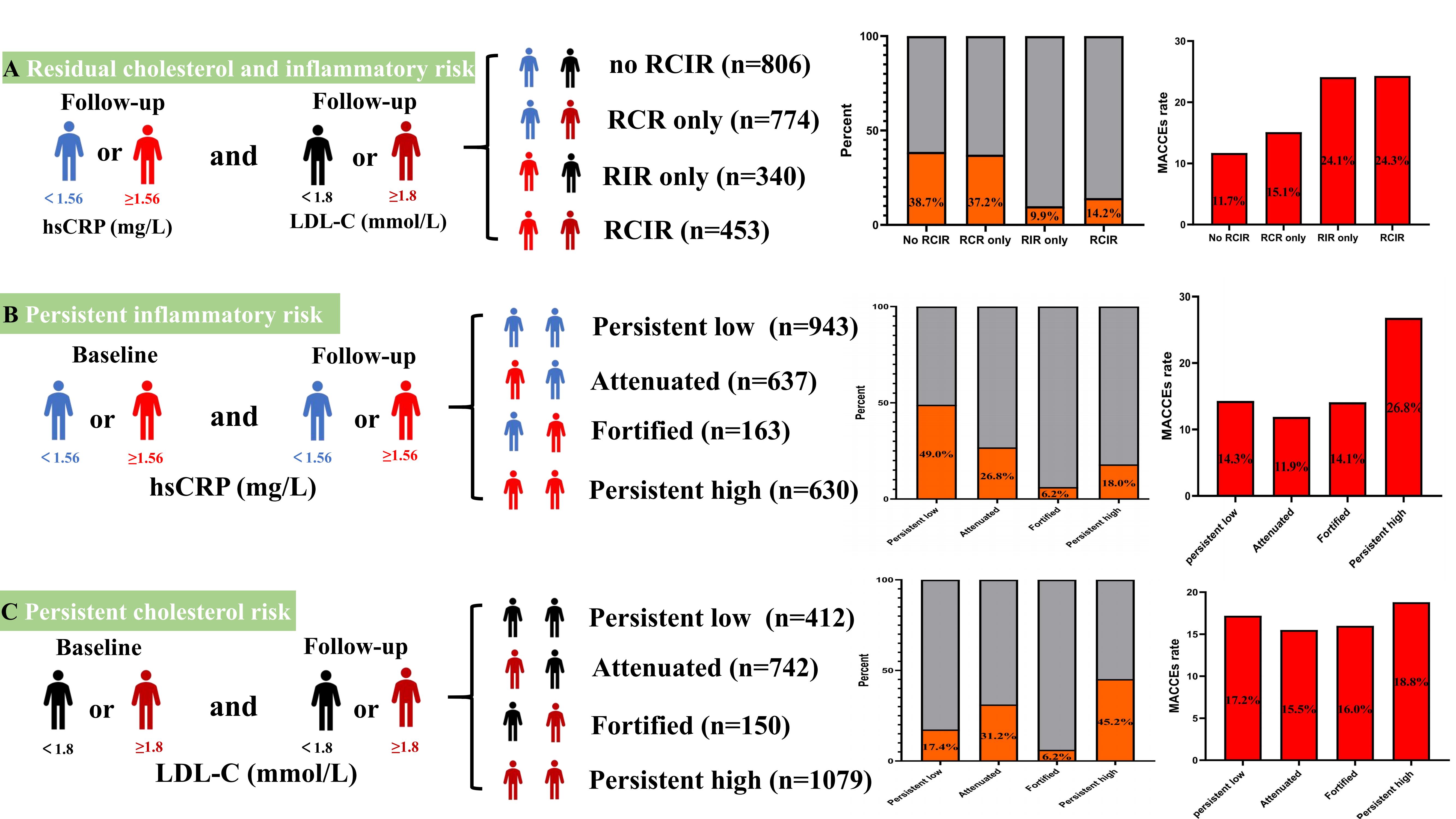
A total of 2373 consecutive percutaneous coronary intervention (PCI) -treated patients at Fuwai Hospital between 1st January 2016 and 29th February 2018 with serial measurements of high sensitive C-reactive protein (hsCRP) and low density lipoprotein cholesterol (LDL-C) levels were recruited into this single-center, retrospective observational study. The primary endpoint of this study was the occurrence of major adverse cardiovascular and cerebrovascular events (MACCEs) after PCI, defined as the composite of cardiovascular death, non-fatal acute myocardial infarction (AMI), recurrent coronary revascularization, or cerebrovascular events comprising stroke or transient ischemic attack. The participants were classified into 3 groups according to the follow-up hsCRP levels: T1: hsCRP ≤ 0.73 mg/L; T2: 0.73 < hsCRP < 1.56 mg/L; T3: hsCRP ≥ 1.56 mg/L. As is shown in Figure 1, Follow-up hsCRP tertile could independently predict the occurrence of MACCEs (T3 versus T1, adjusted HR 1.79, 95% CI: 1.41 to 2.28, p < 0.001). Restricted cubic spline analysis showed a linear relationship between follow-up hsCRP levels and the risks of MACCEs when the hsCRP ≥ 1.10 mg/L. Accordingly, the cutoff value of hsCRP for high residual inflammatory risk in the current study was set as 1.56 mg/L. We further divided these patients into 4 groups according to the residual cholesterol and inflammatory risk: No residual inflammatory and cholesterol risk (RCIR) group: hsCRP < 1.56 mg/L, LDL-C < 1.8 mmol/L; Residual cholesterol risk (RCR) only group: hsCRP < 1.56 mg/L, LDL-C ≥ 1.8 mmol/L; Residual inflammatory risk (RIR) only group: hsCRP ≥ 1.56mg/L, LDL-C < 1.8 mmol/L; RCIR group: hsCRP ≥ 1.56 mg/L, LDL-C ≥ 1.8 mmol/L. The detailed enrolment procedure is depicted in Figure 2. The association between cholesterol risk and inflammatory risk and MACCEs was determined using a multivariable Cox regression model after adjusting for the following confounders: Current smoker, hypertension, diabetes mellitus, body mass index, previous history of coronary revascularization and myocardial infarction, ACC/AHA defined type B2 and C lesions.
Results
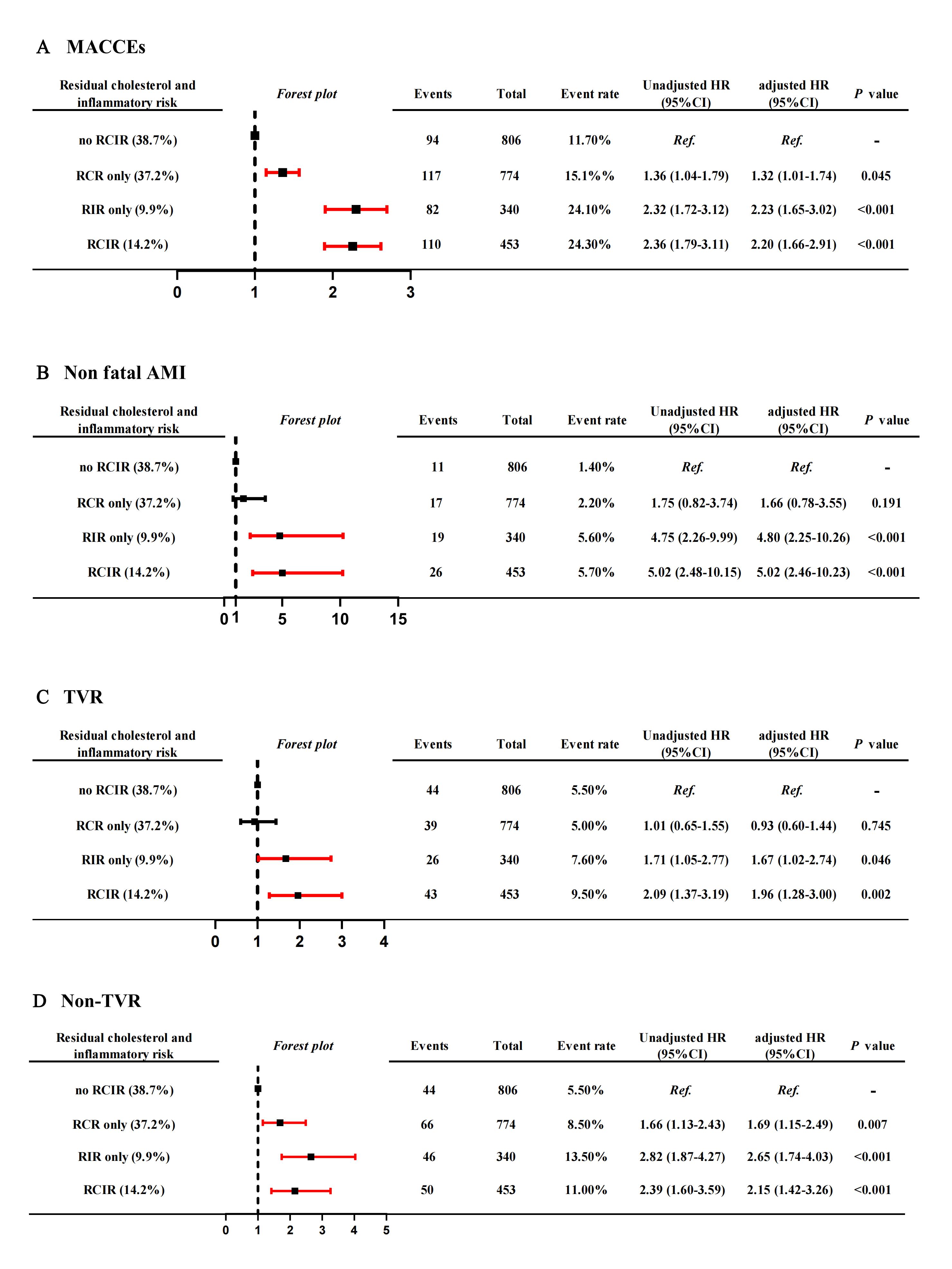
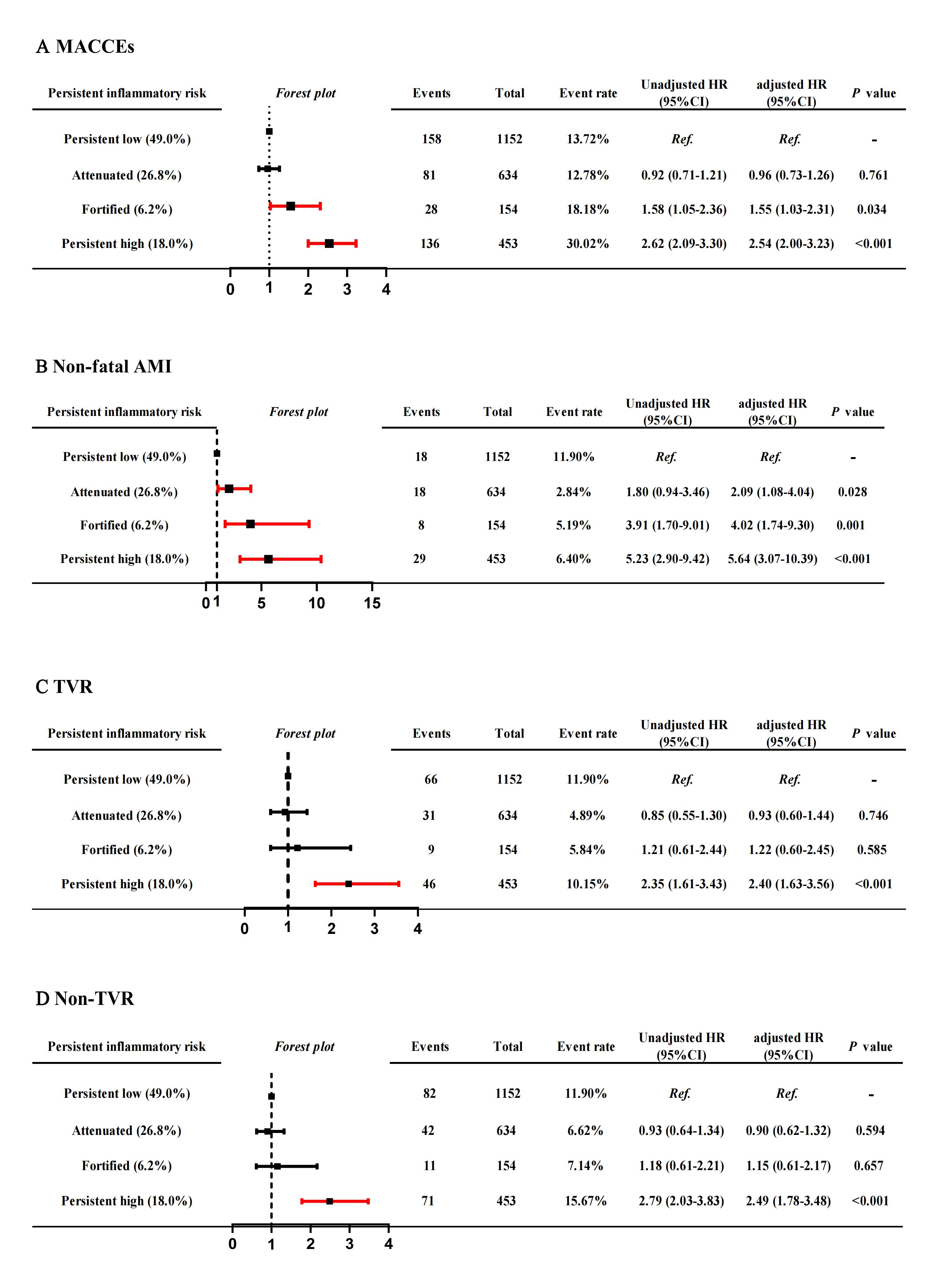
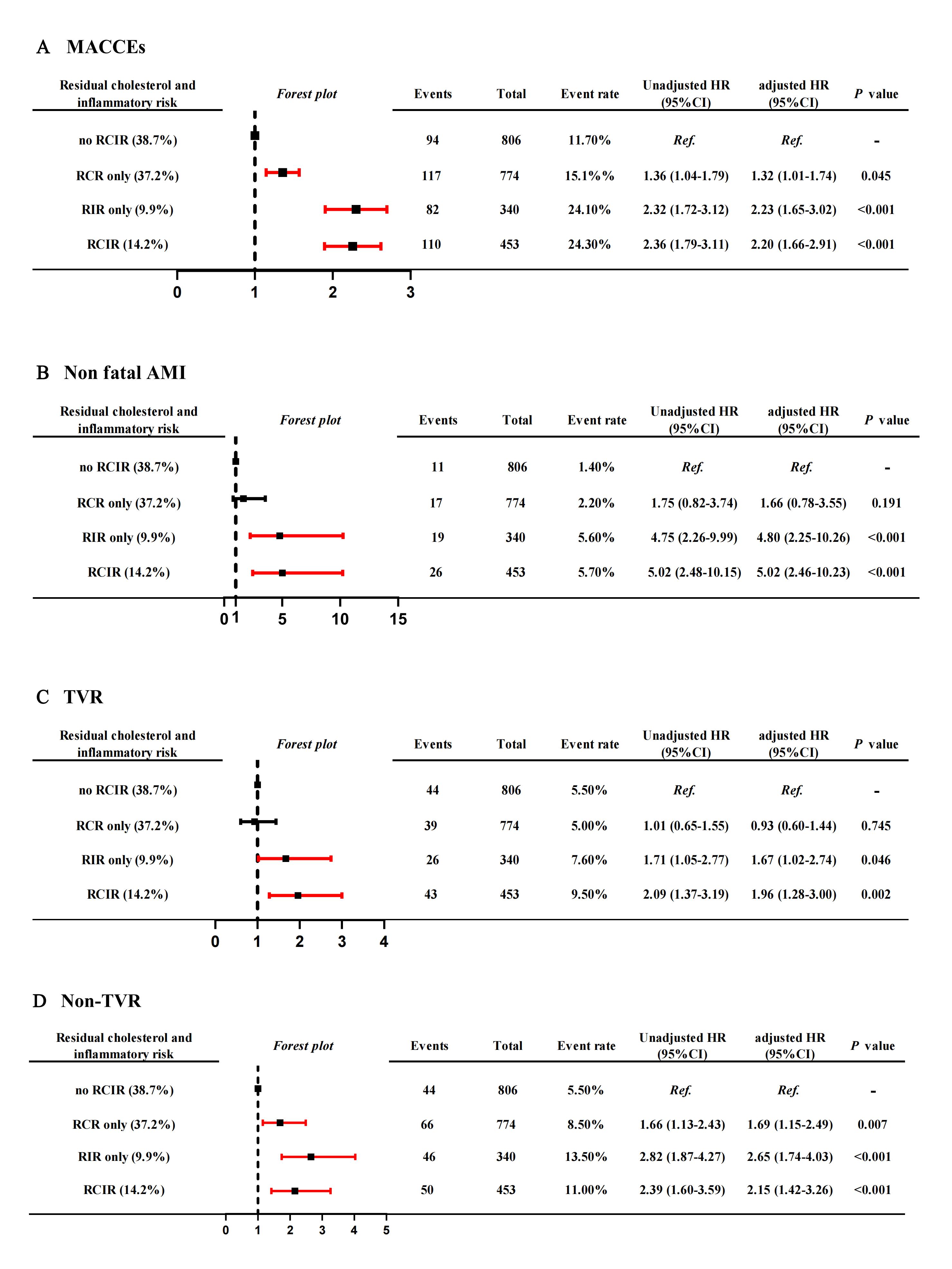
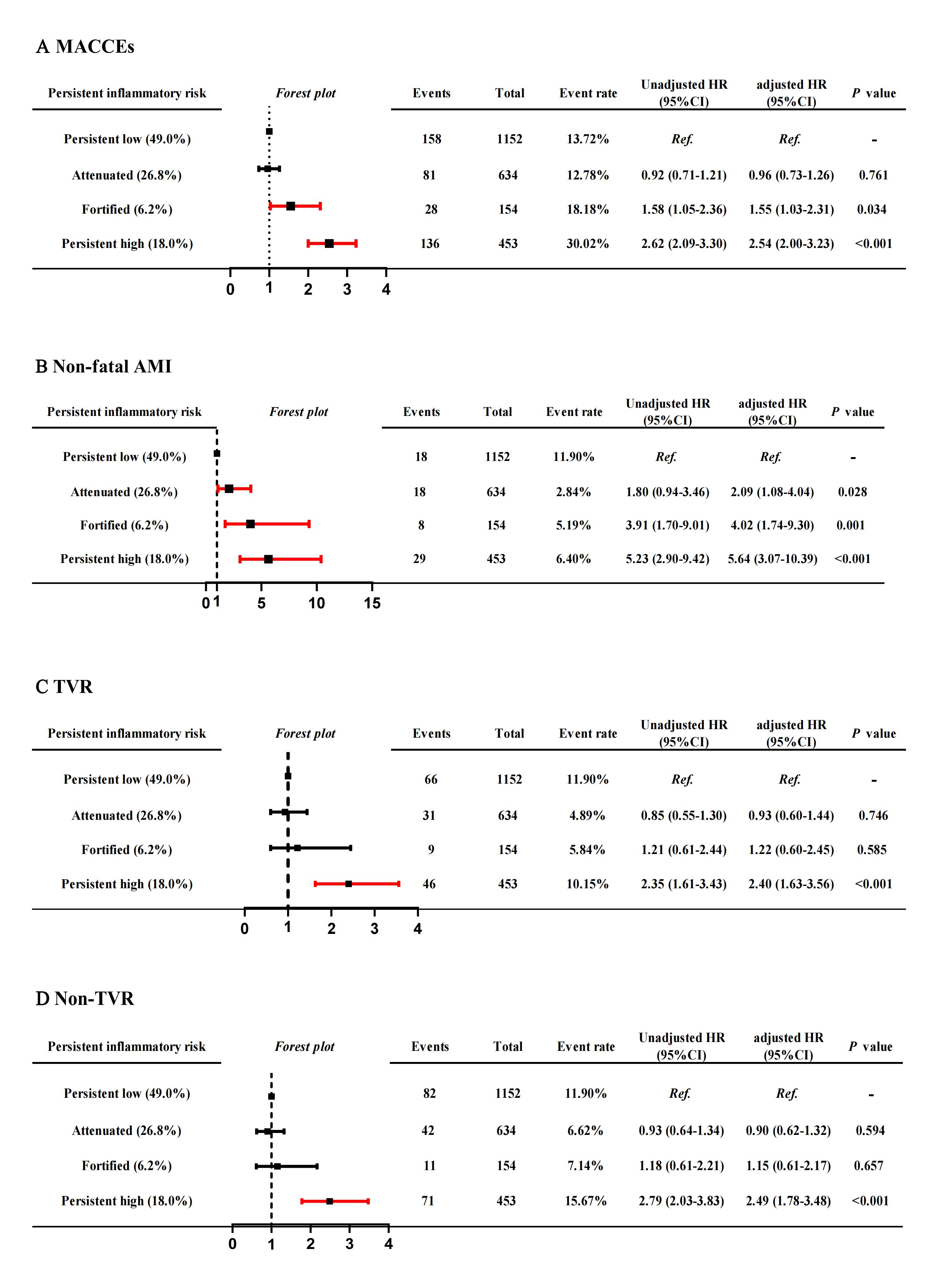
The mean age of the enrolled patients was 58.5 ± 10.32 years. More than a half (68.4%) were presented with acute coronary syndrome (ACS) on admission and most of them were male (76.4%). The hsCRP and LDL-C level were all significantly decreased from 1.7 (IQR: 0.9 - 4.2) mg/L and 2.4 ± 0.82 mmol/L at admission to 1.1 (IQR: 0.6 - 1.97) mg/L and 1.9 ± 0.60 mmol/L at follow-up (all p < 0.001). During the follow-up, 403 of the enrolled cohort (17.0%) experienced MACCEs. The cohort were classified as 4 groups: no RCIR (n = 806, 38.7%) , RCR only (n = 774, 37.2%), RIR only (n = 340, 9.9%) and RCIR group (n = 453, 14.2%). The prevalence of MACCEs was higher in the RCR only (15.1%), RIR only (24.1%) and RCIR (24.3%) group than no RCIR (11.7%) group (p < 0.001). Almost one-fifth of patients (18.0%) were in the persistently high inflammatory risk group and the prevalence of MACCEs was higher in the persistently high inflammatory risk (26.8%) group than in other groups (p < 0.001). A total of 45.2% of PCI-treated patients still experienced persistently high cholesterol risk despite statin treatment. However, no difference was found between groups in the prevalence of MACCEs (p = 0.455) (Figure 3). There were significant differences in the risk of MACCEs, non-fatal AMI, repeat coronary revascularization across the residual inflammatory and cholesterol risk group (all P < 0.001) (Figure 4). RIR-induced MACCEs were more likely to be associated with the increased risks of non-fatal AMI (HR 4.80, 95% CI: 2.25 to 10.26, p < 0.001), while RCR-induced MACCEs were more likely to be associated with the increased risk of repeat coronary revascularization (HR 1.69, 95%CI: 1.15 to 2.49, p = 0.007) (Figure 4). Persistent high inflammatory risk was significantly correlated with higher incidence of MACCEs (adjusted HR 2.02, 95%CI 1.59-2.55, p < 0.001) (Figure 5). Besides, the serial measurements of hsCRP seemed to produce more predictive value for MACCEs than the single measurement (Persistent high inflammatory risk: adjusted HR 2.11 vs. baseline high inflammatory risk: adjusted HR 1.40 vs. follow-up high inflammatory risk: adjusted HR 1.92).
Conclusion
The inflammatory criterium for hsCRP level should be lower in East Asian patients than their Western counterparts, with a cutoff value of 1.56 mg/L in current study. Intensified lipid-lowering strategies is still needed in current clinical practice. RIR and RCR could be a major determinant for recurrent vascular events while hsCRP seemed to be a stronger predictor than LDL-C after taking statins in PCI-treated patients. Serial measurement of inflammatory indicators produces more prognostic value than the single measurement.


