Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP A-037
De Novo Coronary Lesions in Dialysis Patients: Percutaneous Coronary Intervention With Drug-Eluting Stents vs. Drug-Coated Balloons
By I Gede Sumantra, Paula Mota
Presenter
I Gede Sumantra
Authors
I Gede Sumantra1, Paula Mota2
Affiliation
Bandung Adventist Hospital, Indonesia1, Gleneagles JPMC, Brunei Darussalam2
View Study Report
TCTAP A-037
DES/BRS/DCB
De Novo Coronary Lesions in Dialysis Patients: Percutaneous Coronary Intervention With Drug-Eluting Stents vs. Drug-Coated Balloons
I Gede Sumantra1, Paula Mota2
Bandung Adventist Hospital, Indonesia1, Gleneagles JPMC, Brunei Darussalam2
Background
Background
Methods
Methods
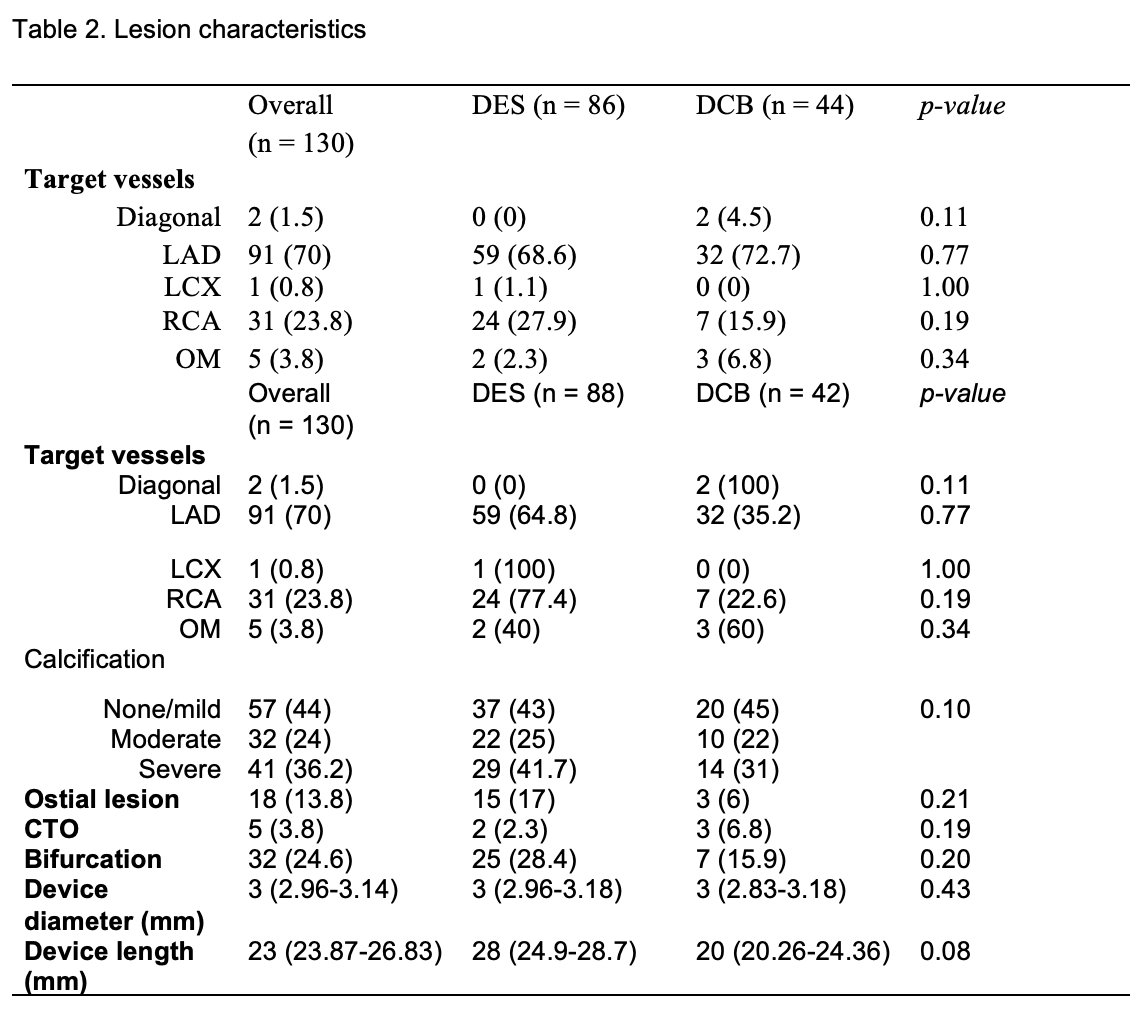
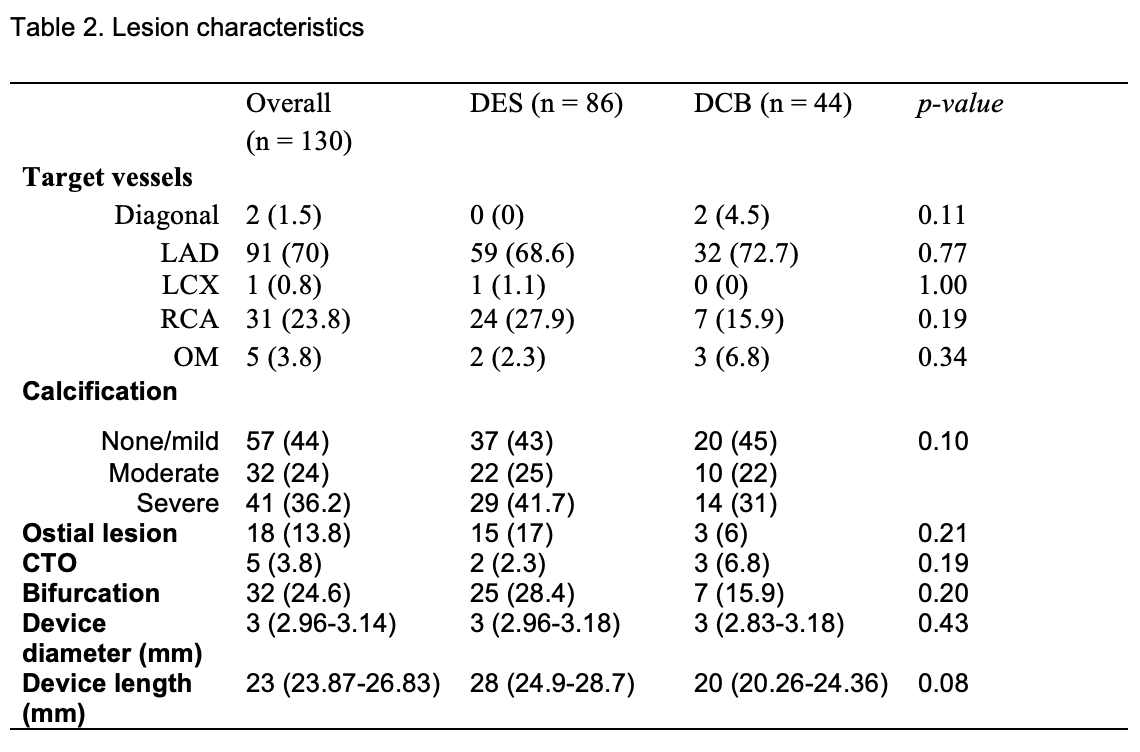
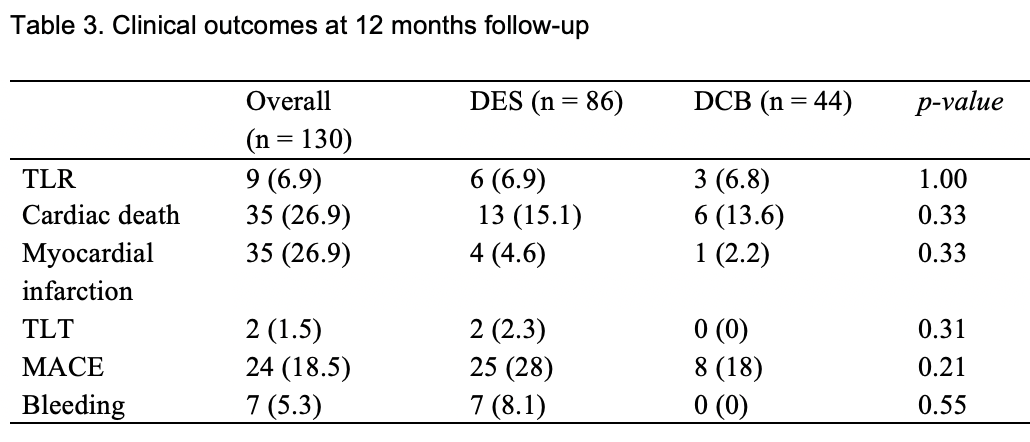
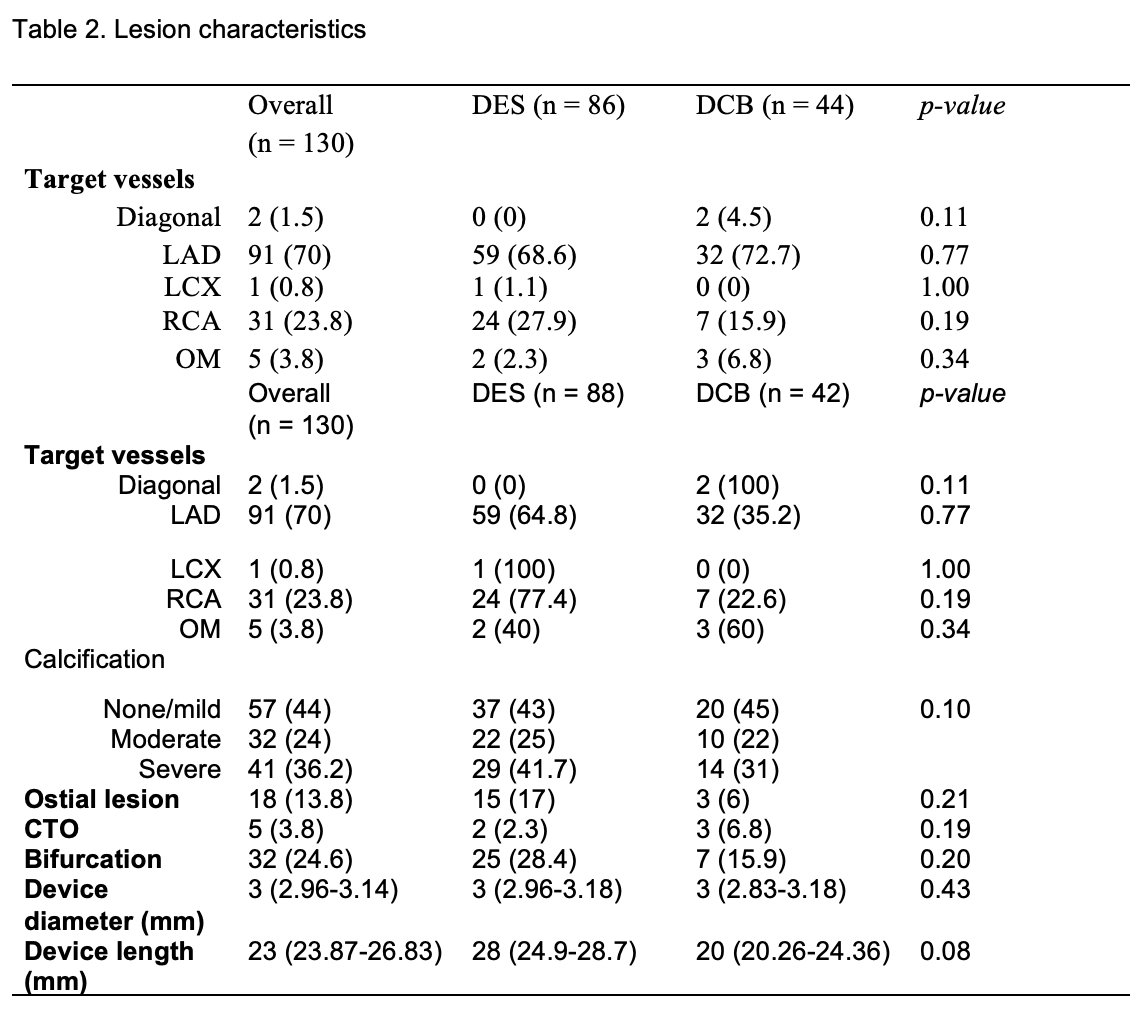
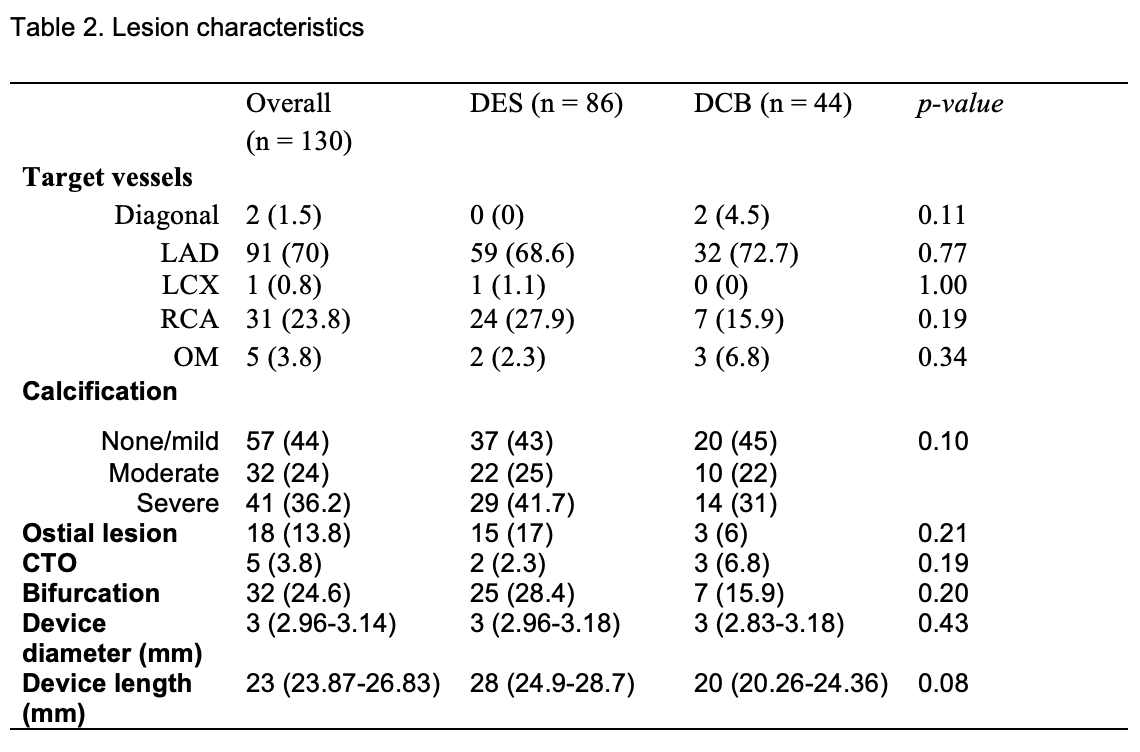
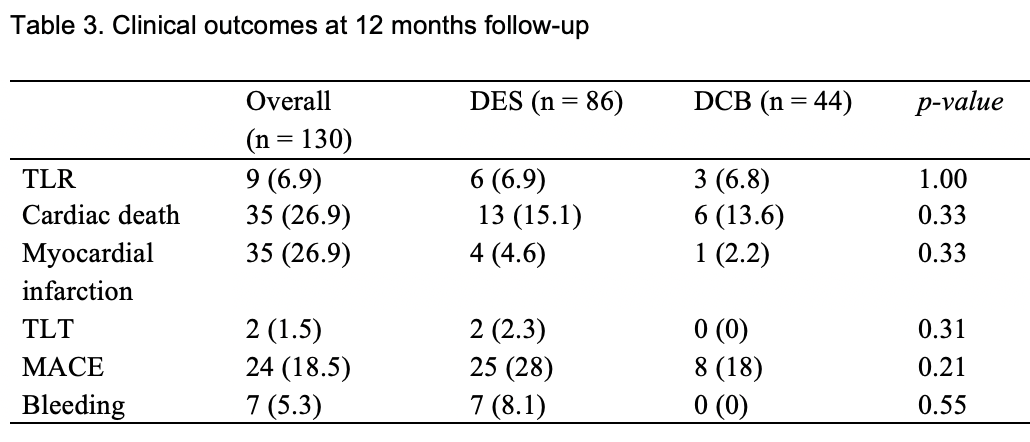
Results
Results
Conclusion
Conclusion


