Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP A-053
Predictive Value of Residual Vessel Fractional Flow Reserve for Optimizing Coronary Physiology Post-Revascularization
By Wei-Ting Sung, Chun-Chin Chang, Po-Hsun Huang
Presenter
Wei-Ting Sung
Authors
Wei-Ting Sung1, Chun-Chin Chang1, Po-Hsun Huang1
Affiliation
Taipei Veteran General Hospital, Taiwan1
View Study Report
TCTAP A-053
FFR
Predictive Value of Residual Vessel Fractional Flow Reserve for Optimizing Coronary Physiology Post-Revascularization
Wei-Ting Sung1, Chun-Chin Chang1, Po-Hsun Huang1
Taipei Veteran General Hospital, Taiwan1
Background
Vessel fractional flow reserve (vFFR) is a non-invasive modality to assess coronary physiology based on coronary angiograms. vFFR can be easily measured at baseline and post percutaneous coronary intervention (PCI). In addition, residual vFFR, a feature designed to predict post-PCI vFFR, provides valuable insights. In this context, the aim of this study is to investigate the potential factors associated with achieving an optimal post-PCI vFFR value and to validate the correlation between residual vFFR and post-PCI vFFR.
Methods
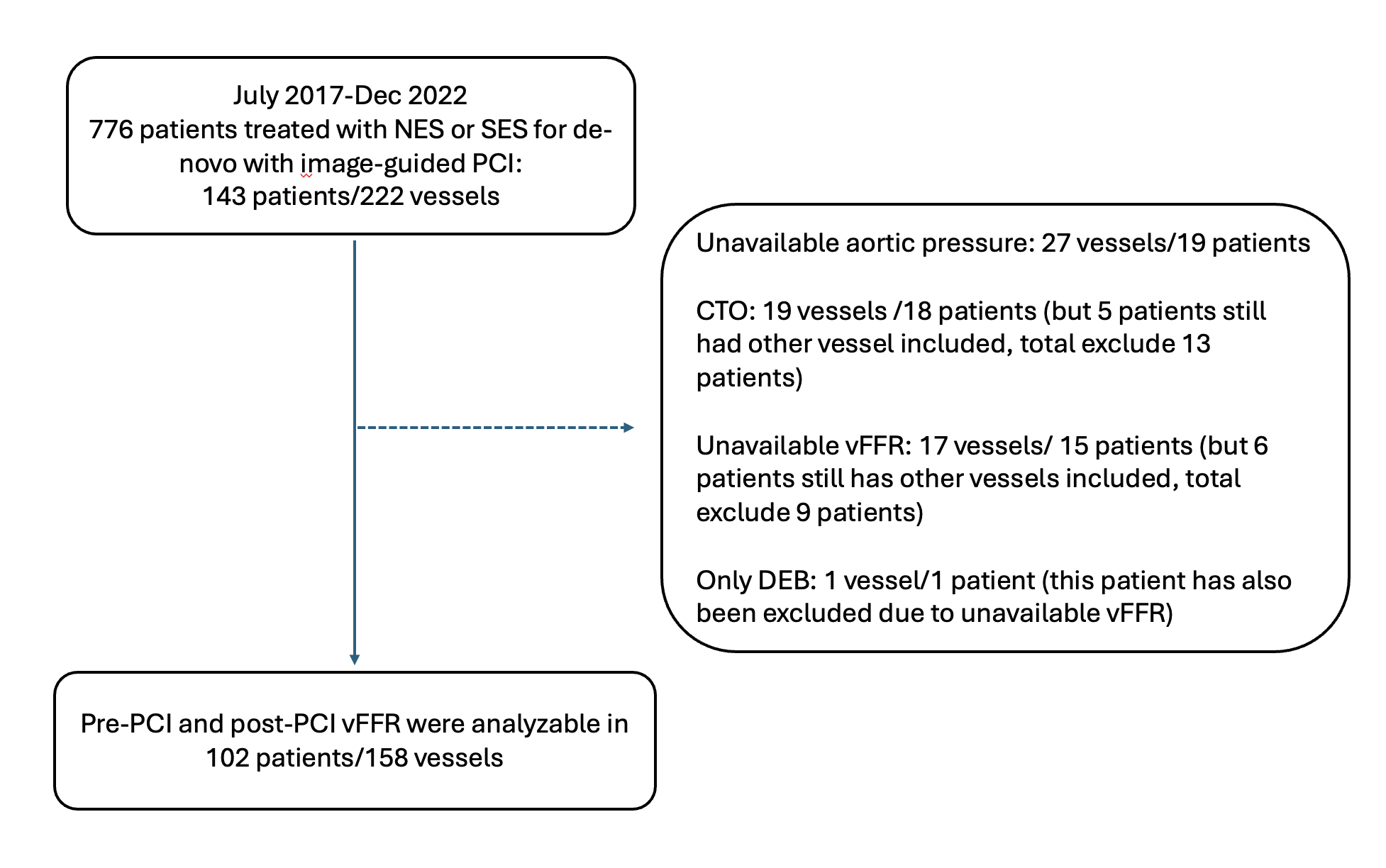
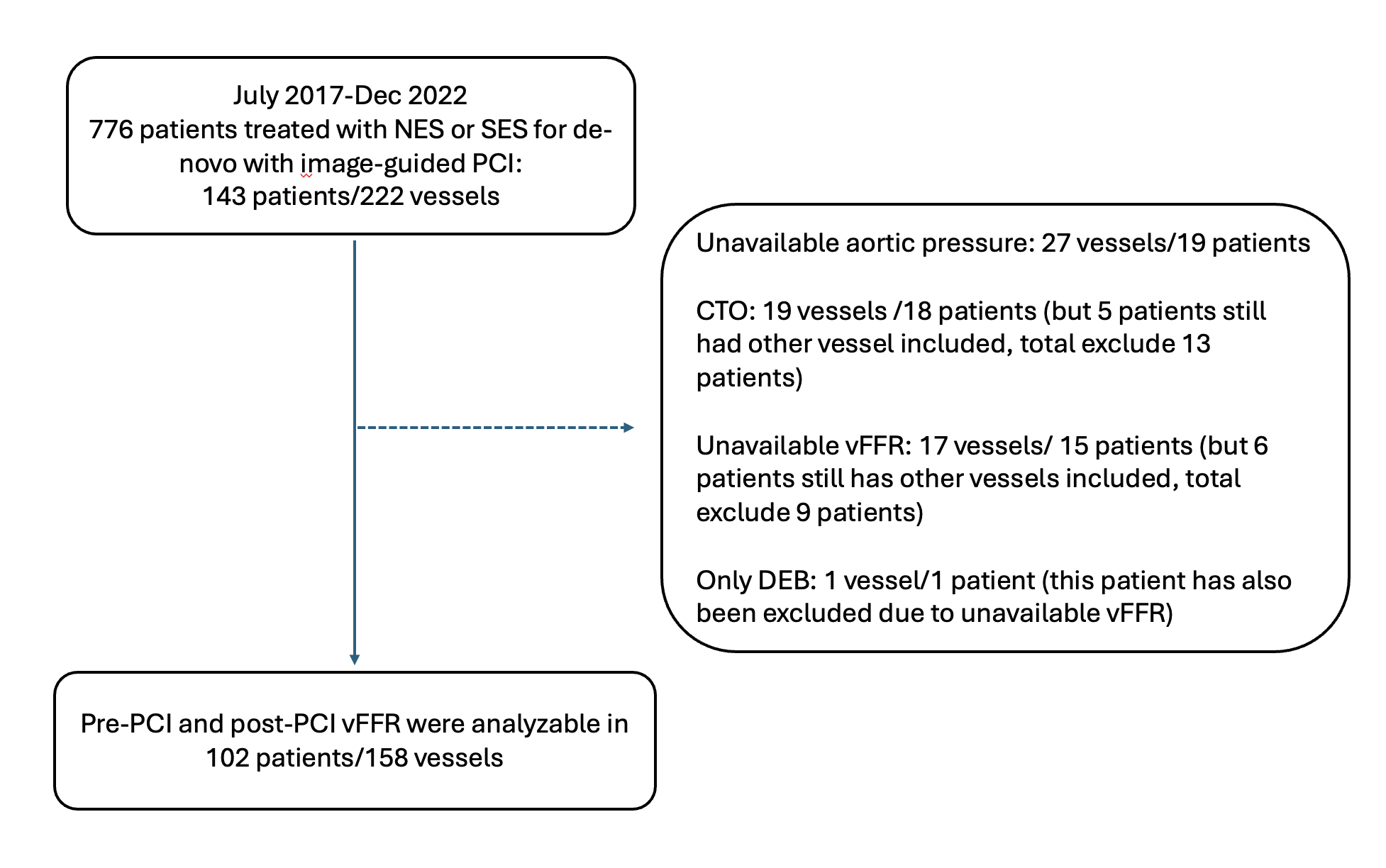
Between July 2017 to December 2022, 143 chronic coronary syndrome patients (222 vessels) undergoing imaged-guided PCI using second-generation drug-eluting stents at a single tertiary center were analyzed. Pre-PCI vFFR, residual vFFR and post-PCI vFFR were calculated retrospectively.
Results
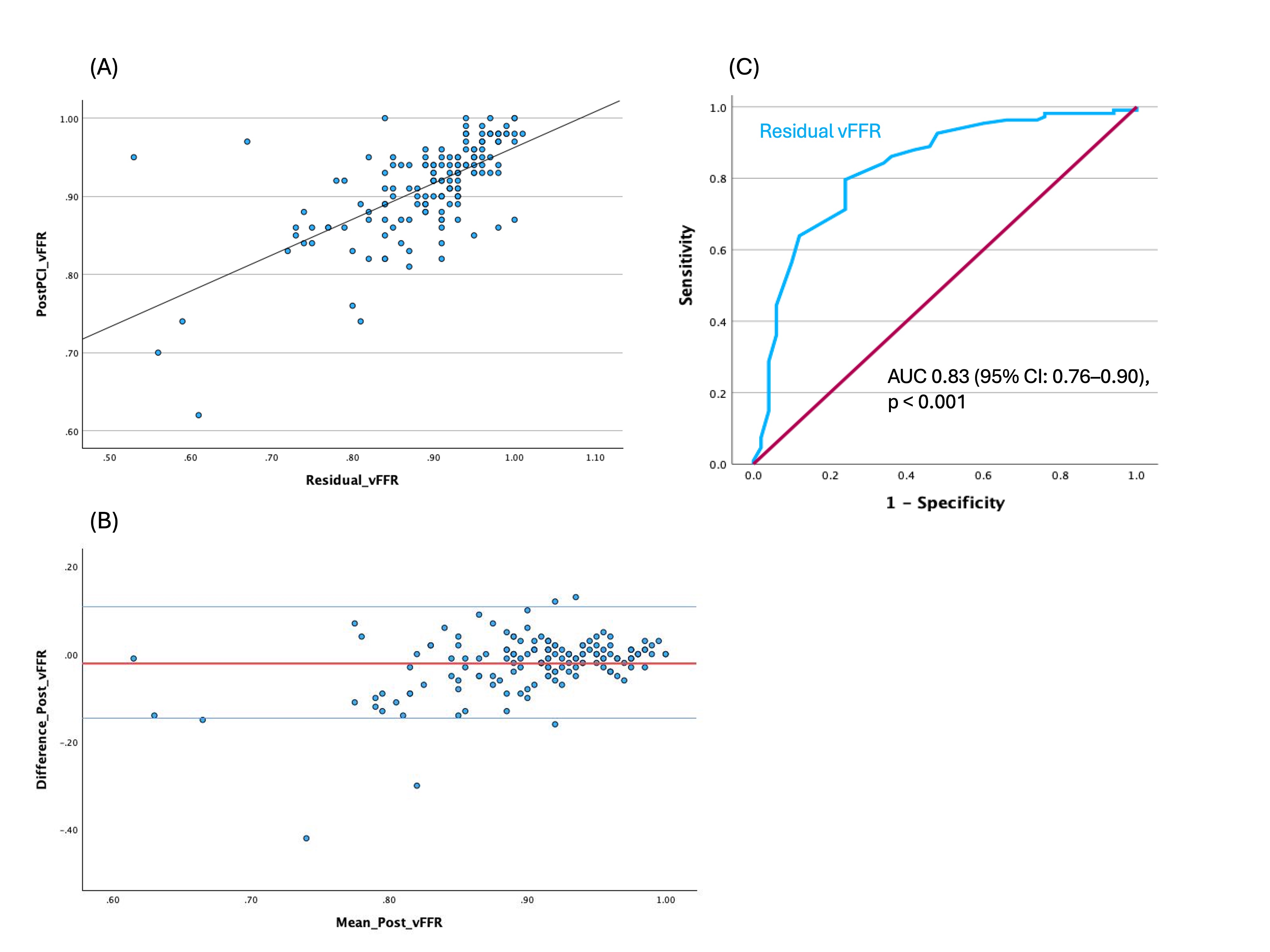
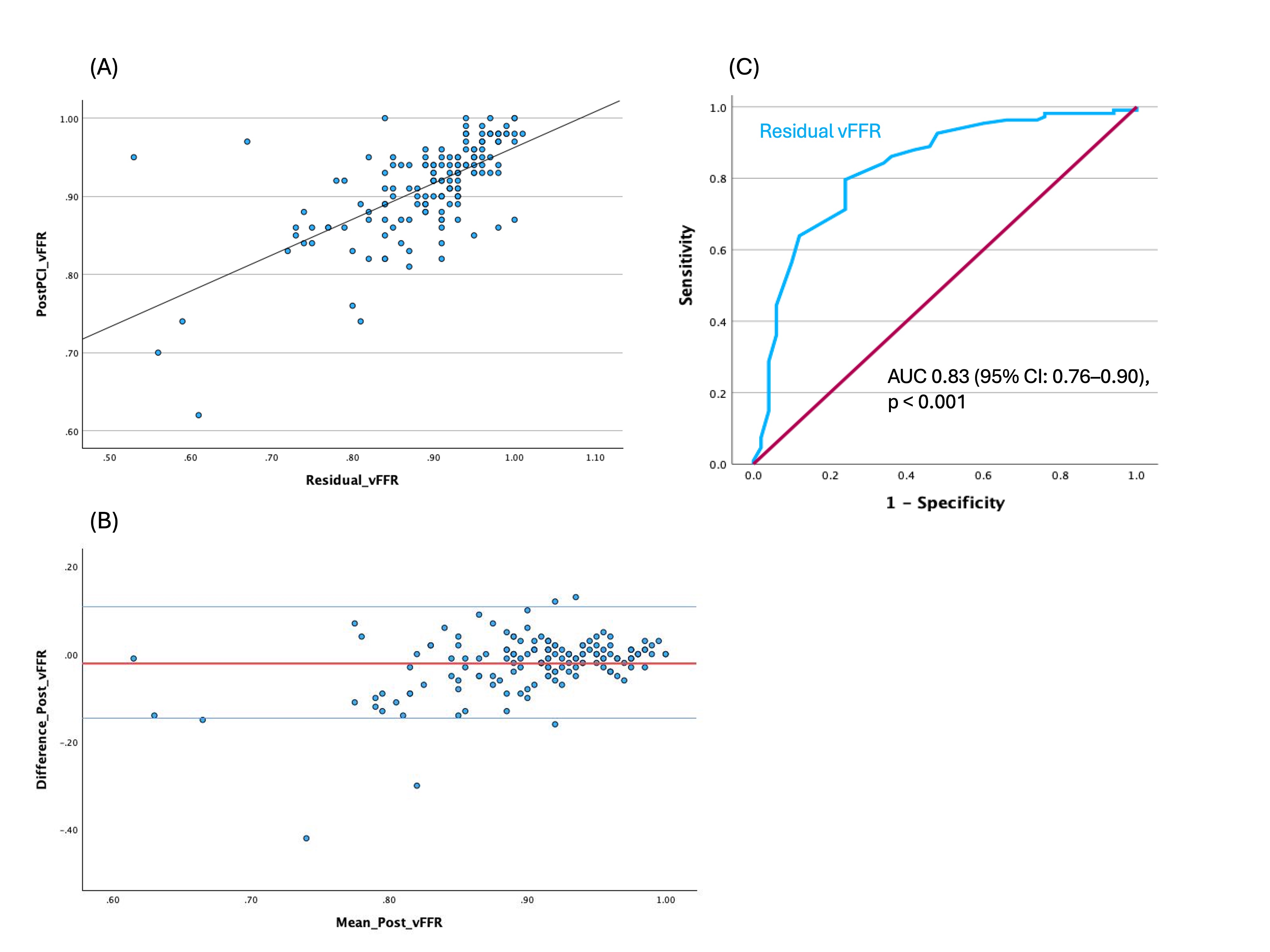
A moderate correlation was observed between residual vFFR and post-PCI vFFR (Figure 1A, r= 0.65). Receiver operating characteristic (ROC) curve analysis demonstrated that residual vFFR has good predictive value for achieving post-PCI vFFR ≥ 0.90, with an area under the curve (AUC) of 0.83 (Figure 1C, 95% confidence interval [CI]: 0.76–0.90, p < 0.001). Multivariable Cox regression analysis revealed that pre-PCI vFFR ≥ 0.80 (odds ratio [OR]: 2.959, 95% CI: 1.084-8.078, p=0.034), non-left anterior descending (LAD) lesions (OR: 4.296, 95% CI: 1.760–10.488, p = 0.001) and stent size ≥ 3.0 mm (OR: 4.226, 95% CI: 1.834-9.737, p < 0.001) were significantly associated with achieving post-PCI vFFR ≥ 0.90.
Conclusion
Residual vFFR showed good predictive value for achieving post-PCI vFFR ≥ 0.90. Non-LAD lesions, pre-PCI vFFR ≥ 0.80 and stent sizes ≥ 3 mm were associated with an optimal physiological result after revascularization.


