Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP A-059
Long-Term Prognostic Implications of Residual Atherothrombotic Cardiovascular Risks During Guideline-Directed Medical Therapy After Percutaneous Coronary Intervention
By Young-Hoon Jeong
Presenter
Young-Hoon Jeong
Authors
Young-Hoon Jeong1
Affiliation
Gwangmyeong Hospital, Korea (Republic of)1
View Study Report
TCTAP A-059
Pharmacotherapy (Coronary)
Long-Term Prognostic Implications of Residual Atherothrombotic Cardiovascular Risks During Guideline-Directed Medical Therapy After Percutaneous Coronary Intervention
Young-Hoon Jeong1
Gwangmyeong Hospital, Korea (Republic of)1
Background
Despite current guideline-directed medical therapy (GDMT),atherothrombotic events occur in a substantial proportion of patients with high-riskcoronary artery disease (CAD).
Methods
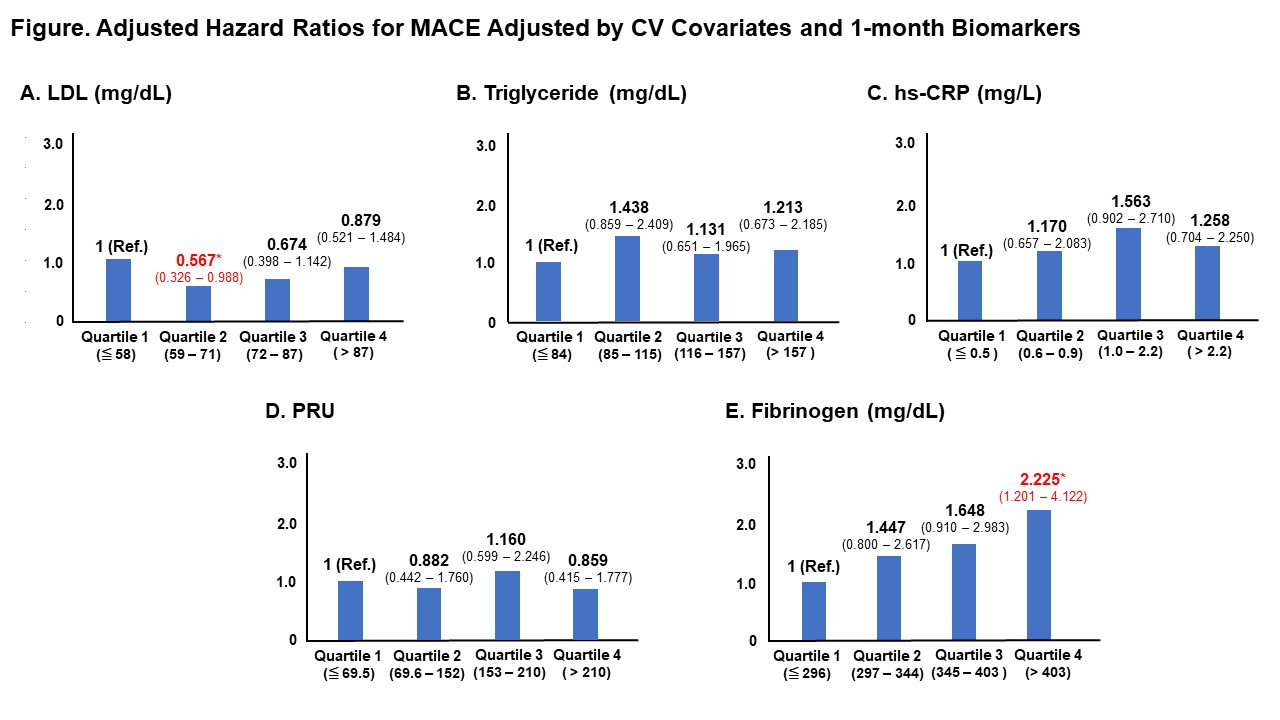
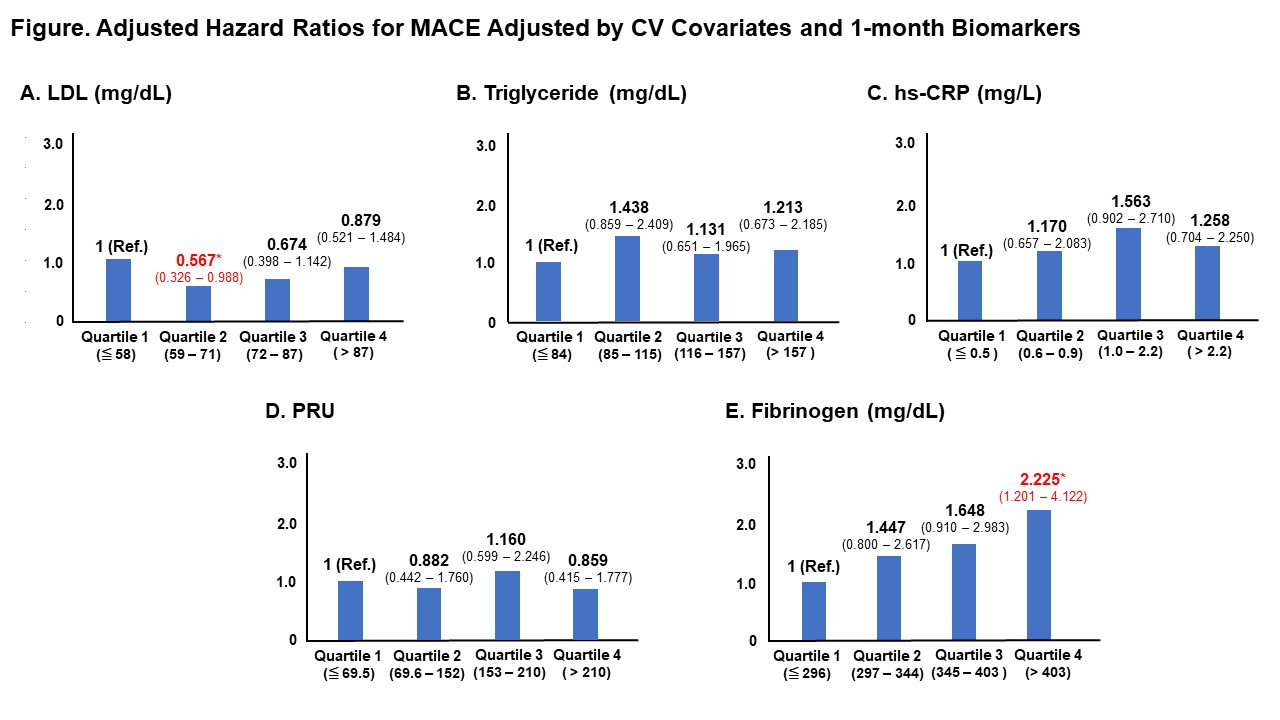
Biomarkers were measured on-admission and after 1 month of GDMT following PCI (n=2,789), which included lipid phenotype (low-density lipoprotein [LDL]-cholesterol and triglyceride) , inflammation (high-sensitivity C-reactive protein [hs-CRP]), platelet reactivity (P2Y12 reaction unit [PRU] measured by VerifyNow) and coagulation (fibrinogen). The primary endpoint was major adverse cardiovascular events (MACEs), which was a composite cardiovascular death, myocardial infarction, or stroke up to 4 years.
Results
Biomarker levels decreased significantly (all P values ≤ 0.001), except for fibrinogen levels (329±86 vs. 359±92 mg/dL; P<0.001). Covariate-adjusted hazard ratios for the lowest to highest quartiles were 1.00 (95% confidence interval [CI], referent), 1.37 (0.78–2.41), 1.89 (1.11–3.21), and 1.71 (1.01–2.91; P<0.001) for 1-month hs-CRP, and 1.00 (referent), 1.49 (0.83–2.67), 1.83 (1.03–3.26), and 2.47 (1.40–4.36; P<0.001) for 1-month fibrinogen. After adjustment with covariates and biomarkers, 1-month fibrinogen level was the only major determinant biomarker of MACE according to quartiles (1.00 [referent], 1.45 [0.80–2.62], 1.65 [0.91–2.98], and 2.23 [1.20–4.12]; P<0.001). The hs-CRP and fibrinogen levels at 1 month showed a modest correlation (r=0.426; P<0.001).
Conclusion
Fibrinogen level measured 1 month is a powerful independent predictor of long-term residual risk in PCI-treated patients receiving GDMT. The latter biomarker may serve as an indicator of the individuals who may benefit from adjunctive anticoagulant therapy beyond the scope of GDMT.


