Lots of interesting abstracts and cases were submitted for TCTAP 2024. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-074
Another Way to Move the Cap
By Chin Wai Lai, Siu Fung Wong, Tak Shun Chung, Chiu Sun Yue
Presenter
Chin Wai Lai
Authors
Chin Wai Lai1, Siu Fung Wong2, Tak Shun Chung1, Chiu Sun Yue1
Affiliation
United Christian Hospital, Hong Kong, China1, Royal Sussex County Hospital, United Kingdom2,
View Study Report
TCTAP C-074
Coronary - Complex PCI - CTO
Another Way to Move the Cap
Chin Wai Lai1, Siu Fung Wong2, Tak Shun Chung1, Chiu Sun Yue1
United Christian Hospital, Hong Kong, China1, Royal Sussex County Hospital, United Kingdom2,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
Our patient was a 63 year-old gentleman with past medical history of hypertension, dyslipidemia, diabetes and end stage renal failure on peritoneal dialysis. He first presented to us in April 2023 with Wellen Syndrome and ischemic acute pulmonary edema.


Relevant Test Results Prior to Catheterization
Echocardiogram showed a reduced left ventricular ejection fraction at 35-40%.
Relevant Catheterization Findings
Coronary angiogram at that time showed mid left anterior descending artery (LAD) subtotal lesion, distal left circumflex artery (LCx) chronic total occlusion (CTO) and left posterolateral artery severe disease (LPL). Percutaneous coronary intervention (PCI) was done to culprit LAD. He made uneventful recovery from the acute episode and was readmitted for staged PCI to LCx CTO 3months later.




Interventional Management
Procedural Step
Antegrade wiring approach was adapted. Distal LCx CTO was wired with Gaia N1 with turnpike support. After going into subintimal, Sasuke assisted parallel wire technique was attempted with Gaia N2. Yet, it failed to achieve exit to distal true lumen. As IVUS confirmed true lumen wiring of proximal CTO body, it was predilated with 2.5NC balloon. Surprisingly, new CTO entry stump appeared. Wiring with Gaia N2 with turnpike support successfully crossed to LPL. Tip injection confirmed distal true lumen. Distal LCx was then predilated with 2.0 and 2.5 NC balloon. Obtuse marginal(OM) 2 CTO was wired with IVUS guidance and parallel wire of Gaia N1 N2 under turnpike support. It was then predilated with 2.5NC balloon. IVUS revealed a sizable OM2 so culotte stenting of LPL/ OM2 was performed with 2.5 x 49mm DES(distal LCx-OM2) and 3.0 x 49mm DES (distal LCx-LPL) and optimized with kissing balloon. Proximal optimization technique (POT) was applied at distal LCx with 3.0 NC balloon. Proximal LCx was predilated with 3.5NC balloon and proximal to distal LCx was stented with overlapping 3.5 x 29mm DES. As IVUS along LAD showed significant focal calcific disease at distal left main (LM). Distal LM to proximal LAD was also stented with 4.0 x 24mm DES after pre-dilatation. Proximal LCx and LM were finally optimized with pot side pot. The final angiographic and IVUS result was satisfactory with TIMI 3 flow.


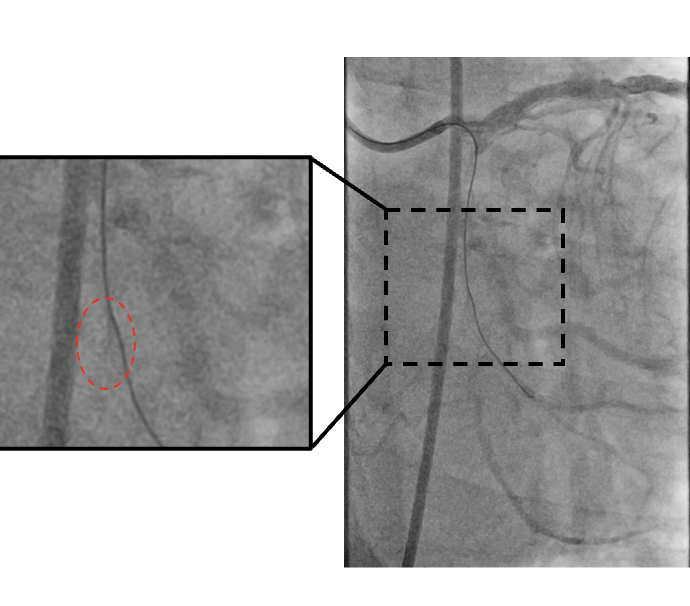


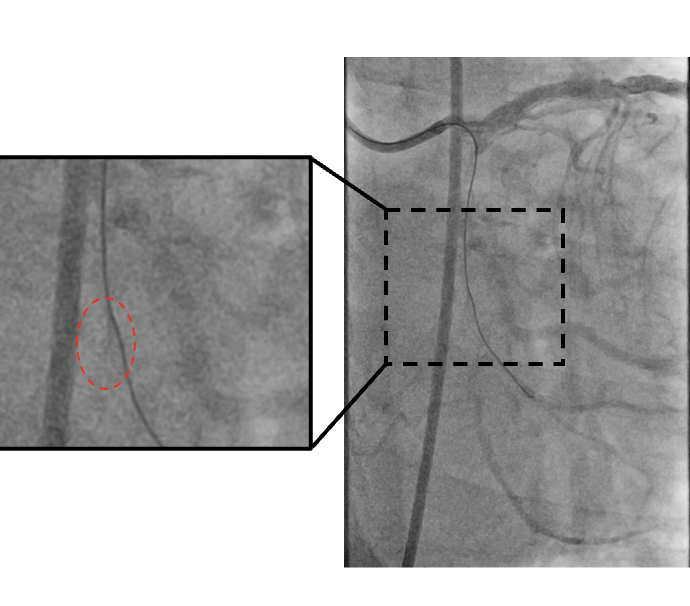
Case Summary
This case demonstrated a CTO case successfully done based on the Global Chronic Total Occlusion Crossing Algorithm and proximal cap modification. The algorithmic approach improves procedural success and safety in CTO intervention. Despite so, antegrade wiring of the proximal cap remains challenging. Balloon dilatation of the true CTO segment can however bring in a surprise change in its morphology and move the cap. Careful analysis of angiogram after proximal cap modification and attention to details are crucial to identify such a change which eventually facilitates the wiring.

