Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP A-019
Outcomes Comparison of Patients Who Underwent Rotational Atherectomy With and Without Heart Block in Thai Populations
By Wittawat Wattanasiriporn, Purish Surunchapakorn, Atthaphon Phaisitkriengkrai, Wirash Kehasukcharoen
Presenter
Wittawat Wattanasiriporn
Authors
Wittawat Wattanasiriporn1, Purish Surunchapakorn2, Atthaphon Phaisitkriengkrai2, Wirash Kehasukcharoen2
Affiliation
Rajavithi Hospital, Thailand1, Central Chest Institute of Thailand, Thailand2
View Study Report
TCTAP A-019
Adjunctive Procedures (Thrombectomy, Atherectomy, Special Balloons)
Outcomes Comparison of Patients Who Underwent Rotational Atherectomy With and Without Heart Block in Thai Populations
Wittawat Wattanasiriporn1, Purish Surunchapakorn2, Atthaphon Phaisitkriengkrai2, Wirash Kehasukcharoen2
Rajavithi Hospital, Thailand1, Central Chest Institute of Thailand, Thailand2
Background
Rotational Artherectomy (RA) a high speed rotating diamond-coated burr for percutaneous coronary intervention (PCI) of heavily calcified lesions. Atheroablative procedure increases the risk of complications including slow flow,no reflow, bradycardia, atrioventricular block, dissection, perforation, myocardial infarction, stroke, and death compared to conventional procedure.
Methods
Materials and Methods
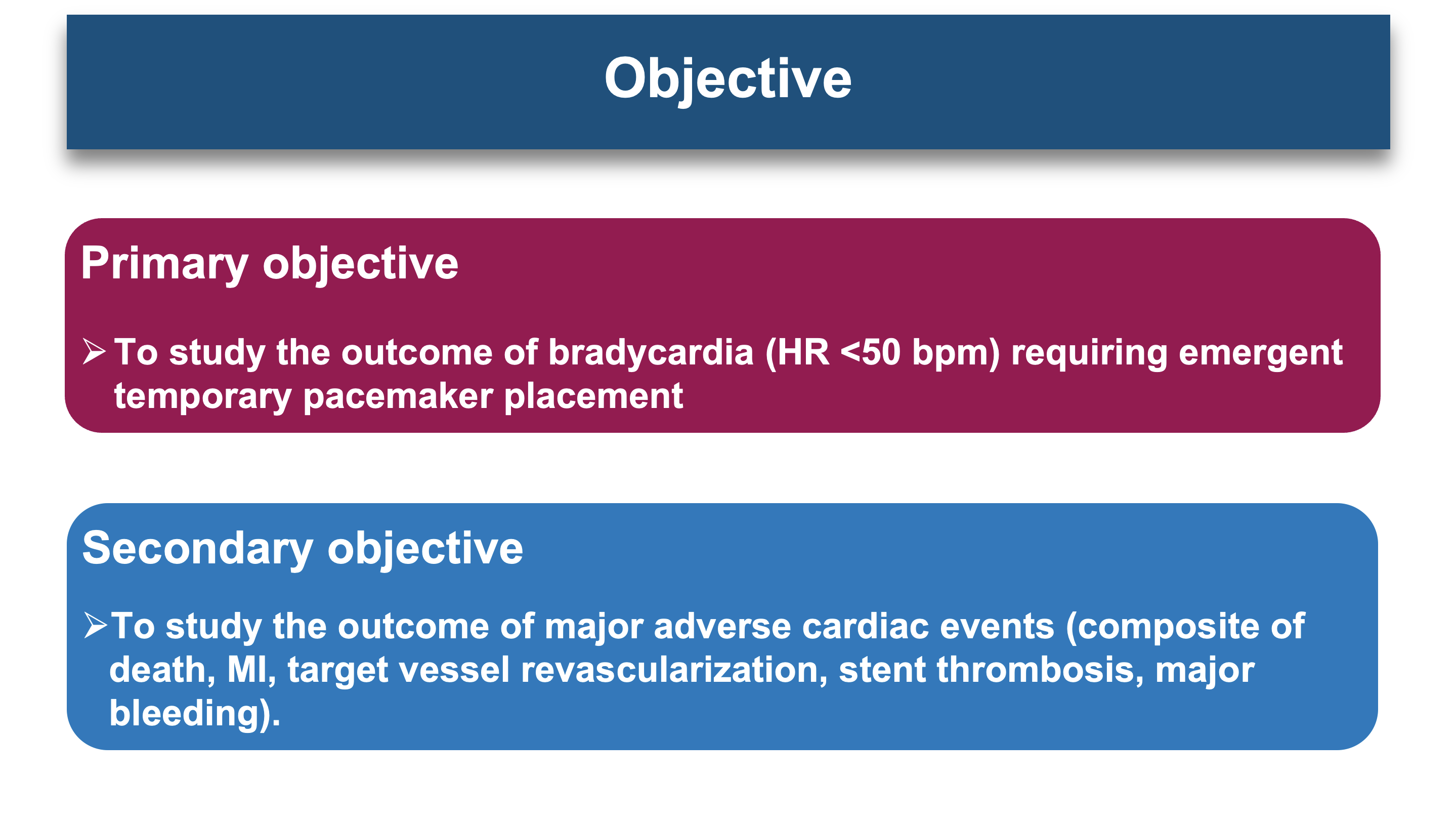
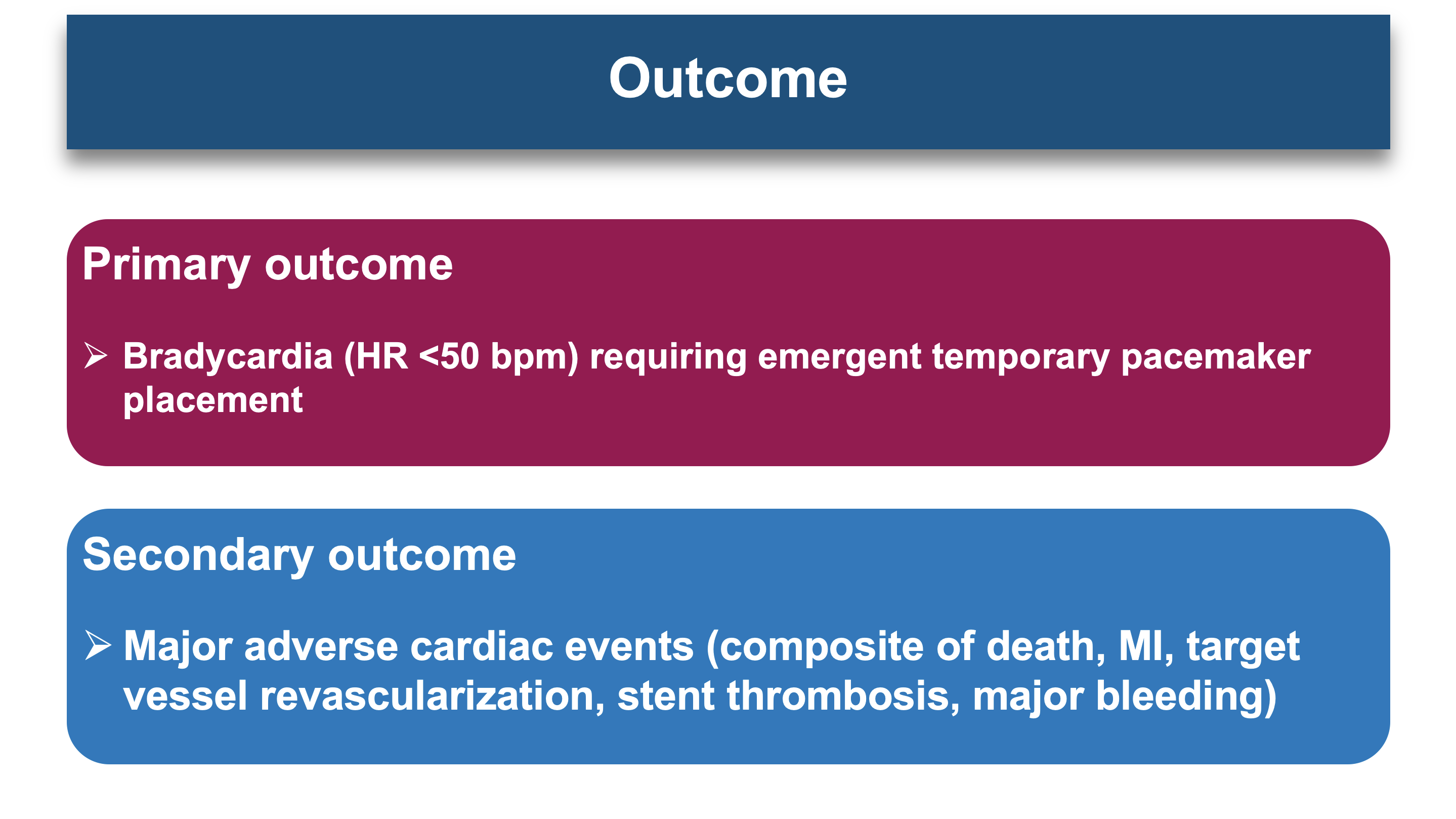
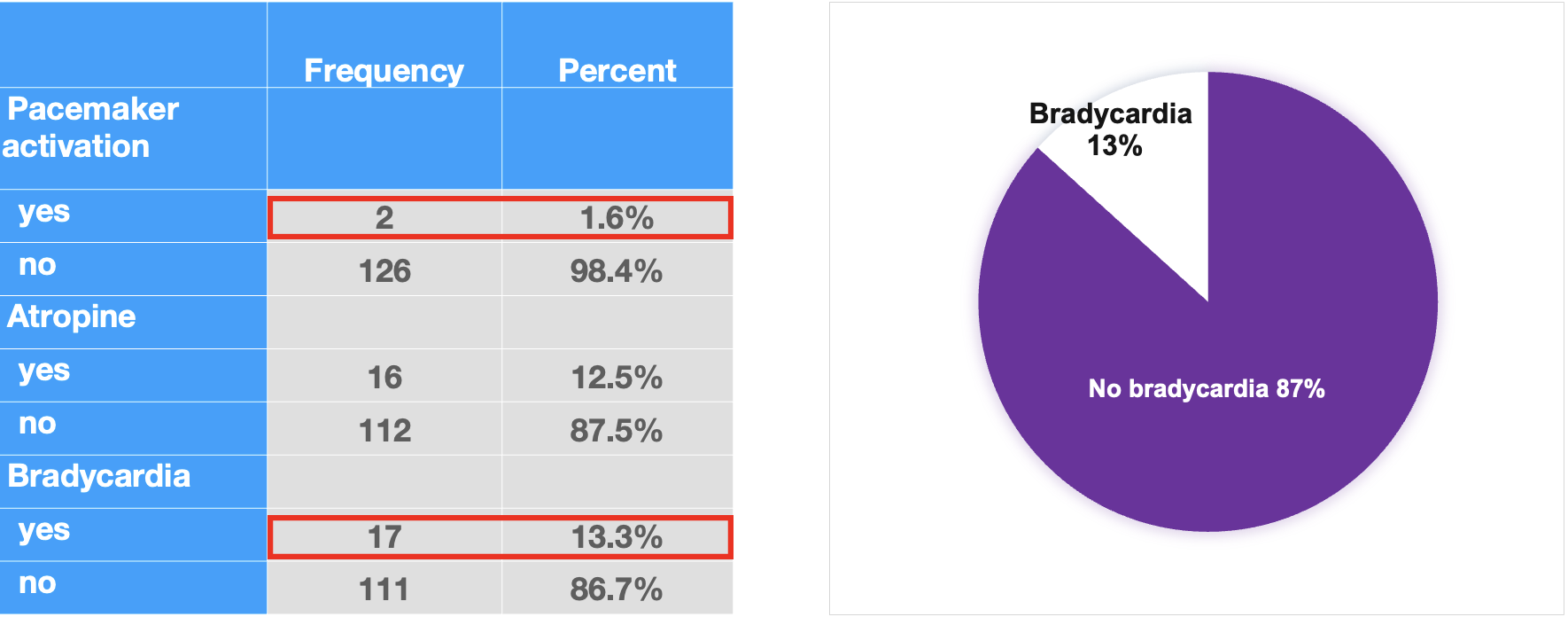
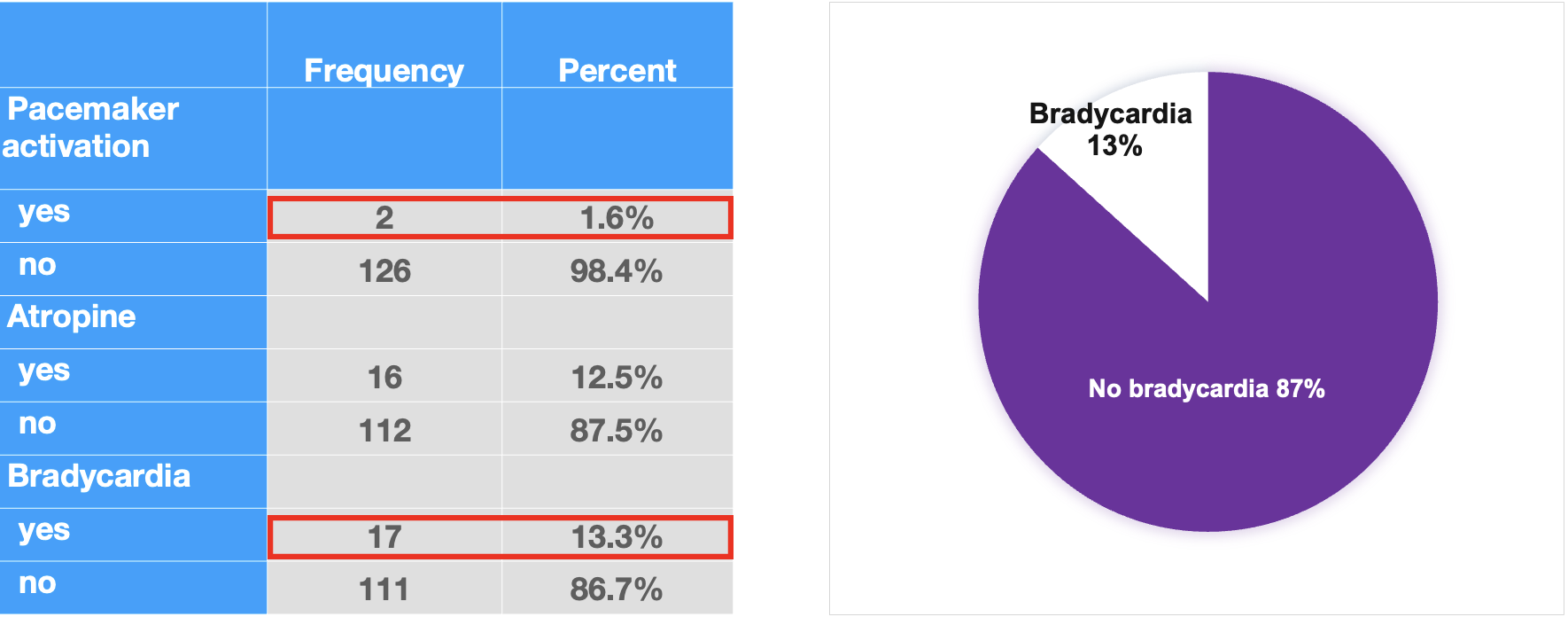
Results
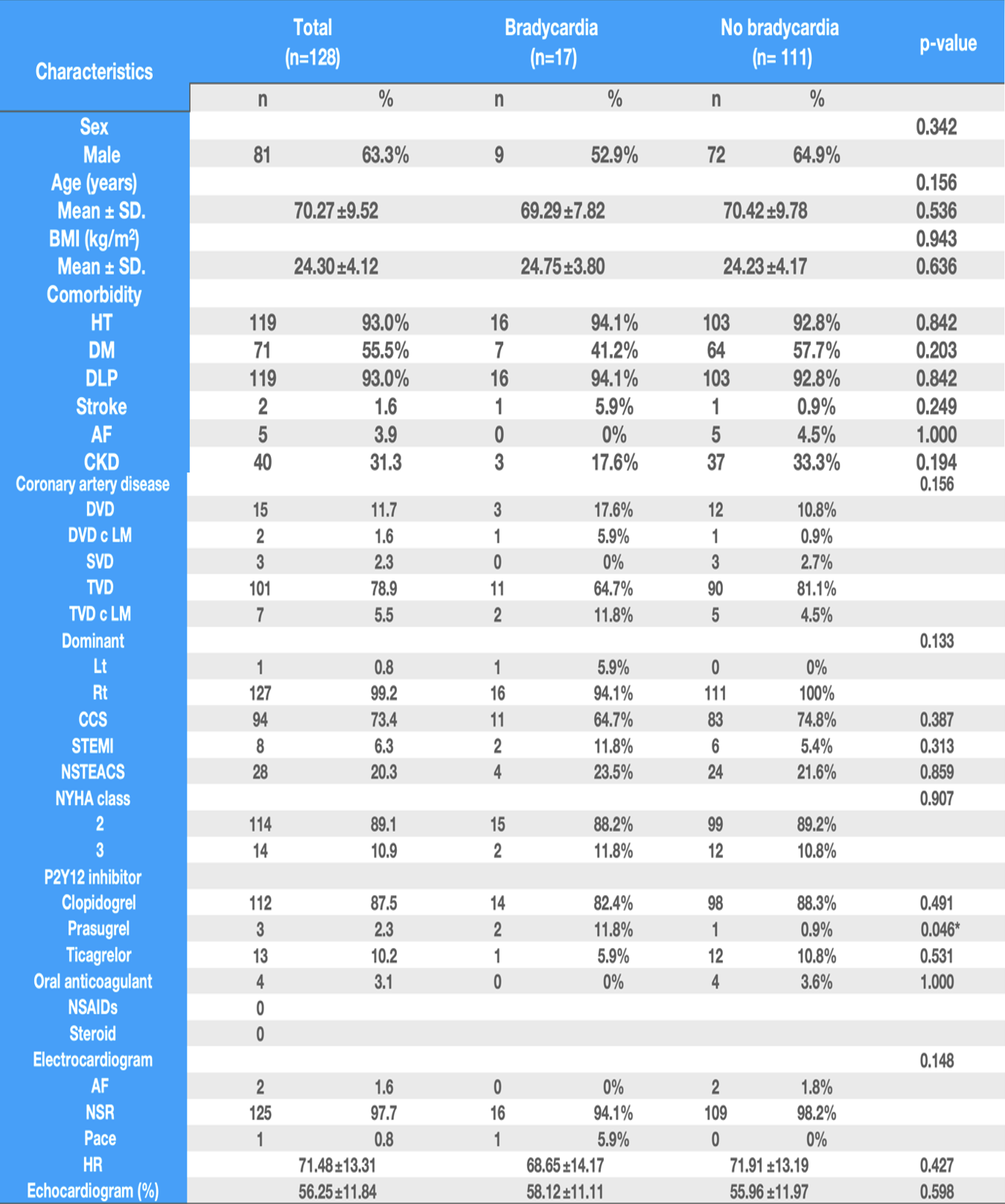
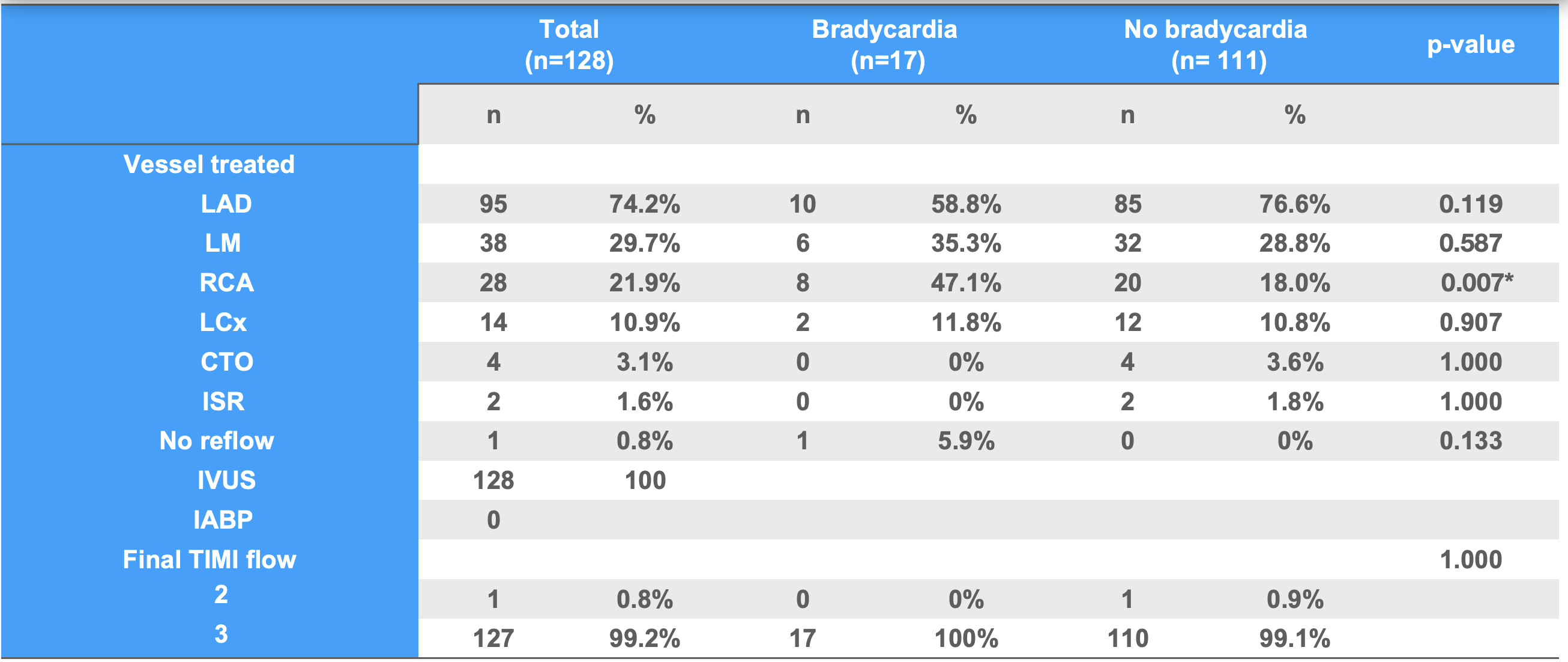
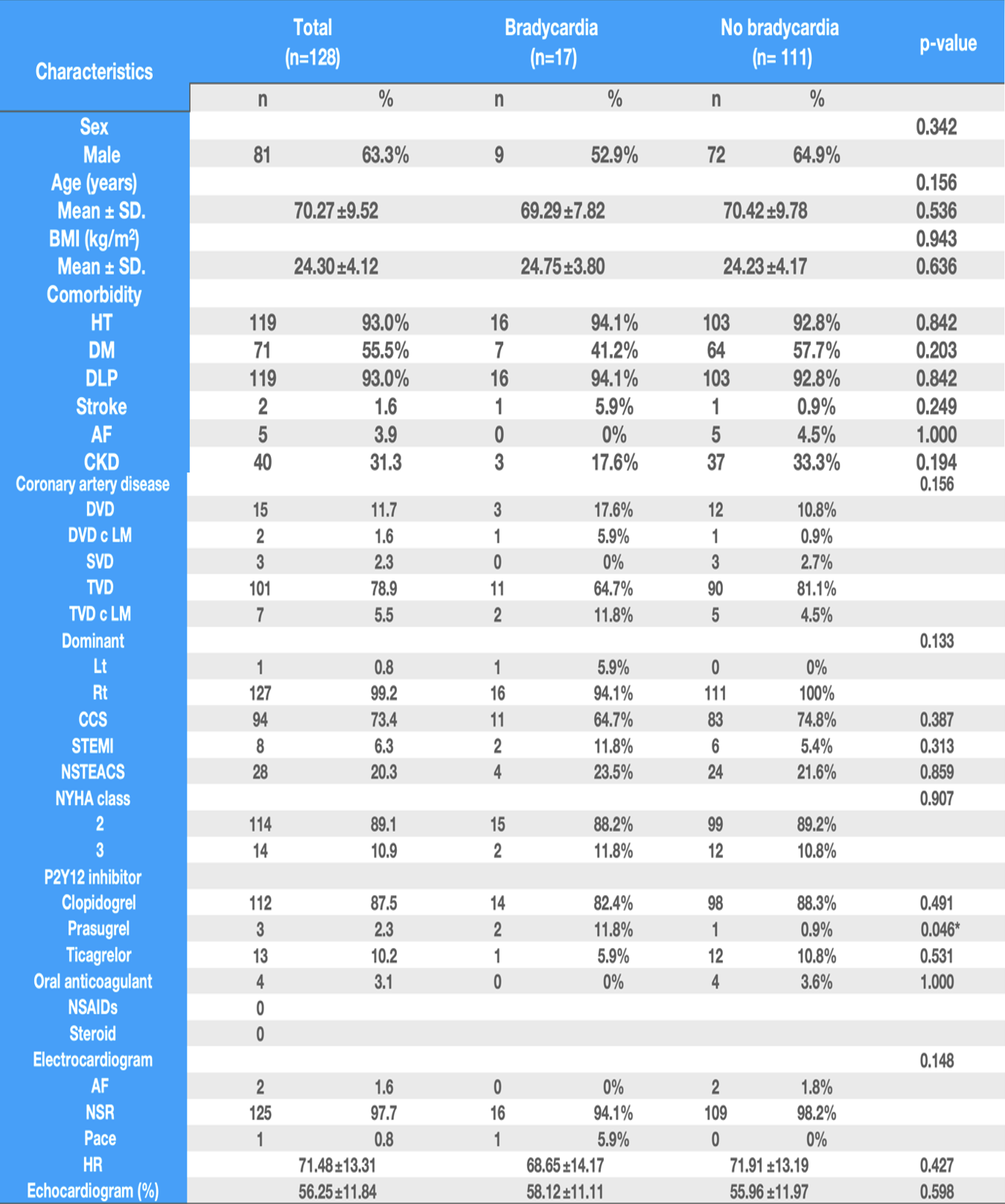
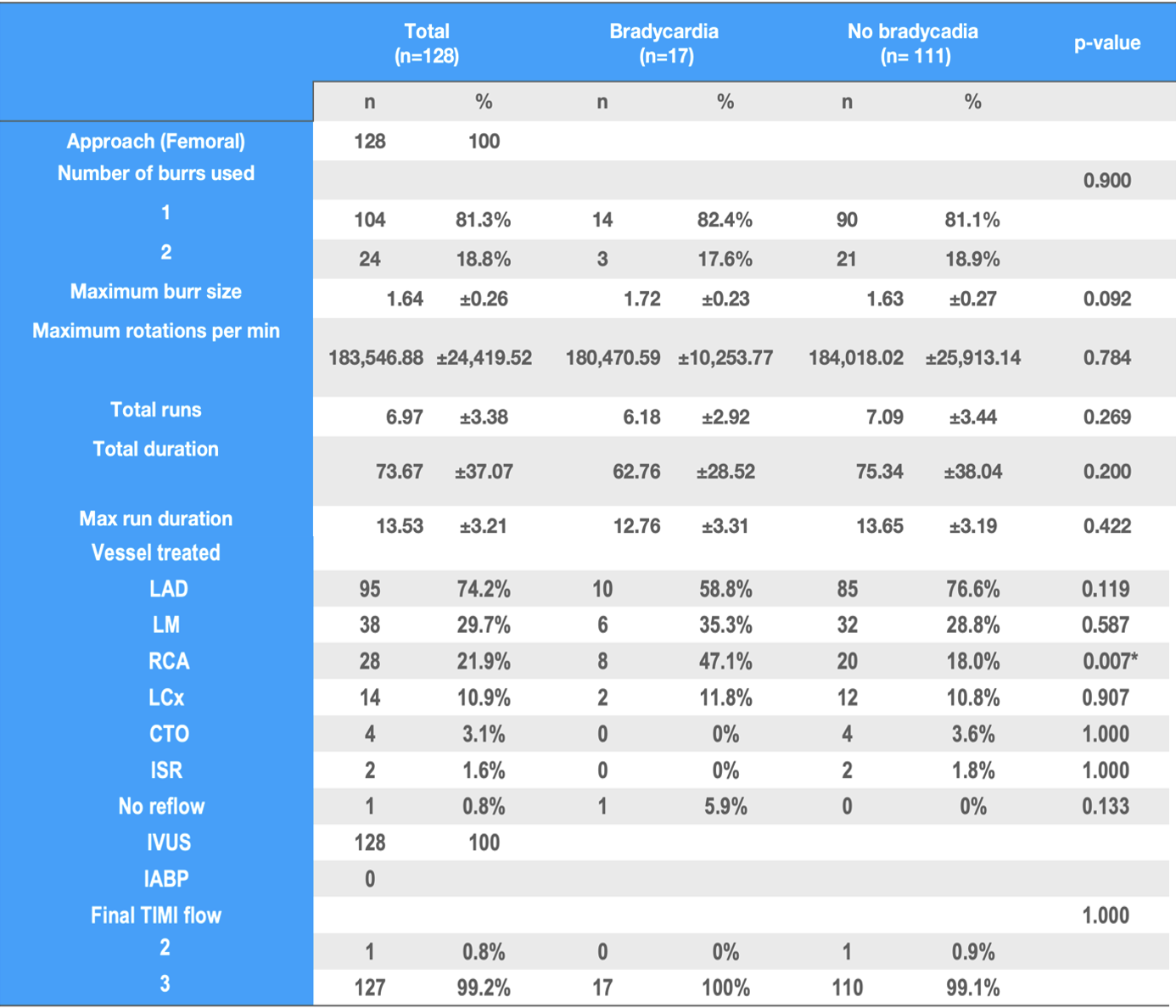
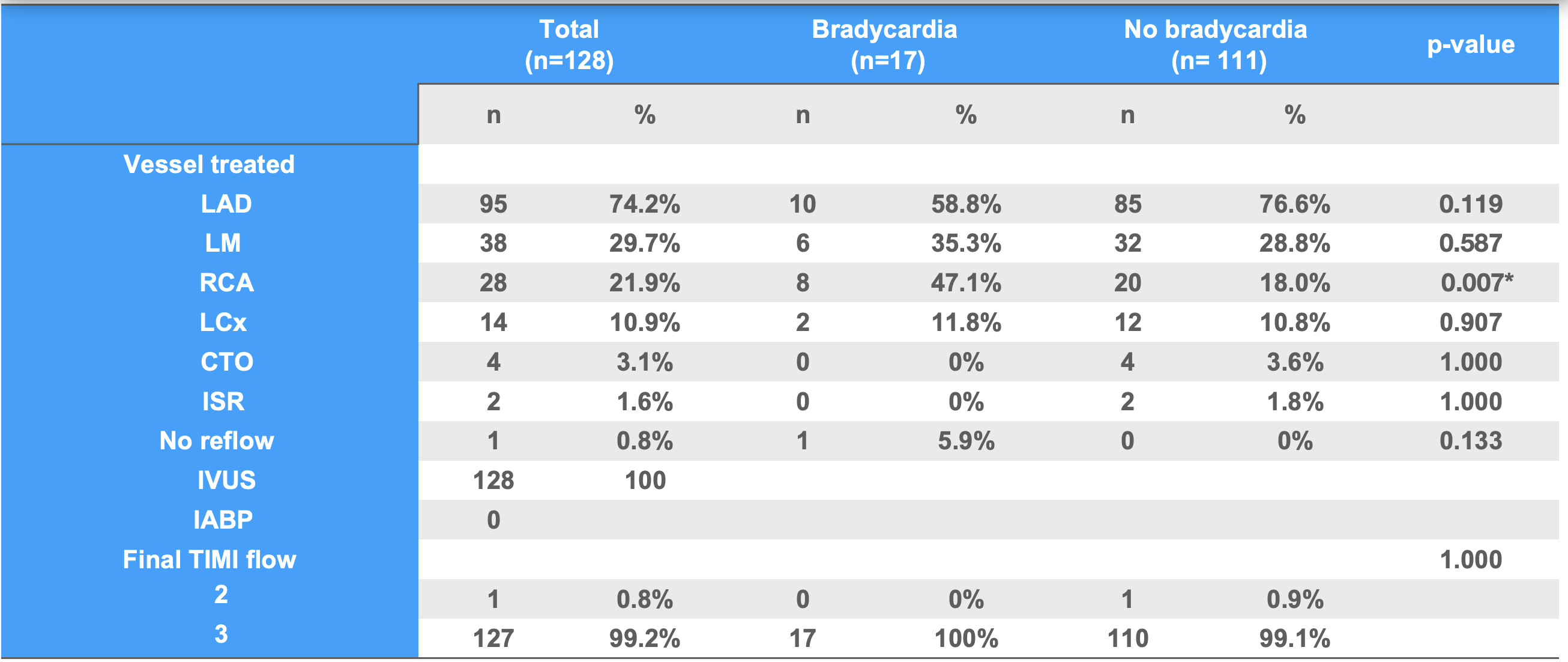
A total of 128 patients who underwent were enrolled in this study. The average was 70.27 ± 9.52 years. 63.3% of these patients were male. The average BMI was 24.3 ± 4.12 Kg/m2. Most of the patients had hypertension, diabetes mellitus and dyslipidemia. 78.9% of the patients had triple vessel disease. 73.4% of the patients were chronic coronary syndrome. 87.5% of the patients received clopidogrel. The average heart rate was 71.84 ± 13.31 bpm and was sinus rhythm. The average left ventricular ejection fraction was 56.25 ± 11.84%.
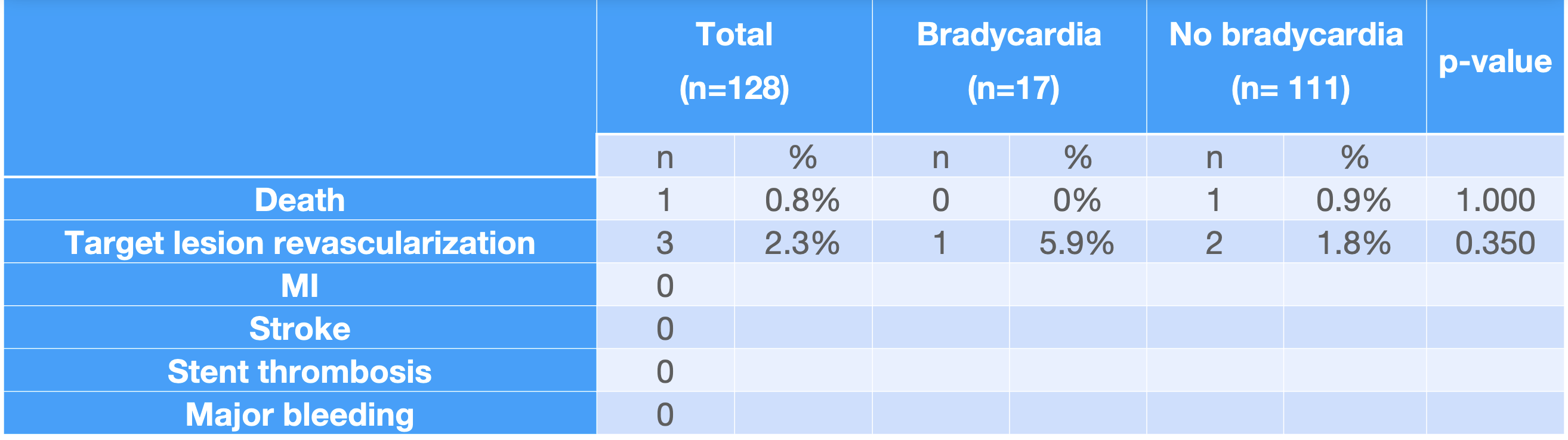
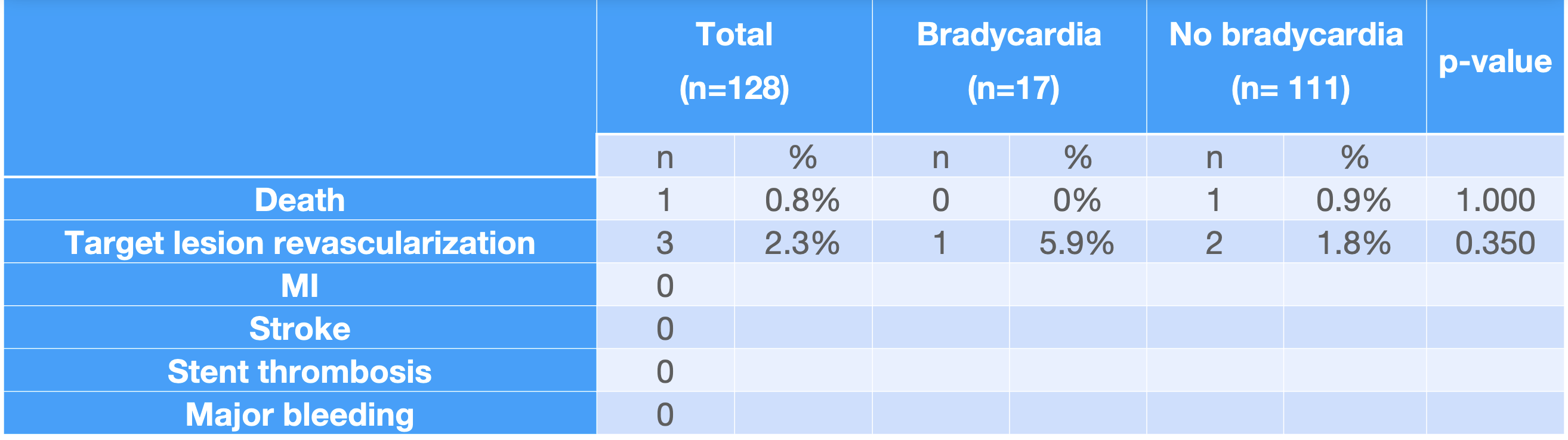
Conclusion
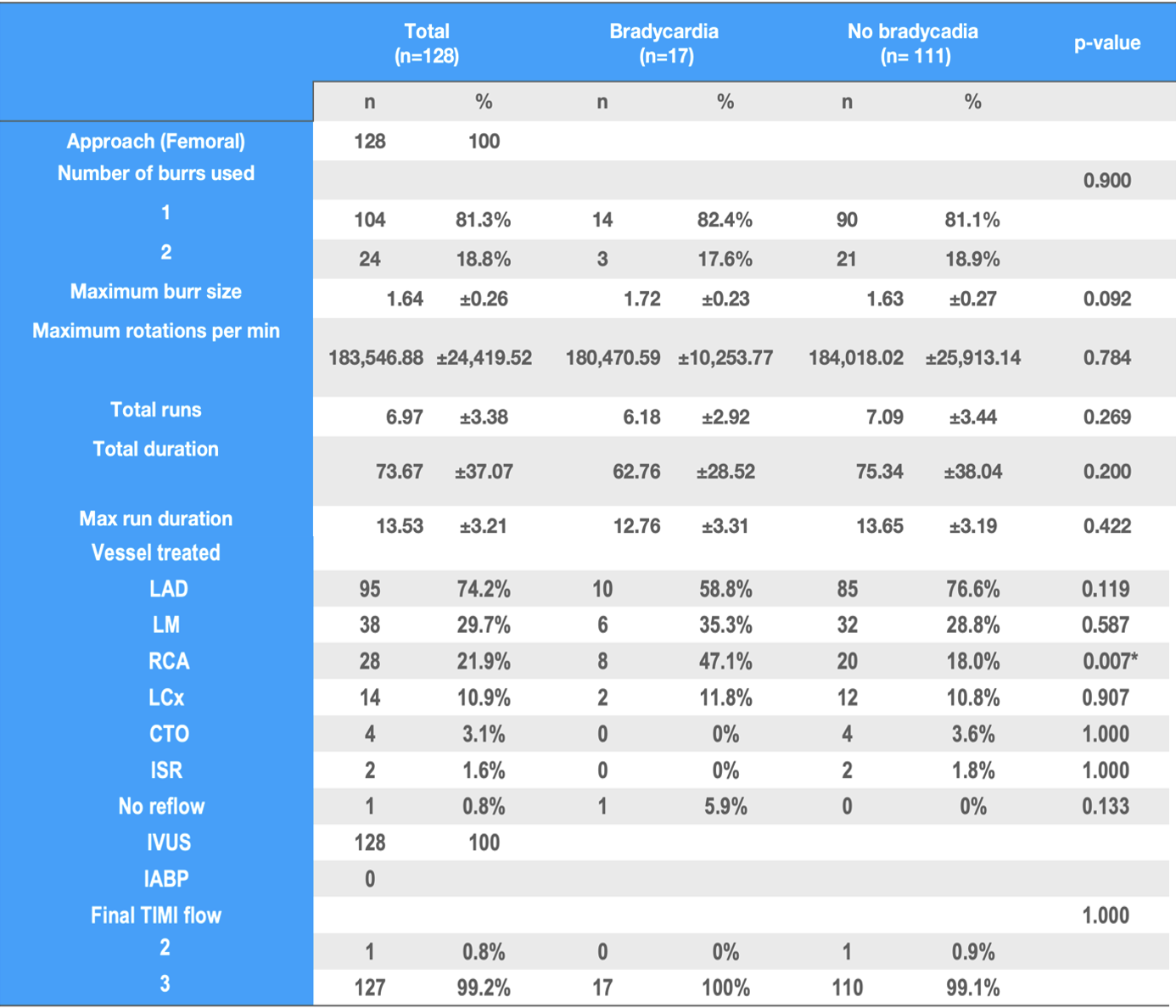
The incidence of bradycardia and temporary pacing during rotational atherectomy was very low. Bradycardia is most common with RCA lesions. The role of prophylactic temporary pacemaker should be considered with RA to the RCA and left dominant LCx artery to prevent conduction abnormalities but it is not necessary to use in the case of right dominant LCA.