Lots of interesting abstracts and cases were submitted for TCTAP 2024. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-086
Chain Reaction--Endless Nightmares!
By Dhiman Banik
Presenter
Dhiman Banik
Authors
Dhiman Banik1
Affiliation
National Heart Foundation Hospital & Research Institute, Bangladesh1,
View Study Report
TCTAP C-086
Coronary - Complex PCI - In-Stent Restenosis
Chain Reaction--Endless Nightmares!
Dhiman Banik1
National Heart Foundation Hospital & Research Institute, Bangladesh1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
• Mr. X-29 years old, Physician by profession.
• Hypertensive, Strong family history of IHD.
• H/O PCI (LAD).
• H/O CABG (LIMA to LAD, Sequential SVG to D1 and OM branch).
• Now presented with chest pain & SOB for two days.
• NSTEMI.

• Hypertensive, Strong family history of IHD.
• H/O PCI (LAD).
• H/O CABG (LIMA to LAD, Sequential SVG to D1 and OM branch).
• Now presented with chest pain & SOB for two days.
• NSTEMI.

Relevant Test Results Prior to Catheterization
• CBC:Hb:11.9 gm/dl
• RBS: 5.9 mmol/L,
• S. Creatinine 1.3 mg/dl
• ECG shows T↓ in V1-V6.
• Echo reveals no regional wall motion abnormality with LVEF -60%.
• RBS: 5.9 mmol/L,
• S. Creatinine 1.3 mg/dl
• ECG shows T↓ in V1-V6.
• Echo reveals no regional wall motion abnormality with LVEF -60%.
Relevant Catheterization Findings
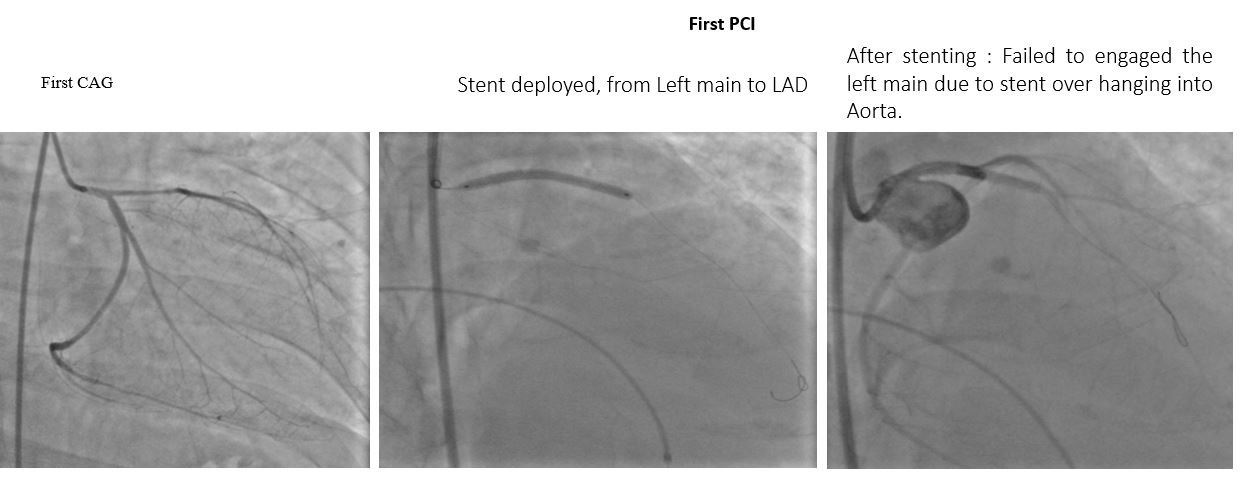
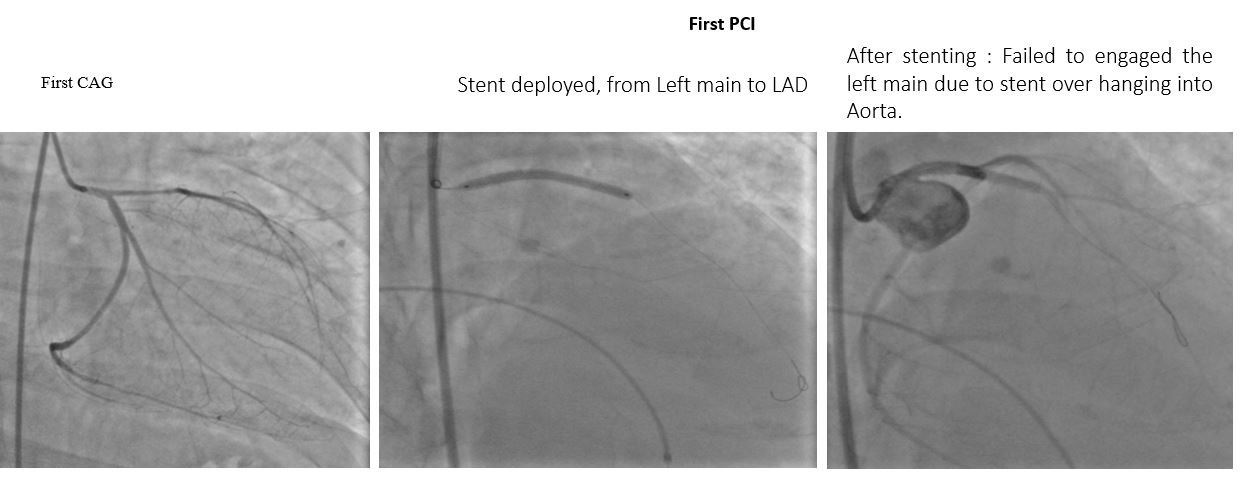
First CAG: Left Dominant & PCI was done in LAD.
After 6 months of PCI, patient developed NSTEMI.
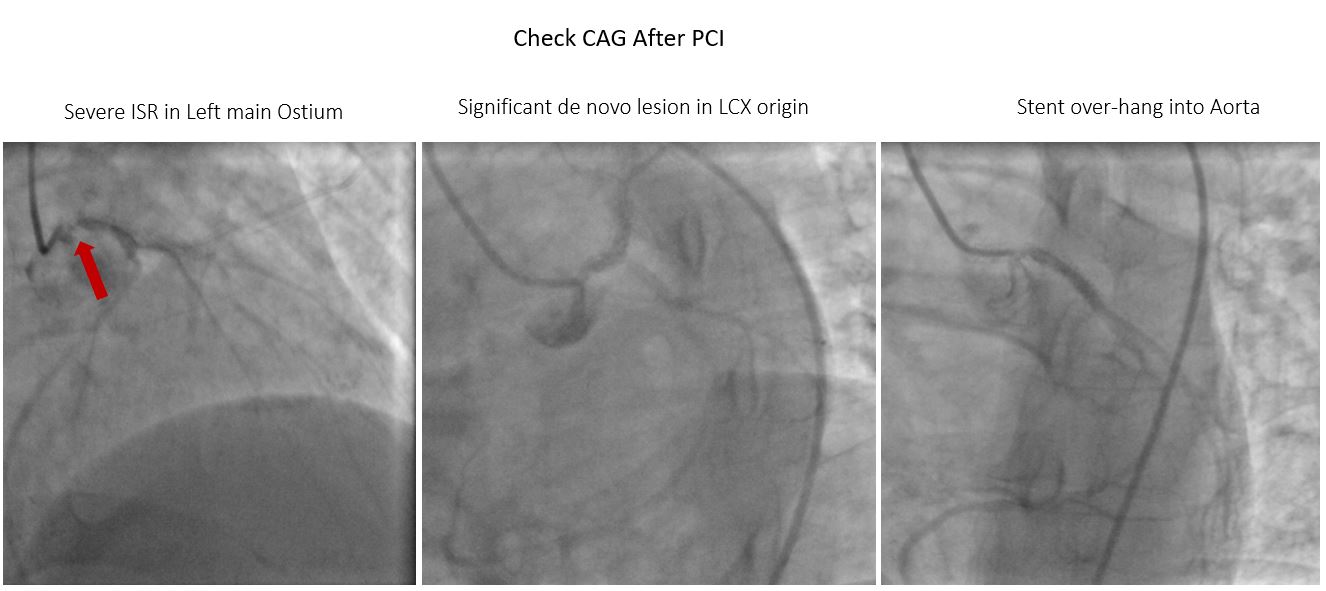
Again Check CAG done: severe ISR in LMCA with significant stenosis in LCX ostia.
CABG done, but after 14 months patient again developed NSTEMI.
Check CAG revealed:
LMCA (significant ISR) & LAD (100% ISR).
Dominant LCX with 90% ostial stenosis.
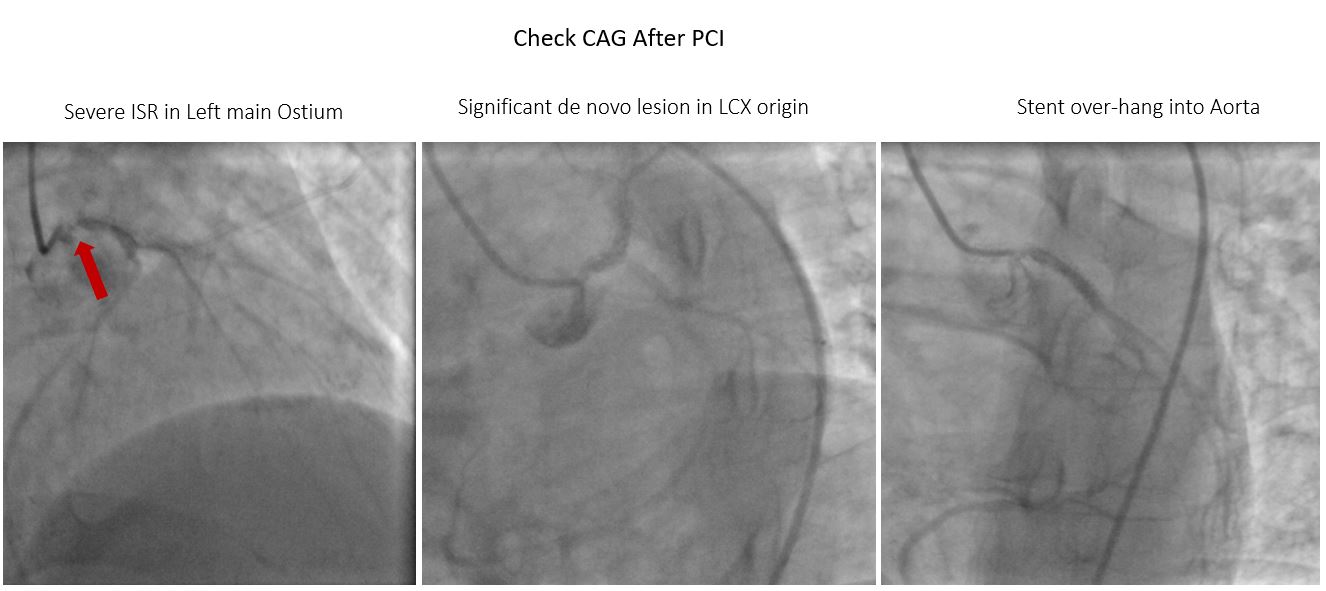

After 6 months of PCI, patient developed NSTEMI.
Again Check CAG done: severe ISR in LMCA with significant stenosis in LCX ostia.
CABG done, but after 14 months patient again developed NSTEMI.
Check CAG revealed:
LMCA (significant ISR) & LAD (100% ISR).
Dominant LCX with 90% ostial stenosis.
SVG to OM & D1 showed Severe stenosis in its proximal part as well as distal anastomotic site.
LIMA to LAD stenosis distal anastomotic site.

Interventional Management
Procedural Step
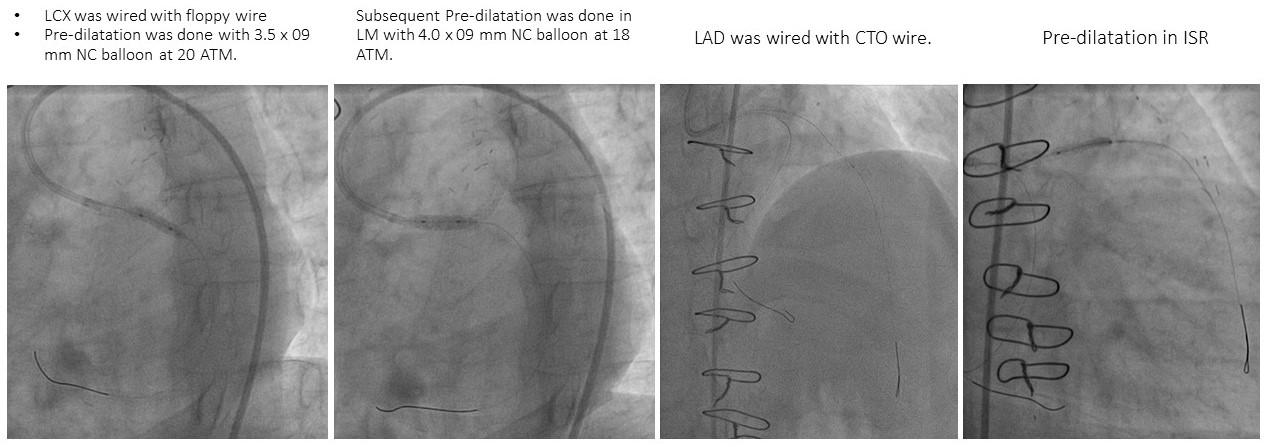
• LCX was wired with floppy wire.
• Pre-dilatation was done with 3.5 x 09 mm NC balloon at 20 ATM.
• Subsequent Pre-dilatation was done in LM with 4.0 x 09 mm NC balloon at 18 ATM.
• LAD was wired with CTO wire.
• Pre-dilatation in ISR.
• 4.5mm x 22 mm DES was inflated in LMCA to LCX
• IVUS study LMCA to LAD was done.
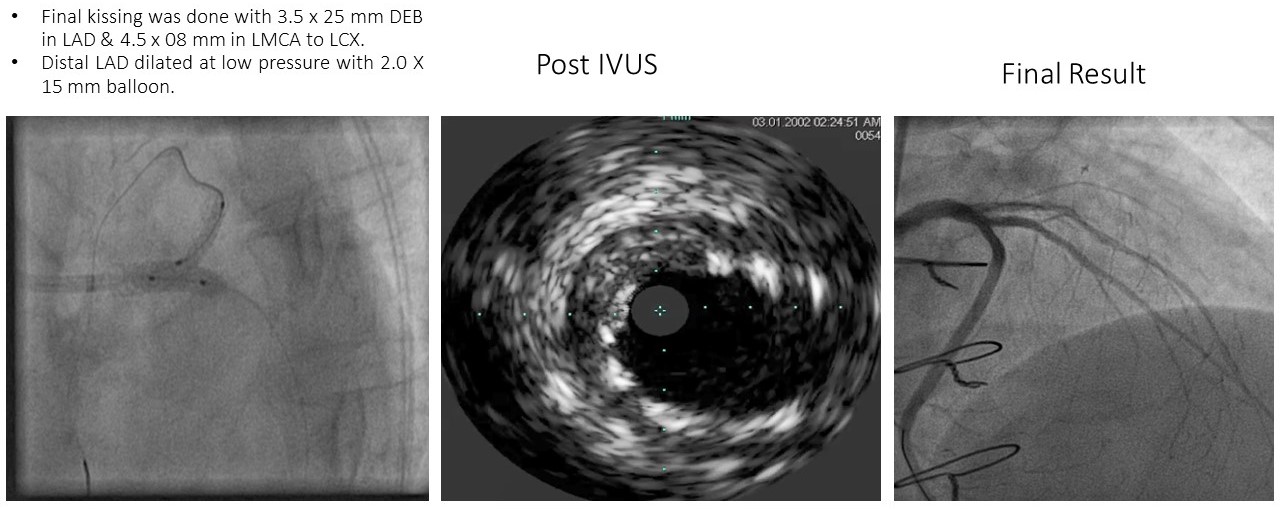
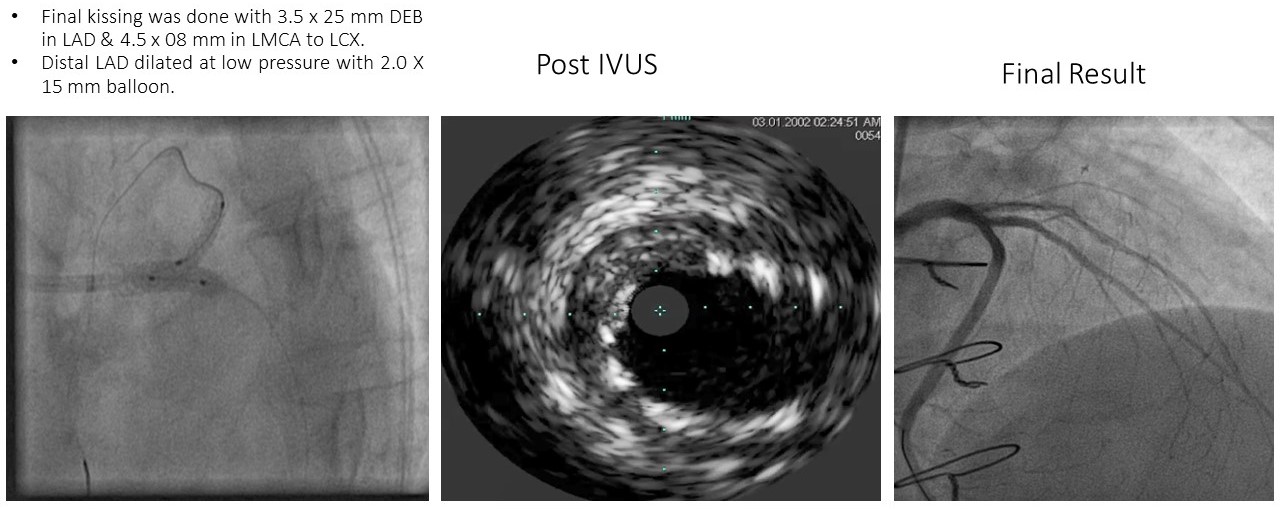
• Final kissing was done with 3.5 x 25 mm DEB in LAD & 4.5 x 08 mm in LMCA to LCX.
• Distal LAD dilated at low pressure with 2.0 X 15 mm balloon.
• IVUS was done revealed good expansion & well apposition.
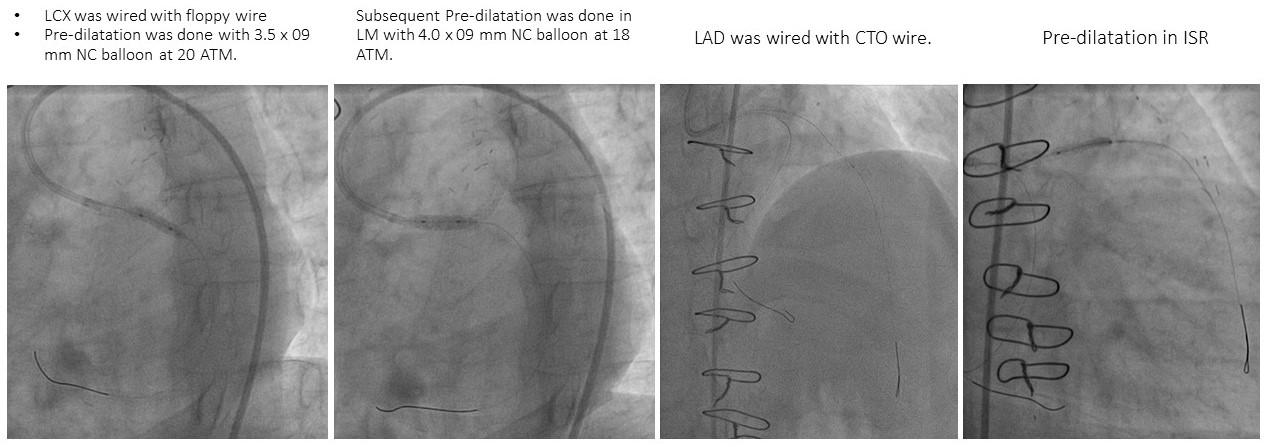

• Pre-dilatation was done with 3.5 x 09 mm NC balloon at 20 ATM.
• Subsequent Pre-dilatation was done in LM with 4.0 x 09 mm NC balloon at 18 ATM.
• LAD was wired with CTO wire.
• Pre-dilatation in ISR.
• 4.5mm x 22 mm DES was inflated in LMCA to LCX
• IVUS study LMCA to LAD was done.
• Final kissing was done with 3.5 x 25 mm DEB in LAD & 4.5 x 08 mm in LMCA to LCX.
• Distal LAD dilated at low pressure with 2.0 X 15 mm balloon.
• IVUS was done revealed good expansion & well apposition.

Case Summary
• Any PCI or CABG is not free from life threatening complications.
• Before doing an ostial LMCA in a left dominant case the pros and cons should be carefully assessed.
• Proper sizing & placement of the stent is mandatory.
• Stent should be properly inflated & over hanging in the aorta should be avoided.
• For the proper assessment of lesion severity in ostial Left main, IVUS & FFR can be of immense value.
• In fact overhanging of the stent lead to great difficulty during check CAG & redo PCI.
• Before doing an ostial LMCA in a left dominant case the pros and cons should be carefully assessed.
• Proper sizing & placement of the stent is mandatory.
• Stent should be properly inflated & over hanging in the aorta should be avoided.
• For the proper assessment of lesion severity in ostial Left main, IVUS & FFR can be of immense value.
• In fact overhanging of the stent lead to great difficulty during check CAG & redo PCI.

