
Adrian P. Banning
Oxford University Hospitals NHS Foundation Trust
United Kingdom
In a captivating presentation at TCTAP 2024 in Incheon, Korea, Adrian Banning, MD (Oxford University, United Kingdom) illuminated the current landscape of reperfusion therapy in acute myocardial infarction (MI), with a particular focus on the outcomes of intermittent coronary sinus occlusion.
Despite technological strides enhancing the efficacy of reperfusion therapy post-acute MI, outcomes have been stagnant since the early 2000s. Cardiologists worldwide acknowledge their unwavering dedication to patient care yet recognize the persistent need for improved clinical outcomes in acute MI cases. Countless clinical trials have endeavored to evaluate novel devices and approaches to better prognoses, yet many have failed due to inefficacy.
While the current standard treatments yield favorable results in approximately 60-70% of ST-segment elevation myocardial infarction (STEMI) patients, the crux lies in individualized care. Each patient presents with unique comorbidities and socioeconomic factors, necessitating tailored approaches within the framework of standard management protocols.
The size of the infarct is a pivotal determinant of clinical outcomes post-acute MI. Extensive research underscores a direct correlation between larger infarct sizes and worsened clinical prognoses. Meta-analyses have elucidated this relationship, showing mortality and heart failure (HF) hospitalization rates escalating alongside increasing infarct sizes.
Various validated tools have emerged to refine outcome prognostication. Microvascular occlusion, detected via cardiac magnetic resonance imaging (CMR) post-percutaneous coronary intervention (PCI), stands out as a robust predictor of mortality and HF hospitalization within one year. Additionally, the index of microcirculatory resistance (IMR) has emerged as an early discriminator, with post-PCI IMR values exceeding 40 signaling adverse outcomes in the catheterization laboratory. Recent advancements, such as angiography-derived IMR, leveraging computational flow dynamics for 3D vessel modeling, exhibit a promising correlation with wire-based IMR measurements.
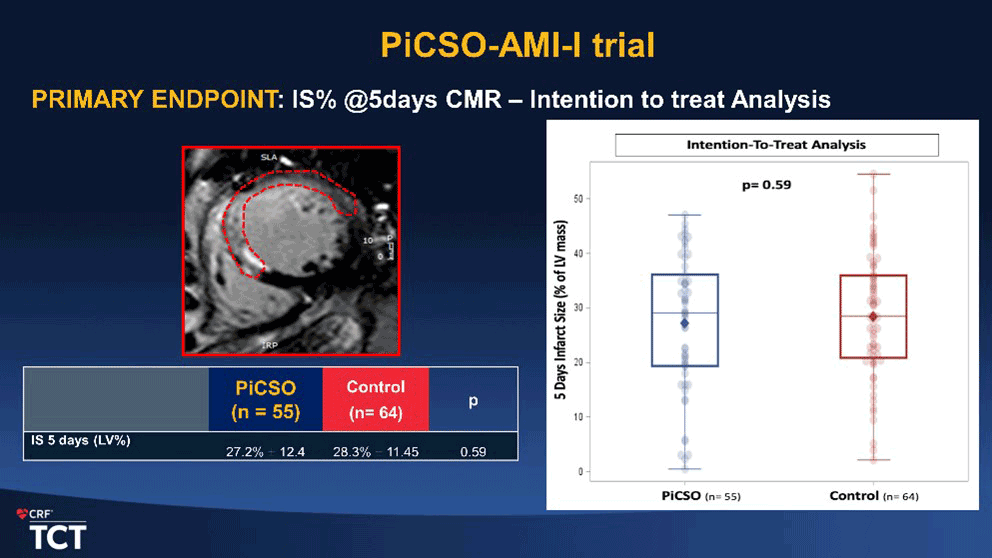
In light of these advancements, Adrian Banning, MD, unveiled findings from the pressure-controlled intermittent coronary sinus occlusion (PiCSO)-AMI-I trial, evaluating the clinical efficacy of intermittent coronary sinus occlusion. Enrolling 145 STEMI patients, the trial randomized participants to conventional PCI or PiCSO-assisted PCI. Disappointingly, the primary endpoint of infarct size at 5 days by CMR failed to exhibit significant differences between groups despite prolonged PCI durations and increased radiation and radiocontrast exposure (Figure 1). Similarly, clinical outcomes remained unaltered.
As pursuing enhanced outcomes in acute MI treatment persists, these findings underscore the necessity for continued exploration and innovation within reperfusion therapy paradigms.
Meet the Experts Over Breakfast
ACS and Acute MI: Brand New Issues
Saturday, April 27, 7:30 AM ~ 8:25 AM
Presentation Room 2, Level 1
Edited by
Yong-Hoon Yoon, MD
Ulsan City Hospital, Korea (Republic of)
