
Jung-Min Ahn
Asan Medical Center, Republic of Korea
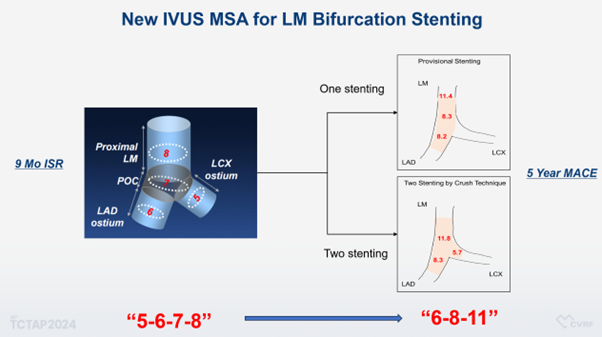
At TCTAP 2024, Jung-Min Ahn, MD (Asan Medical Center, Seoul, Korea) presented compelling new criteria for optimizing left main (LM) coronary artery stenting. Traditionally, intravascular ultrasound (IVUS) guidance has been recommended to enhance clinical outcomes in LM procedures, highlighted by the well-known "5-6-7-8" criteria developed at Asan Medical Center. This standard, primarily predictive of angiographic restenosis, has been a benchmark in the field.
A recent study scrutinizes the adequacy of these existing recommendations, focusing on the relationship between stent expansion in LM bifurcation and long-term clinical outcomes. Ahn conducted a comprehensive analysis of 292 patients who underwent LM two-stenting with crush technique. The study identified the minimal stent area (MSA) at various segments within the LM bifurcation—11.8 mm©ų at the distal LM, 8.3 mm©ų at the ostial left anterior descending (LAD), and 5.7 mm©ų at the ostial circumflex—which are crucial for predicting clinical outcomes, including major adverse cardiac events (MACE). The findings compellingly suggest that while the distal LM's MSA did not significantly predict clinical outcomes, the MSA at the ostia of LAD and circumflex independently predicted outcomes, marking them as critical areas for ensuring adequate stent expansion. Those in the under-expansion group exhibited notably poorer outcomes, further emphasizing the need for precise stent placement and expansion.
In another research, conducted on a large cohort of 879 patients at Asan Medical Center from March 2005 to September 2022, sought to validate the efficacy of IVUS in patients who underwent LM single-stent with crossover. The study identified the MSA from LM to LAD—11.4 mm©ų at the proximal LM, 8.3 mm©ų at the distal LM, and 8.1 mm©ų at the ostial LAD.
Importantly, these two studies propose a shift from the "5-6-7-8" to a "6-8-11" criteria, which better correlates with the observed clinical outcomes in LM PCI (Figure 1).
Ahn°Įs findings highlighted the importance of ensuring maximal MSA, as stent under-expansion was significantly associated with adverse long-term outcomes. The new criteria aim to establish more rigorous standards to ensure better clinical outcomes.
The presentation concluded with a strong endorsement of intracoronary imaging as a pivotal tool for optimizing stent placement. It was emphasized that while imaging itself does not directly correlate with better outcomes, strategic use of this technology to guide stent placement contributes significantly to improved patient and stent outcomes. This session not only provided invaluable insights into the technical aspects of LM PCI but also reinforced the importance of ongoing research and adaptation of techniques in the interventional cardiology field.
TCTAP Workshops
New Concept of Bifurcation PCI
Thursday, April 25, 4:00 PM ~ 5:40 PM
Valve & Endovascular Theater, Level 2
Edited by

Ju Hyeon Kim, MD
Asan Medical Center, Korea (Republic of)
