Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP A-032
Beyond Stent: The Value of PRECISE-DAPT Score on Bleeding Risk Assessment and Outcome Prediction in Left Main PCI
By En-Shao Liu, Yan-Ning Shih, Feng-Yu Kuo
Presenter
En-Shao Liu
Authors
En-Shao Liu1, Yan-Ning Shih1, Feng-Yu Kuo1
Affiliation
Kaohsiung Veterans General Hospital, Taiwan1
View Study Report
TCTAP A-032
Left Main
Beyond Stent: The Value of PRECISE-DAPT Score on Bleeding Risk Assessment and Outcome Prediction in Left Main PCI
En-Shao Liu1, Yan-Ning Shih1, Feng-Yu Kuo1
Kaohsiung Veterans General Hospital, Taiwan1
Background
Left main (LM) coronary artery disease (CAD) is a significant indicator of lesion severity and myocardial ischemia, carrying higher morbidity and mortality compared to other forms of obstructive CAD. With advancements in operator techniques, interventional devices, and adjunctive medications, the use of percutaneous coronary intervention (PCI) for LM disease has increased, particularly in patients at higher surgical risk, such as the elderly and those with multiple comorbidities. Studies have shown that high bleeding risk (HBR), as assessed by the Academic Research Consortium (ARC) HBR criteria, is associated with worse outcomes in these high-risk patients. Additionally, the PRECISE-DAPT (PREdicting bleeding Complications In patients undergoing Stent implantation and subsEquent Dual Anti Platelet Therapy) score has been introduced as a standardized tool to evaluate bleeding risks and to guide the optimal duration of dual antiplatelet therapy (DAPT) after PCI. Compared to the ARC-HBR criteria, the PRECISE-DAPT score offers the advantage of simplicity and higher specificity. However, the predictive value of the PRECISE-DAPT score in LM PCI remained unclear. This study aimed to assess the impact of HBR, as evaluated by the PRECISE-DAPT score, on outcomes in patients undergoing LM PCI.
Methods
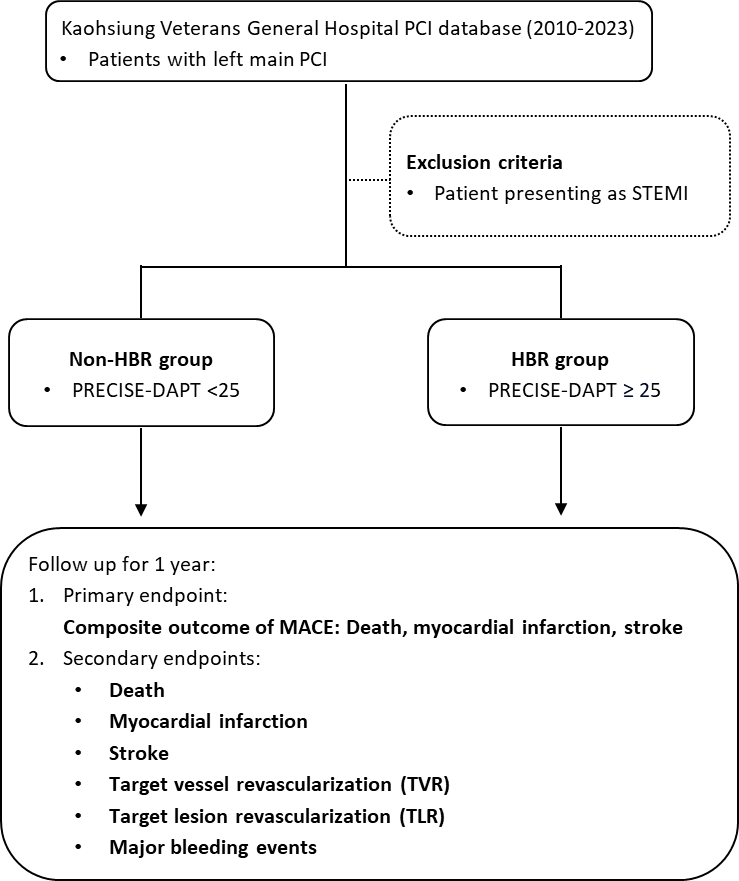
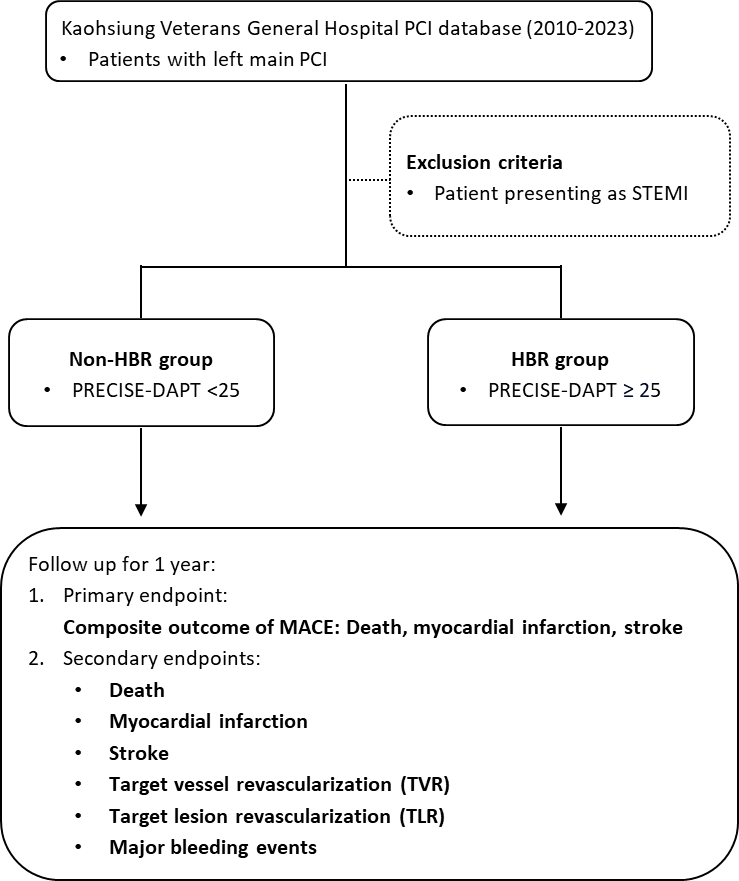
This retrospective study was conducted at a tertiary medical center in Taiwan, including consecutive patients who underwent LM PCI between January 2010 and September 2023. Patients with ST-segment elevation myocardial infarction (STEMI) were excluded (Figure 1). PCI procedures followed standard protocols, leaving the treatment strategy to the operator's discretion. The duration and regimen of dual antiplatelet therapy (DAPT) following PCI was based on the patient's condition and the attending physician’s judgment. Baseline characteristics and angiography data were gathered from electronic medical records and the catheterization lab database. The PRECISE-DAPT score was calculated using an online calculator, and laboratory values (hemoglobin, white blood cell count, and creatinine clearance) were based on the last available data before PCI. A history of bleeding was defined as either one of the following criteria: (1) hemorrhage-related diagnosis at the emergency room or prior hospitalization, (2) blood transfusion with clinical signs or symptoms of bleeding, or (3) endoscopic or imaging evidence of bleeding with symptoms. Patients were classified into the HBR group (PRECISE-DAPT score ≥25) and the non-HBR group (PRECISE-DAPT score <25). Patients were followed for one year. The primary ischemic endpoint was major adverse cardiovascular events (MACE), which included all-cause death, myocardial infarction, or stroke. Target lesion revascularization (TLR) and target vessel revascularization (TVR) were also assessed. Major bleeding was defined as bleeding events requiring blood transfusion or hospitalization. Statistical comparisons of continuous variables were made using the Student’s t-test or Wilcoxon test, while categorical variables were analyzed using the Chi-square or Fisher’s exact test. Kaplan-Meier and log-rank tests were used to compare cumulative incidence between the two groups. Multivariable Cox regression analysis estimated the hazard ratio for events associated with the PRECISE-DAPT score, and discriminative ability was assessed by Harrell’s C-index. Statistical analyses were performed using SPSS (version 22.0) and R software (version 4.4.1).
Results
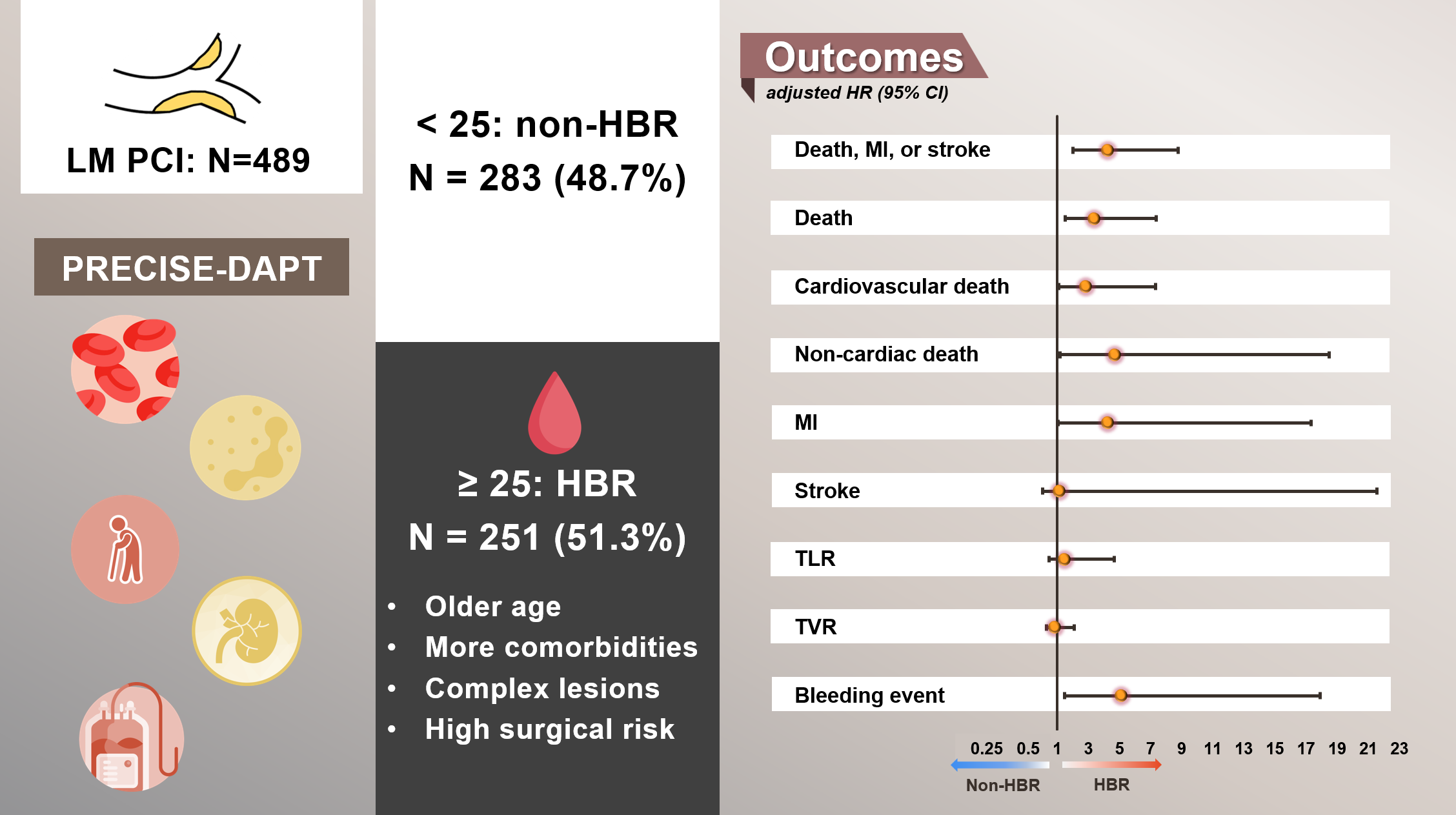
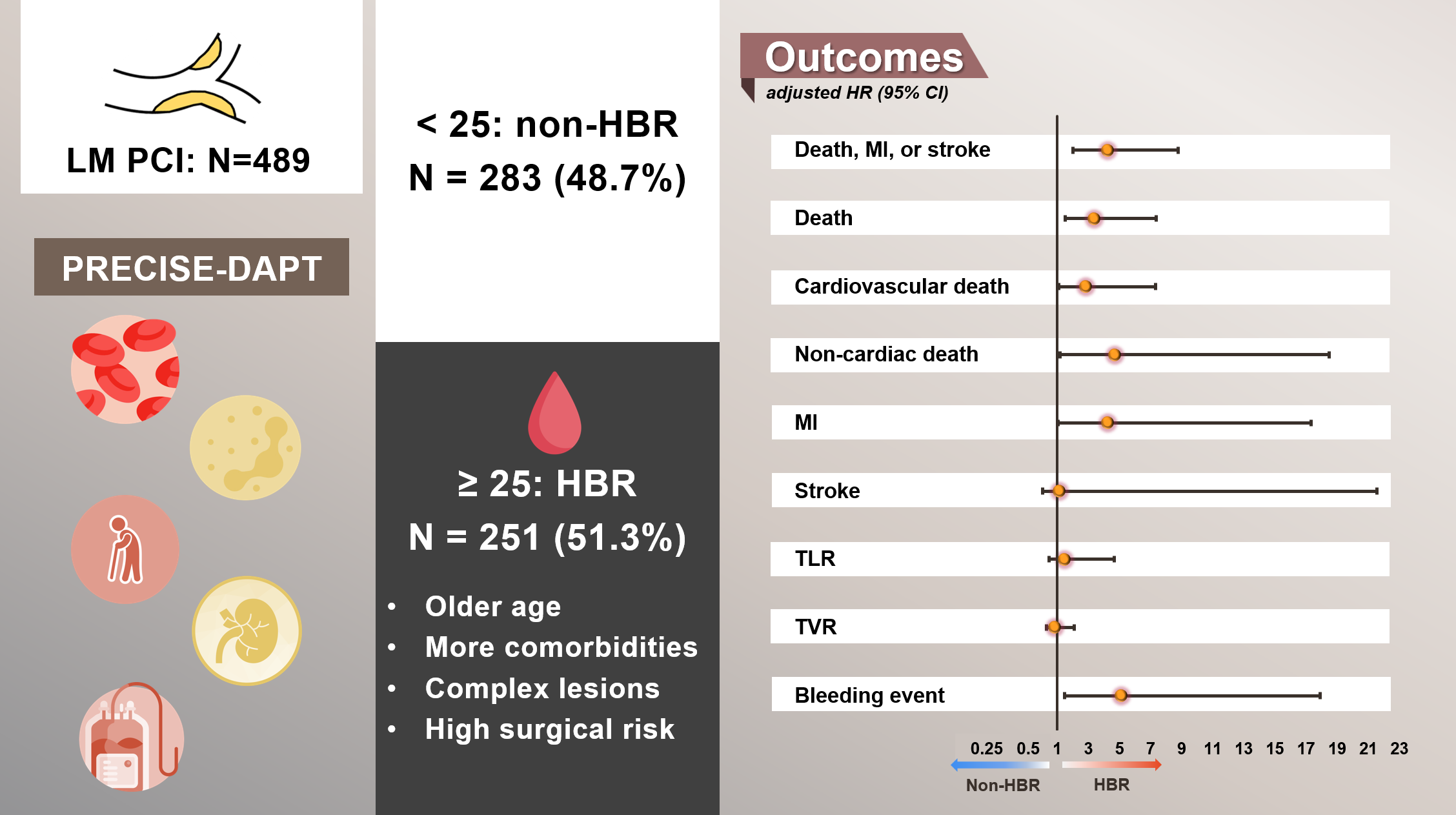
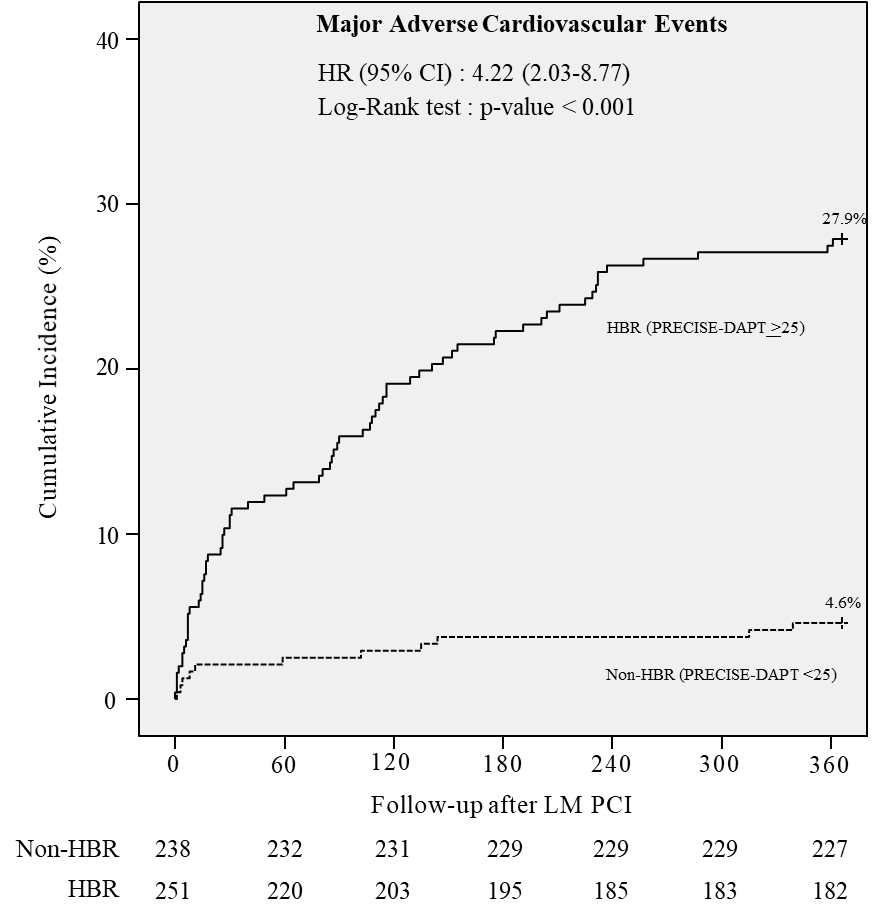
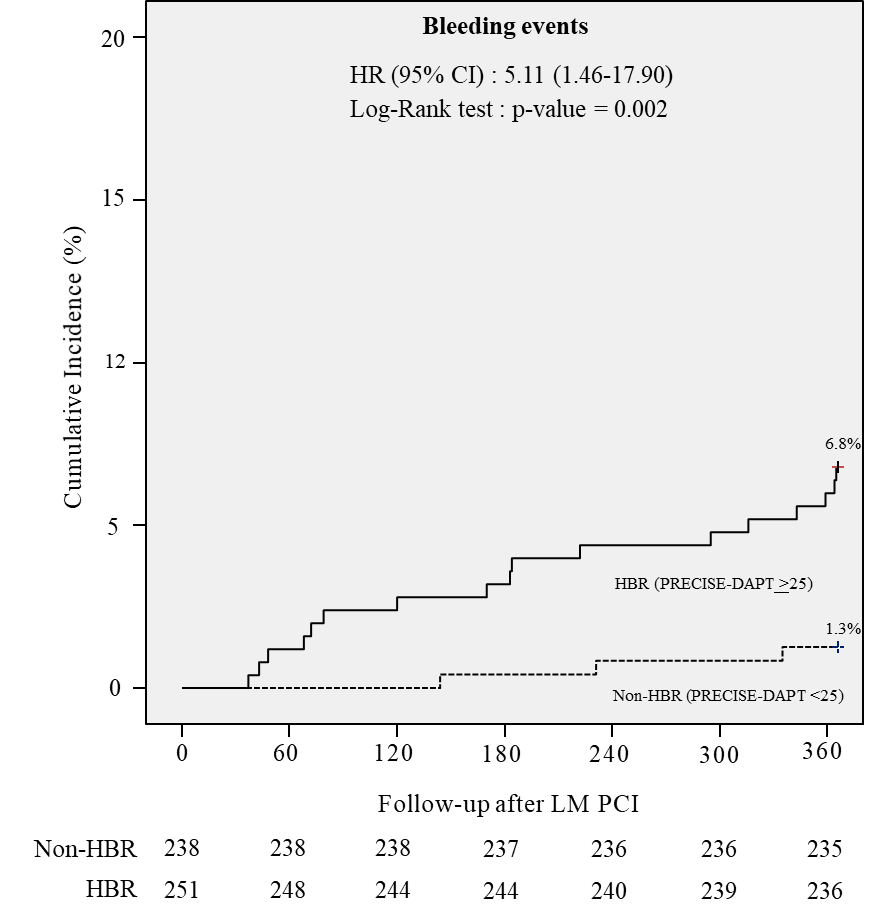
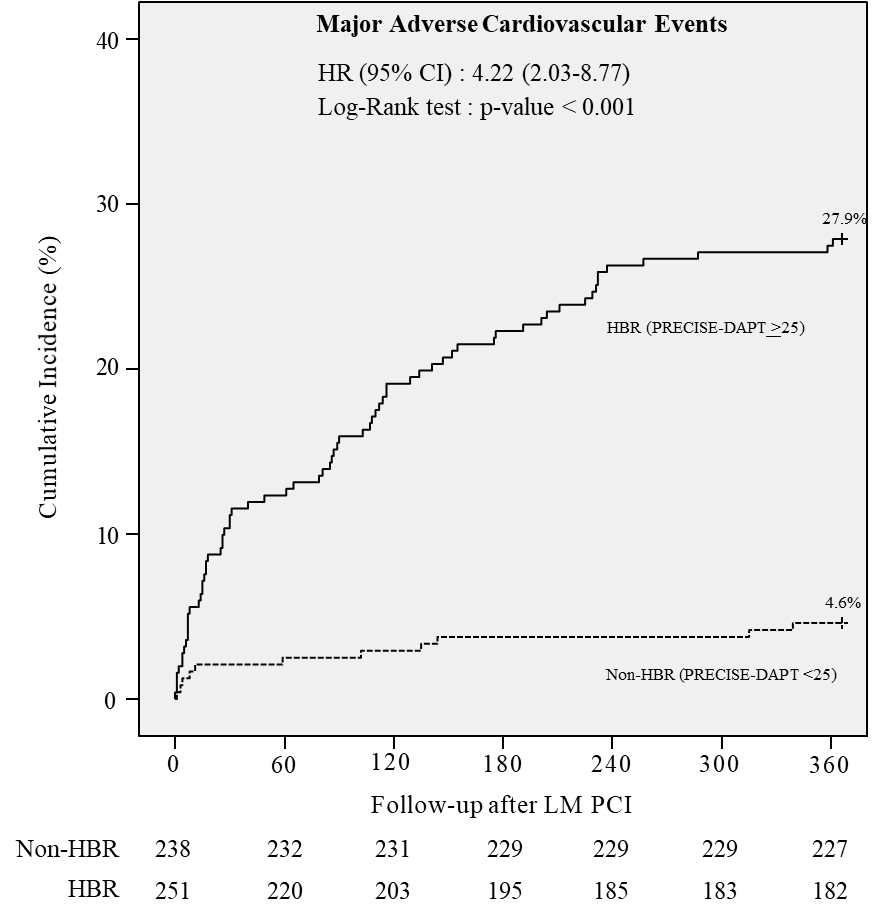
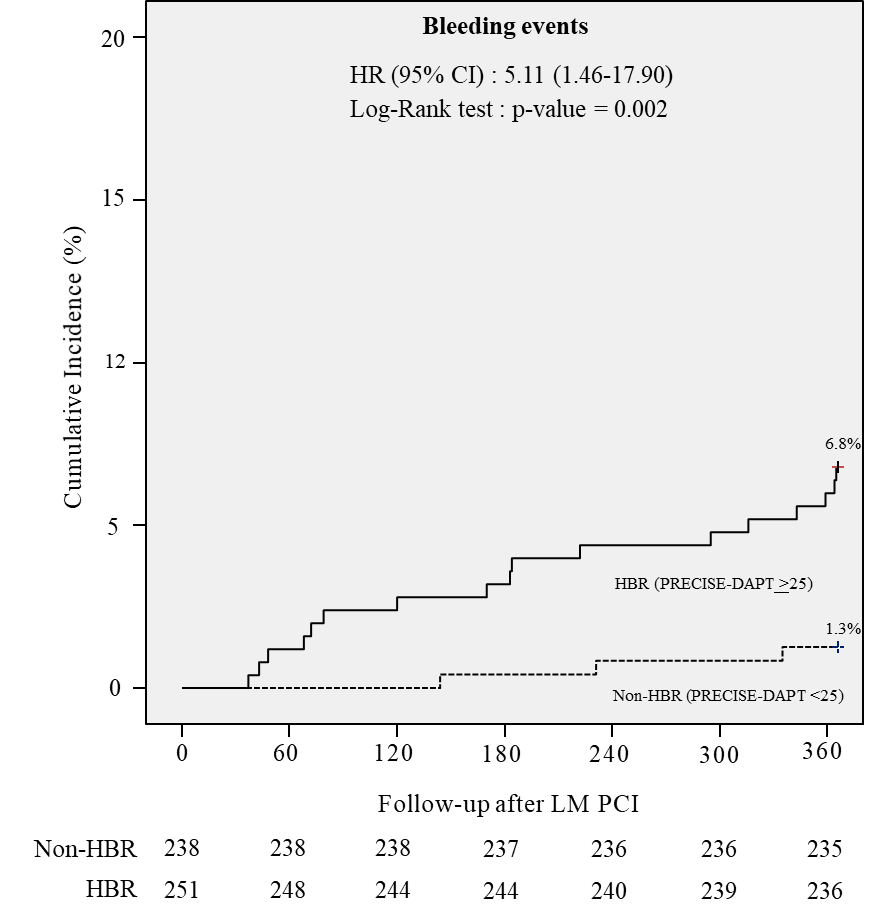
A total of 489 patients who received LM PCI were identified at our institution, and more than half of the patients (n=251, 51.3%) were classified as HBR group according to the PRECISE-DAPT score. Compared with the non-HBR group, patients at HBR were older and carried a higher proportion of comorbidities, including diabetes mellitus, hypertension, chronic kidney disease, heart failure, old cerebrovascular accident, chronic obstructive pulmonary disease, and bleeding history. Among these LM PCI patients, about one-third presented with acute coronary syndromes (n=174, 35.6%), with a greater distribution of NSTEMI in the HBR group. Patients at HBR also presented more complex coronary anatomy with a higher SYNTAX score on angiography. Intravascular imaging was performed in over half of the patients who underwent LM PCI, and there was no significant difference between the two groups. The HBR group had longer stays in the intensive care unit (ICU) and hospitalization. Clinical outcomes at one year revealed a higher MACE rate in the HBR group compared with the non-HBR group (27.9% v.s. 4.6%; HR: 6.86; 95% confidence interval (CI): 3.63-12.95). This result was mainly driven by death (21.9% v.s. 4.2%; HR: 5.74; 95% CI: 2.92-11.25) and myocardial infarction (7.2% v.s. 1.3%; HR: 5.86; 95% CI: 1.73-19.88). The one-year mortality was significantly higher in the HBR group, regardless of the cause of death. TLR and TVR revealed no difference between the two groups. The HBR group was associated with the risks of future major bleeding after LM PCI (6.8% v.s. 1.3%; HR: 5.53; 95% CI: 1.62-18.88). The time-to-event curves showed significant differences for MACE (Figure 2; log-rank p-value <0.001) and major bleeding (Figure 3; log-rank p-value=0.002) between HBR and non-HBR groups through one year. Multivariate Cox multivariable regression analysis revealed that the PRECISE-DAPT score ≥25 remained the only significant predictor of MACE (HR: 4.22; 95% CI: 2.03-8.77) and bleeding (HR: 5.11; 95% CI: 1.46-17.90). The discrimination ability of PRECISE-DAPT was 0.74 for MACE and 0.68 for major bleeding by Harrell’s C-index separately.
Conclusion
The research highlighted the impact of HBR, defined by the PRECISE-DAPT score, on the clinical outcomes of patients treated with LM PCI. The prevalence of HBR in LM patients was notably higher (over 50%) compared to around 20% in general PCI patients, as reported in previous studies. The HBR group faced not only an increased risk of bleeding but also higher rates of mortality and myocardial infarction. The high proportion of intravascular imaging use (over 55% in both groups) and the absence of a significant relationship between HBR and TLR or TVR suggest that the elevated cardiovascular death and myocardial infarctions in the HBR group were likely due to baseline characteristics, such as frailty and comorbidities, rather than the procedure itself. The increased non-cardiac death in this group supports this assumption and highlights the broader implications of HBR. Compared to the previous study that used the ARC-HBR criteria to assess HBR in LM PCI outcomes, this study revealed consistent results when defining HBR using the PRECISE-DAPT score. Compared with ARC-HBR criteria, the PRECISE-DAPT score includes only five items for calculation, which makes it a more straightforward tool for risk stratification. The higher prevalence of intravascular imaging use in this study and the inclusion of a broader patient population, such as those with NSTEMI or prior CABG, further supported the value of the PRECISE-DAPT score. Harrell's C-index indicated that the PRECISE-DAPT score could effectively identify high-risk LM PCI patients, regardless of assessing future ischemic events or bleeding. To our knowledge, this is the first study to utilize the PRECISE-DAPT score for HBR classification and outcome evaluations in LM PCI patients. Our results validate the PRECISE-DAPT as an effective tool for bleeding risk categorization and prognosis prediction in this patient population. (Figure 4.)