Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP A-045
Percutaneous Coronary Intervention (PCI) After Return of Spontaneous Circulation (ROSC) Following In-Hospital Cardiac Arrest With Evidence of Acute Myocardial Infarction & Its Neurological Outcome
By Md Moniruzzaman, Kazi Shamim Al Mamun, Md Nahid Hasan, Md Saiful Islam, Md Afzalur Rahman
Presenter
Md Moniruzzaman
Authors
Md Moniruzzaman1, Kazi Shamim Al Mamun2, Md Nahid Hasan1, Md Saiful Islam3, Md Afzalur Rahman1
Affiliation
Sheikh Fazilatunnessa Mujib Memorial KPJ Specialized Hospital, Bangladesh1, Chattagram Medical College Hospital, Bangladesh2, Khwaja Yunus Ali Medical College & Hospital, Bangladesh3
View Study Report
TCTAP A-045
ACS/AMI
Percutaneous Coronary Intervention (PCI) After Return of Spontaneous Circulation (ROSC) Following In-Hospital Cardiac Arrest With Evidence of Acute Myocardial Infarction & Its Neurological Outcome
Md Moniruzzaman1, Kazi Shamim Al Mamun2, Md Nahid Hasan1, Md Saiful Islam3, Md Afzalur Rahman1
Sheikh Fazilatunnessa Mujib Memorial KPJ Specialized Hospital, Bangladesh1, Chattagram Medical College Hospital, Bangladesh2, Khwaja Yunus Ali Medical College & Hospital, Bangladesh3
Background
AcuteMyocardial Infarction (AMI) is a major cause of cardiac arrest worldwide.Immediate coronary angiography and percutaneous coronary intervention (PCI) maybe considered in patients who have been successfully resuscitated after cardiacarrest with pre or post-cardiac arrest documentary evidence of acute myocardialinfarction. This study aimed to evaluate the effects of PCI on in-hospitalmortality & neurological outcomes after gaining Return of Spontaneous Circulation(ROSC) following cardiac arrest due to AMI.
Methods
Inthis prospective observational cohort study, we have randomly assigned 36patients from August 2021 to November 2023 who had a cardiac arrest either atEmergency or In Patient Department during ongoing care with evidence of acutemyocardial infarction.
Results
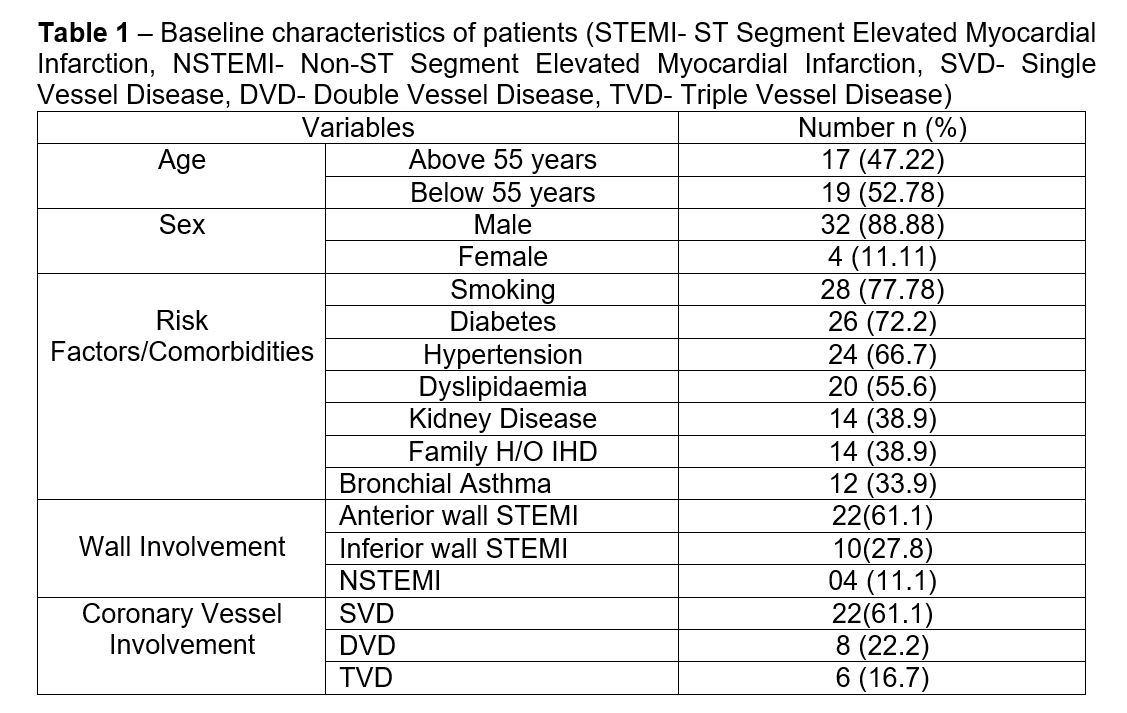
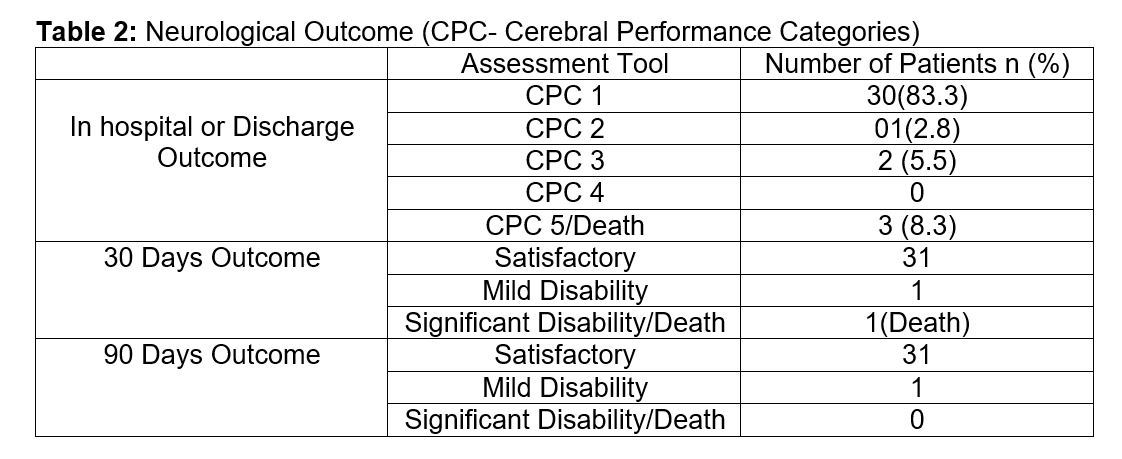
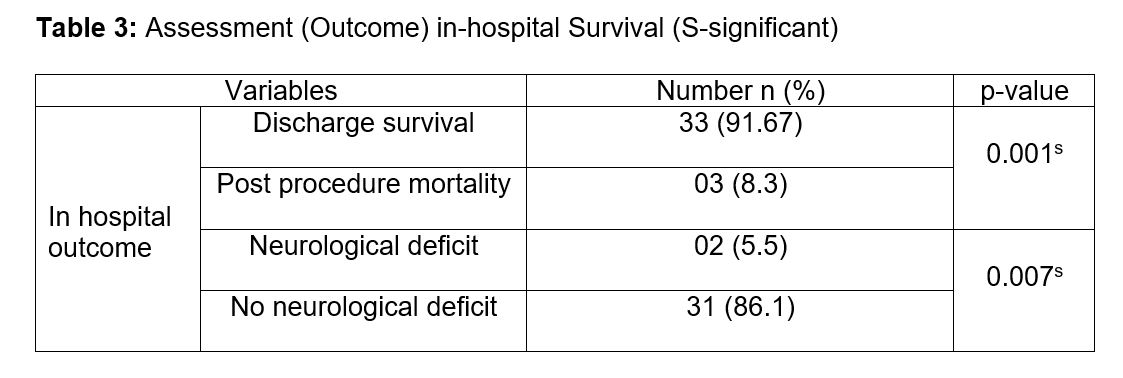
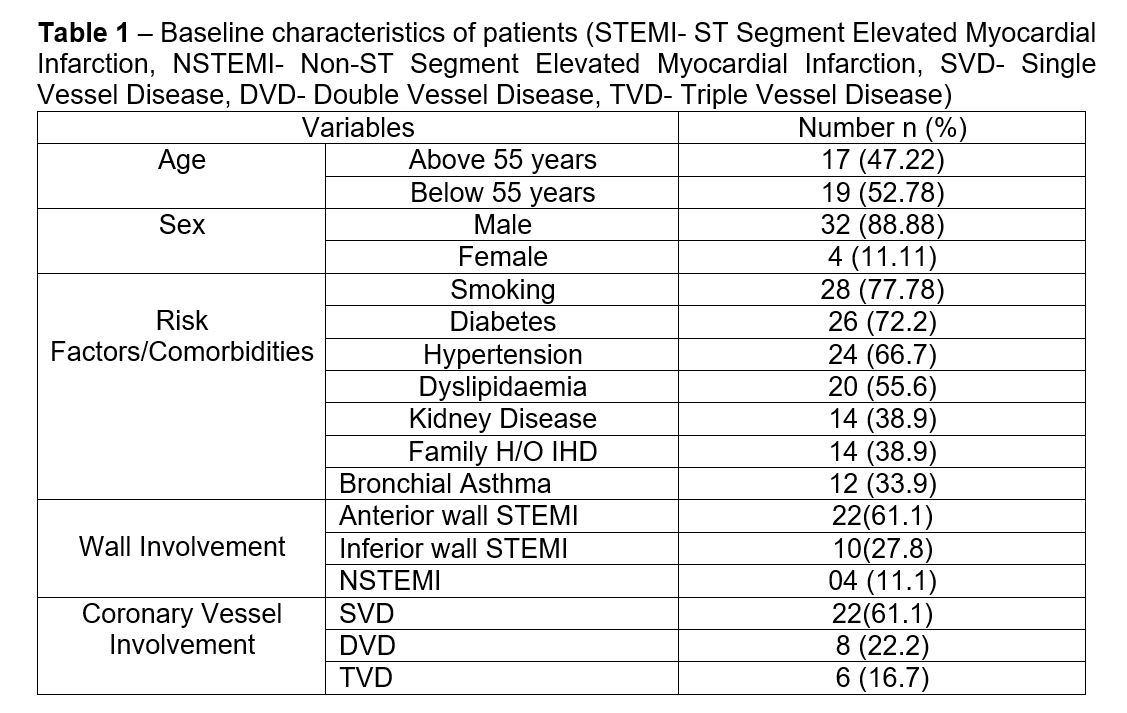
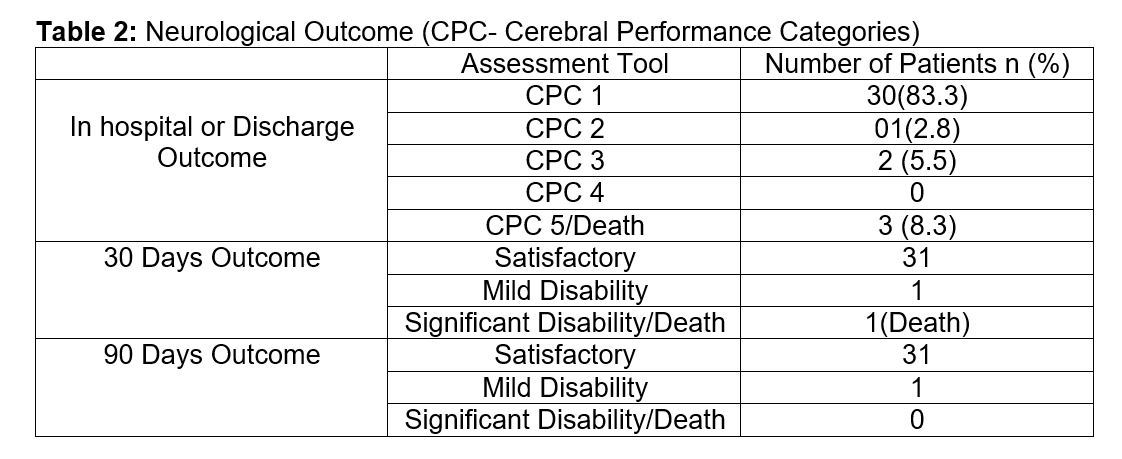
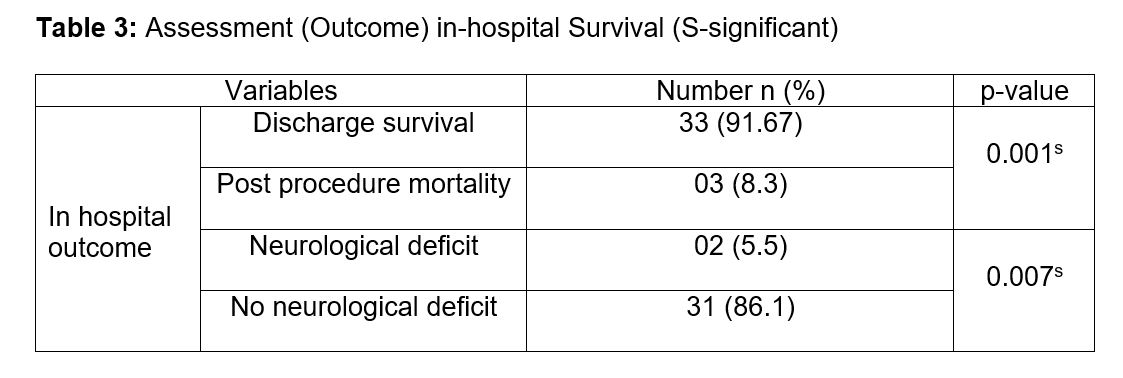
Themean age of the patients was 55.39±10.89 years. Among them male was32(88.88%), female was 4(11.11%). Smoking (77.78%) was the most common riskfactor followed by Diabetes mellitus (72.2%), Hypertension (66.7%),Dyslipidemia (55.6%), positive family history of IHD (38.9%), chronic kidneydisease (38.9%) & Bronchial Asthma (33.9%) patients. Among all patients,22(61.1%) patients had Acute STEMI (Anterior). 10(27.8%) patients had AcuteSTEMI (Inferior) & 4 (11.1%) had acute NSTEMI. SVD was found in 22(61.1%)patients, DVD in 08(22.2%) patients and TVD in 6(16.7%) patients. (Table-1)All 36 patients underwent immediate Coronary Angiogram (CAG) after ROSCfollowed by newer generation Drug Eluting Stent (DES) implantation. 32 patientsgot target vessel revascularization & 4 patients got total revascularization.In all patients with CT or MRI of brain was done as per advice of Neurologist.
Conclusion
The patients who gained ROSC after cardiac arrestcaused by AMI & underwent PCI had a lower in-hospital mortality &satisfactory neurological outcomes.


