Lots of interesting abstracts and cases were submitted for TCTAP 2024. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-053
Chronic Total Occlusion: To Treat or not to Treat?
By Ying-Chang Tung
Presenter
Ying-Chang Tung
Authors
Ying-Chang Tung1
Affiliation
Chang Gung Memorial Hospital, Taiwan1,
View Study Report
TCTAP C-053
Coronary - Complex PCI - CTO
Chronic Total Occlusion: To Treat or not to Treat?
Ying-Chang Tung1
Chang Gung Memorial Hospital, Taiwan1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
The patient was a 56-year-old man with a history of dyslipidema and three-vessel coronary artery disease. He underwent LAD stenting in 2017 at an outside institute, and CTOs in LCx and RCA were left untreated. He remained clinically uneventful until a traffic accident in Oct 2020, resulting in multiple bone fractures, hemothorax and liver hemorrhage. He was immediately transferred to our hospital for transarterial embolization to address the liver hemorrhage.


Relevant Test Results Prior to Catheterization
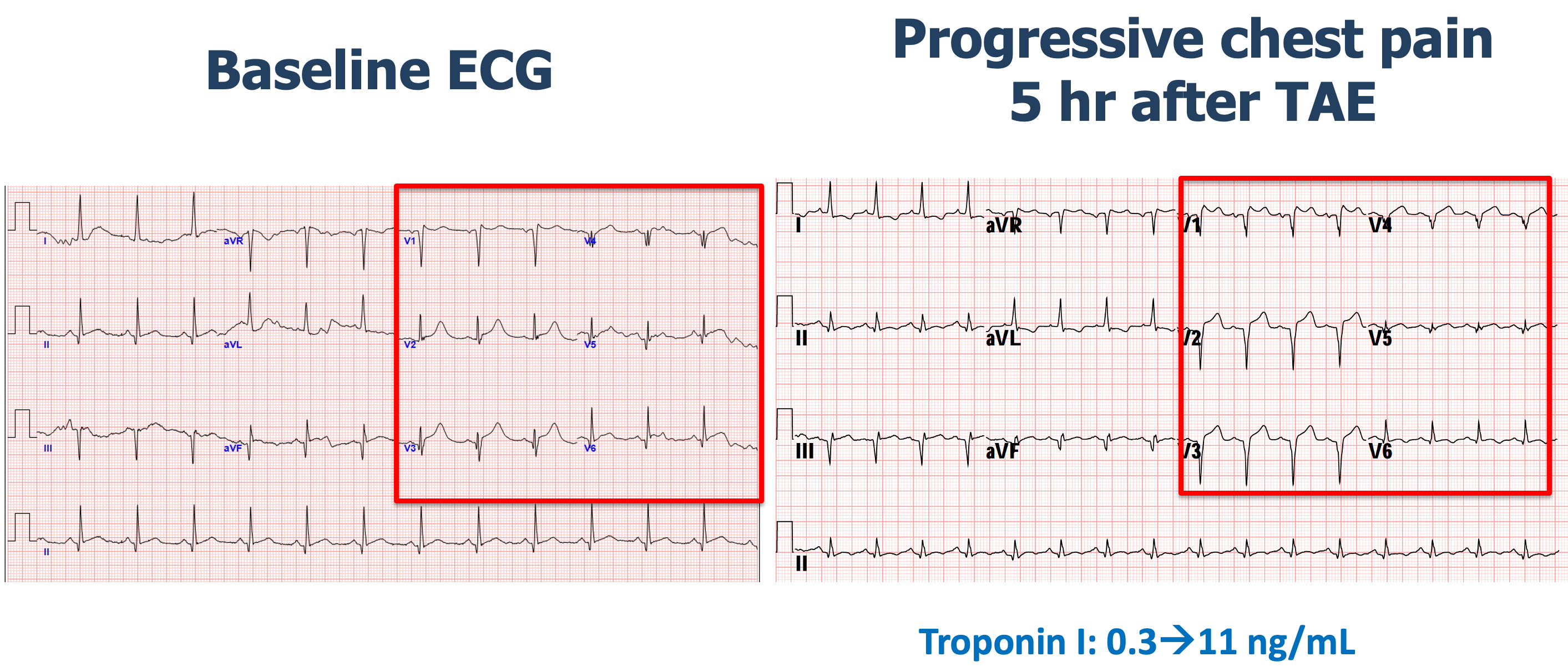
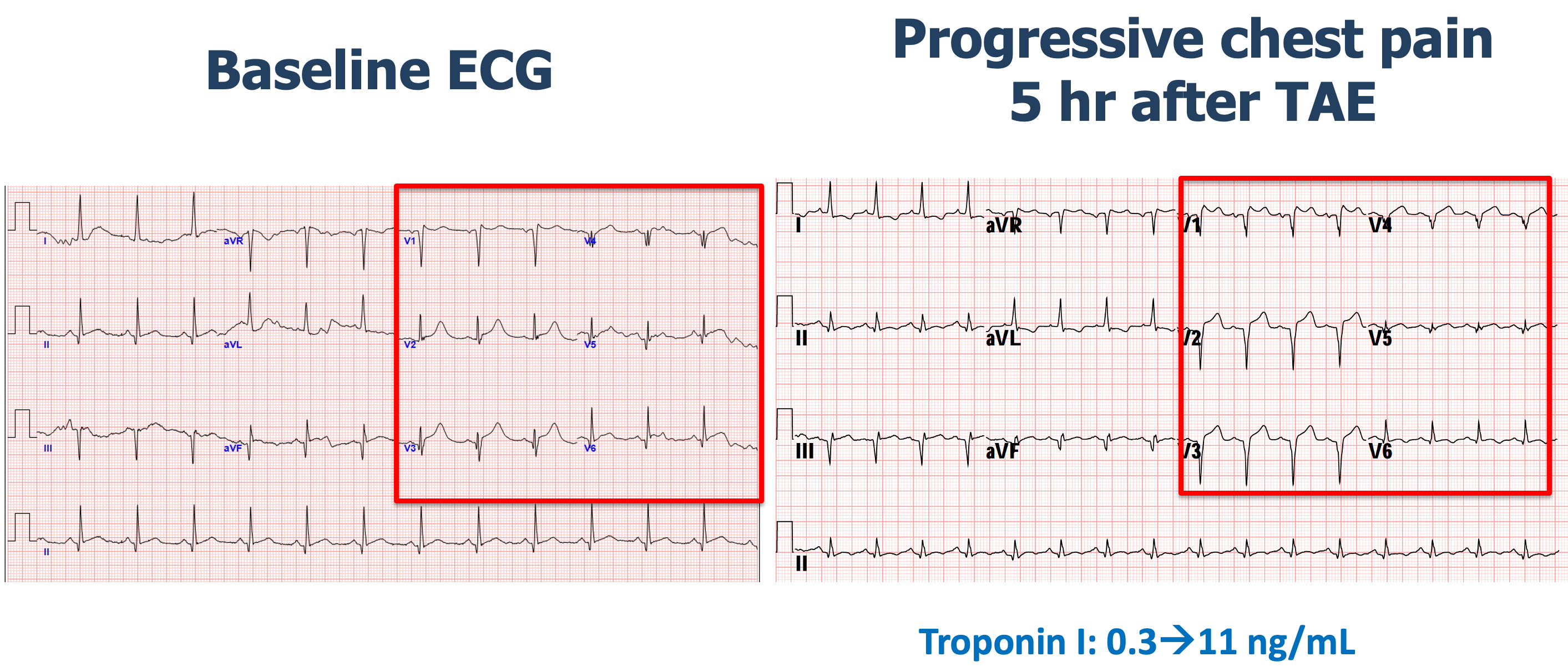
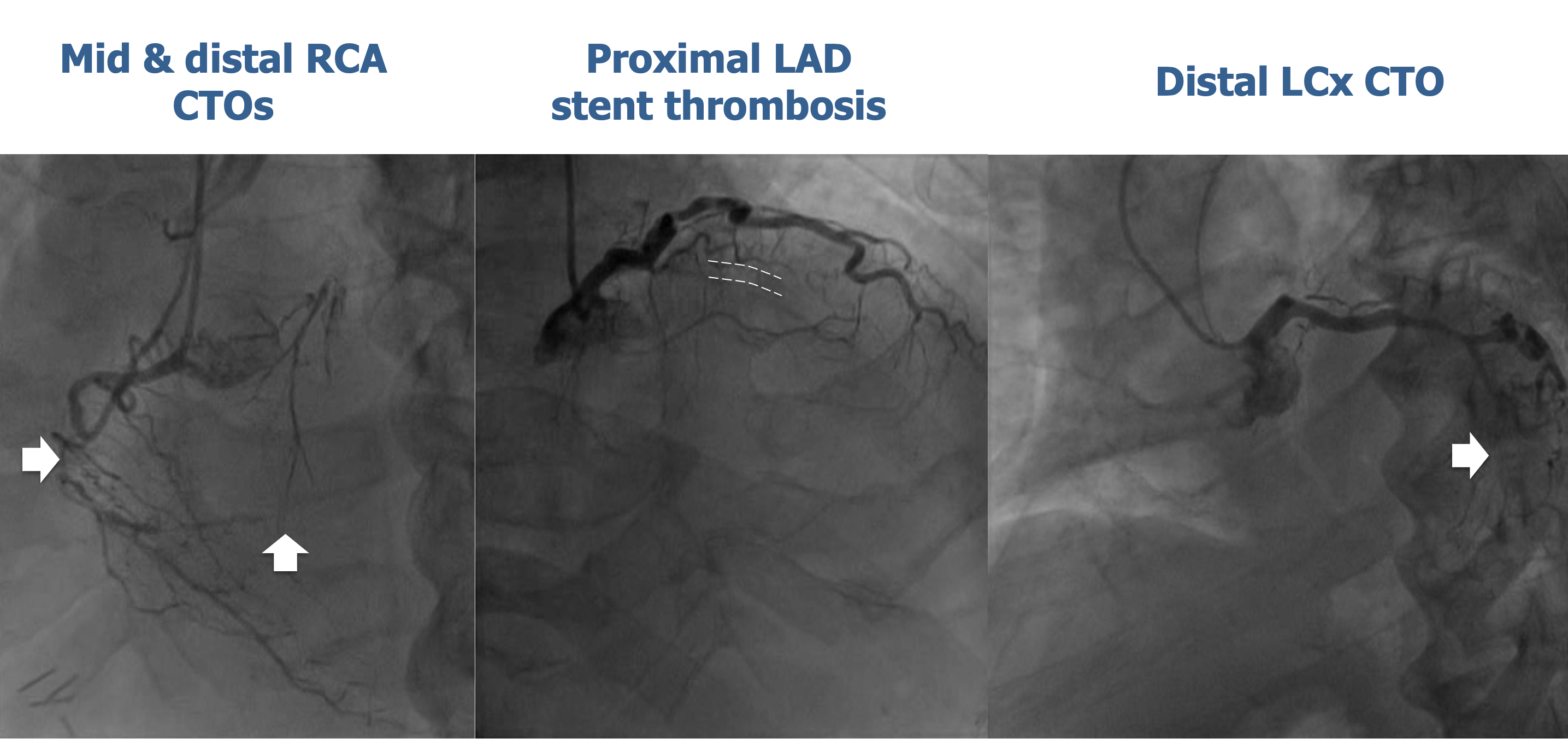
Five hours after transarterial embolization, he developed acute-onset chest pain. The ECG revealed new ST elevation in the precordial leads, accompanied by elevation of troponin I levels. Emergent coronary angiography revealed acute thrombotic occlusion in the proximal LAD stent and CTOs in the LCx and the RCA. Aspiration thrombectomy and small balloon dilation were performed to restore LAD flow with a reduced dose heparin to avoid recurrent bleeding.
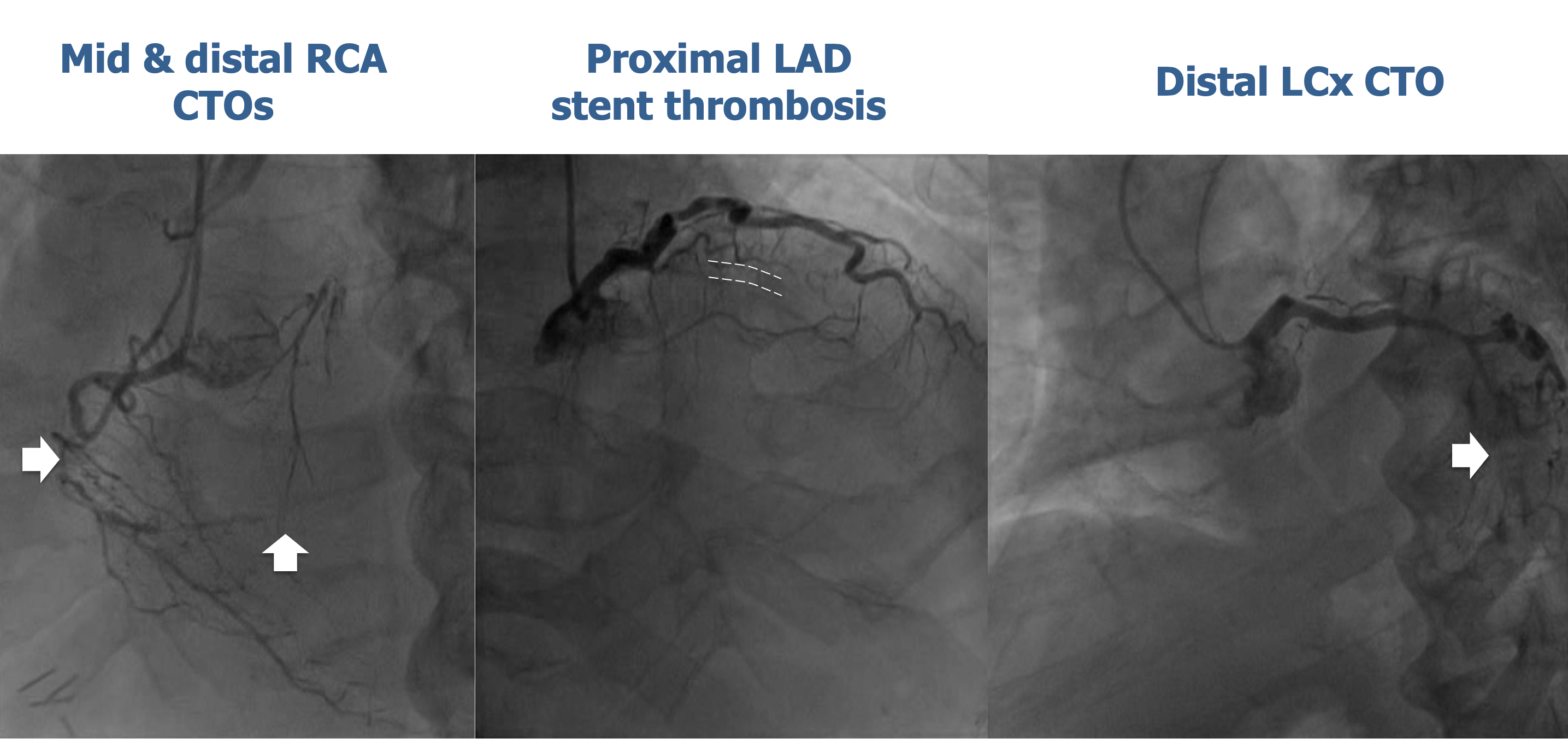
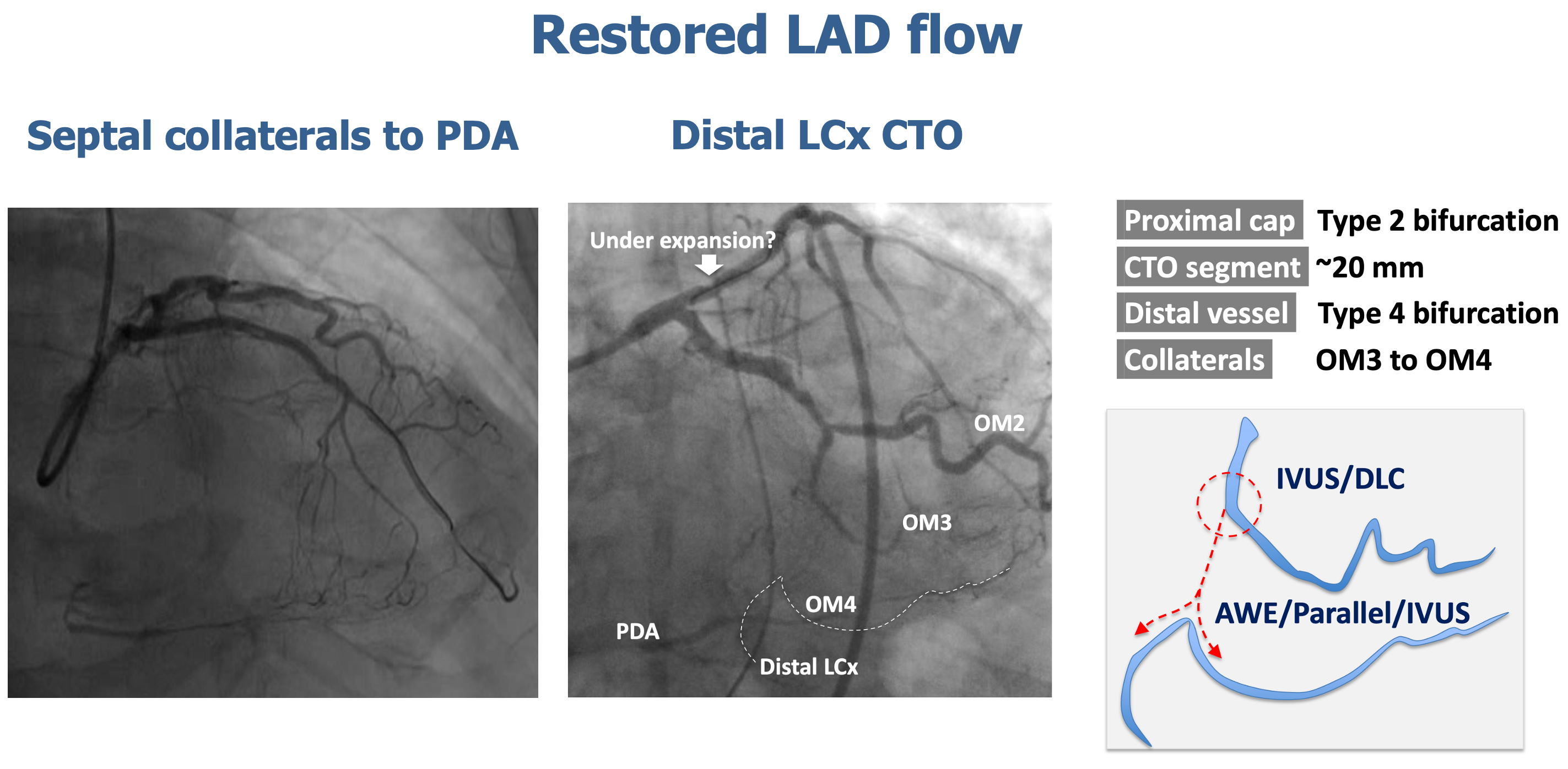
Relevant Catheterization Findings
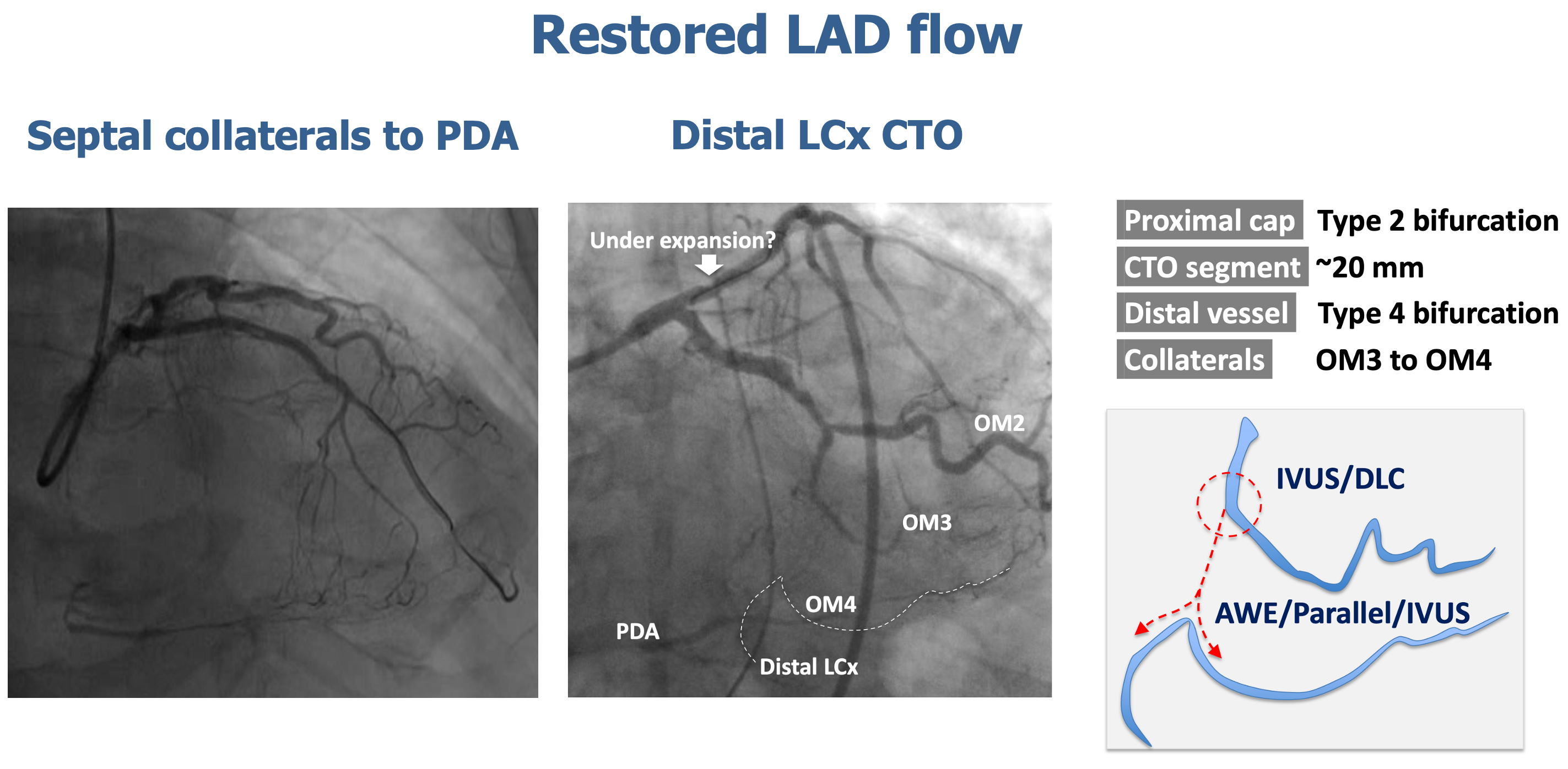
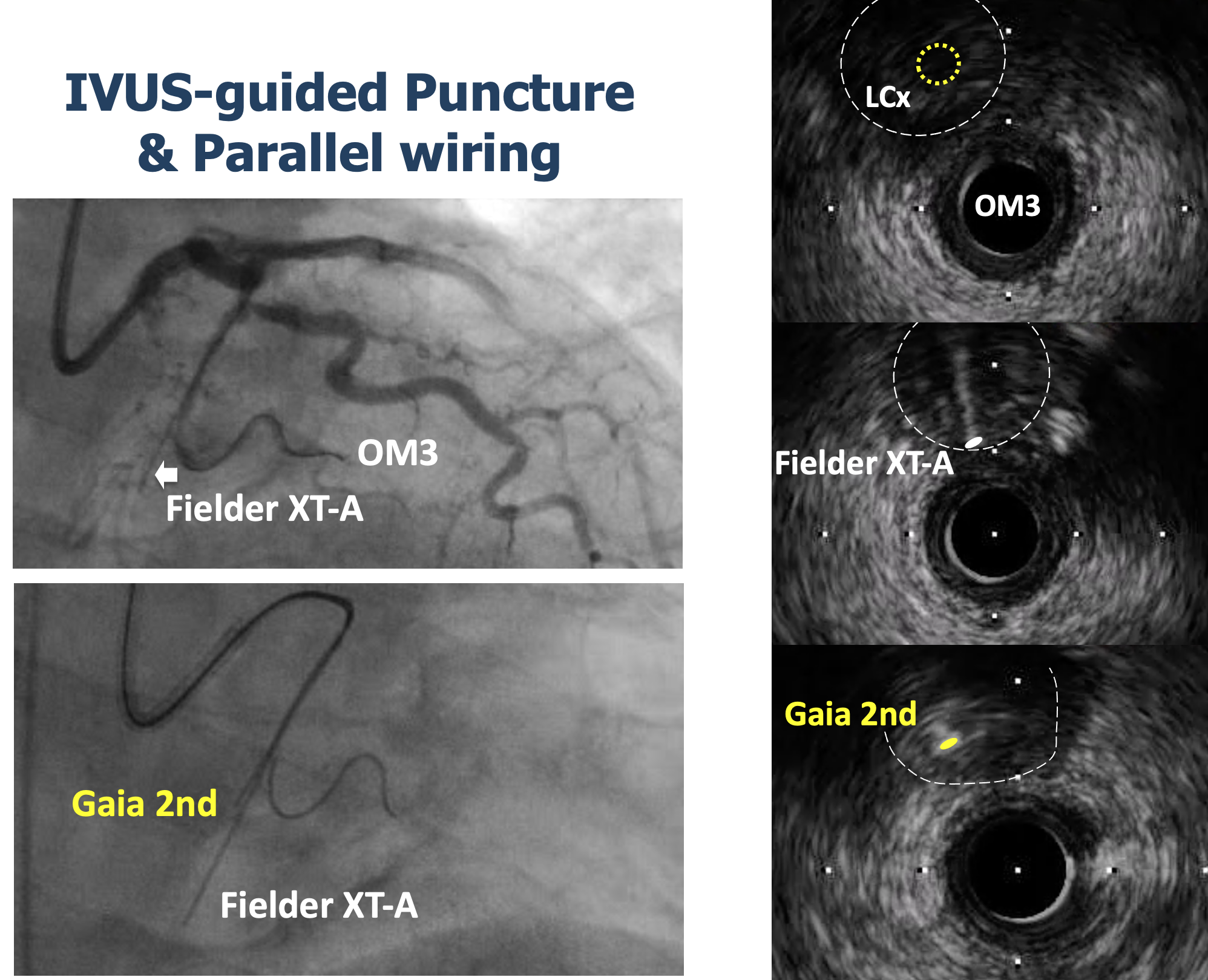
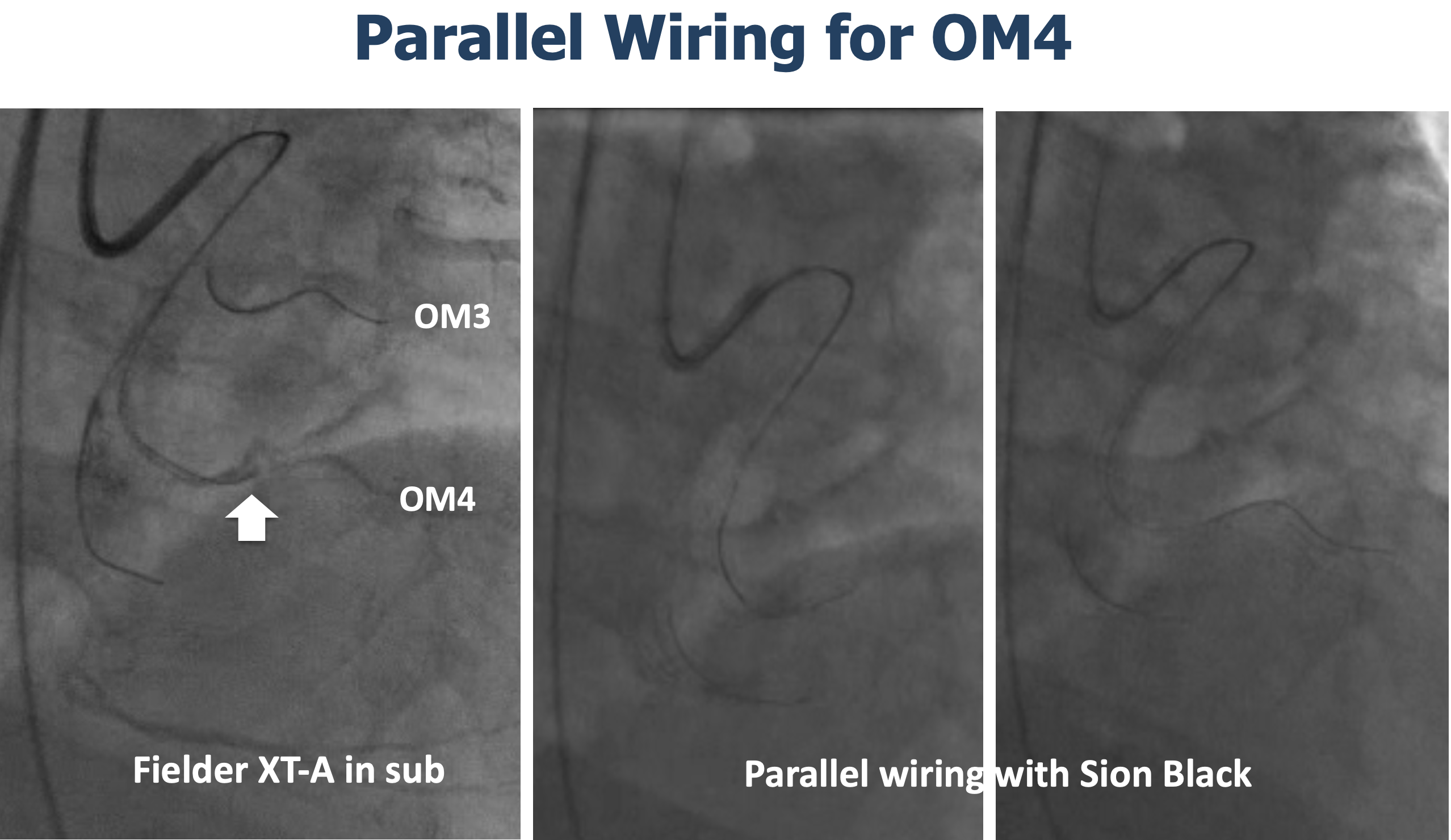
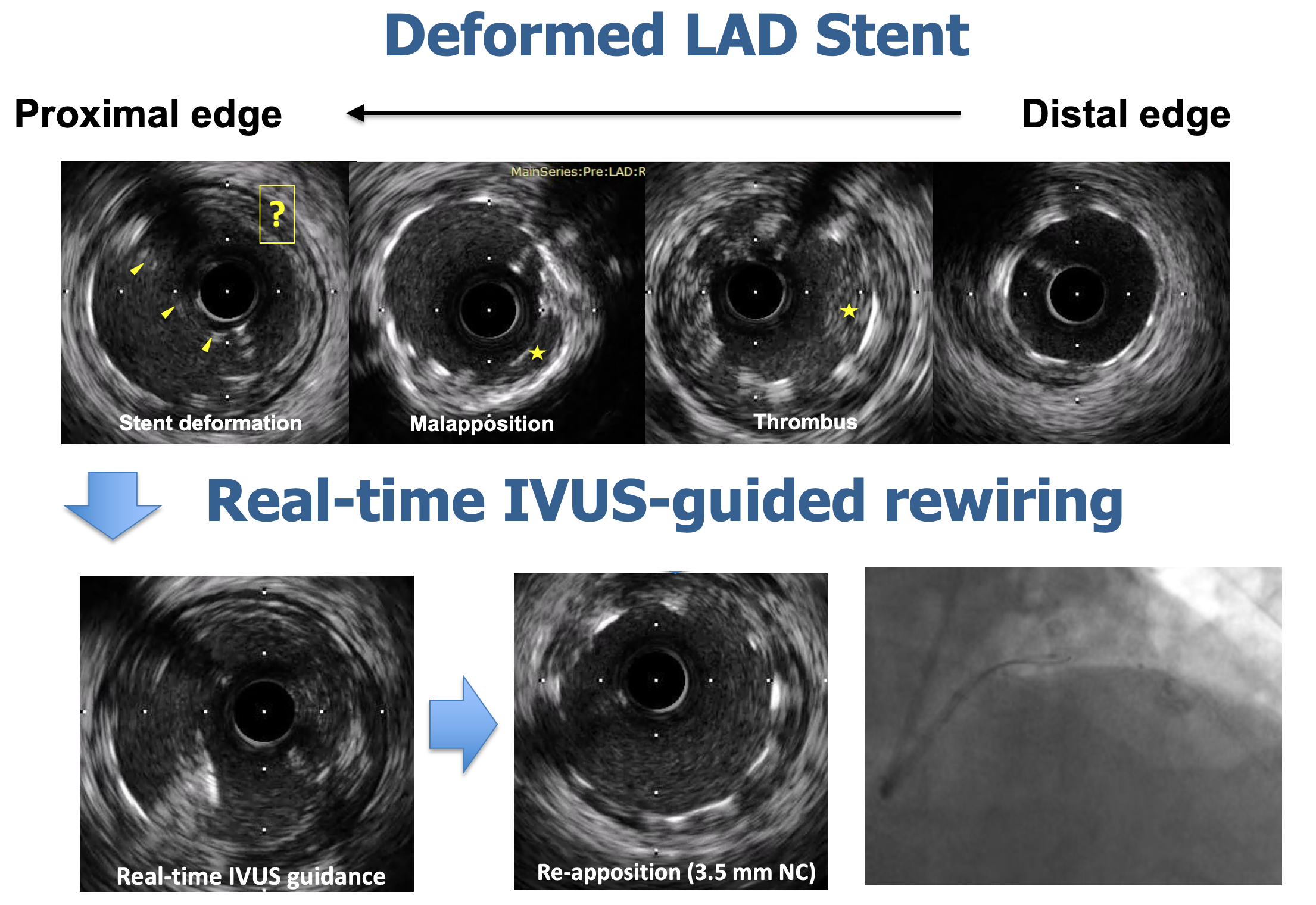
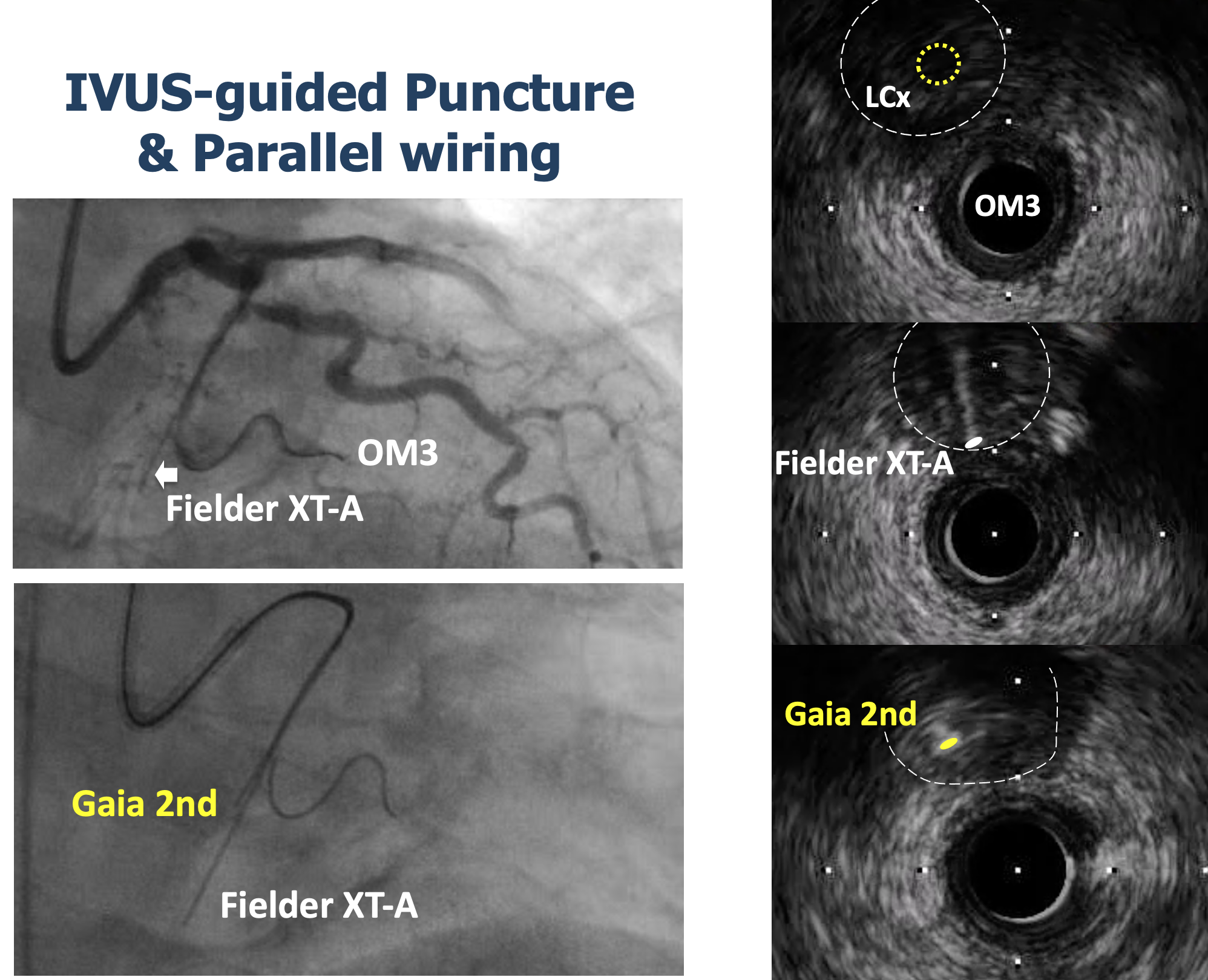
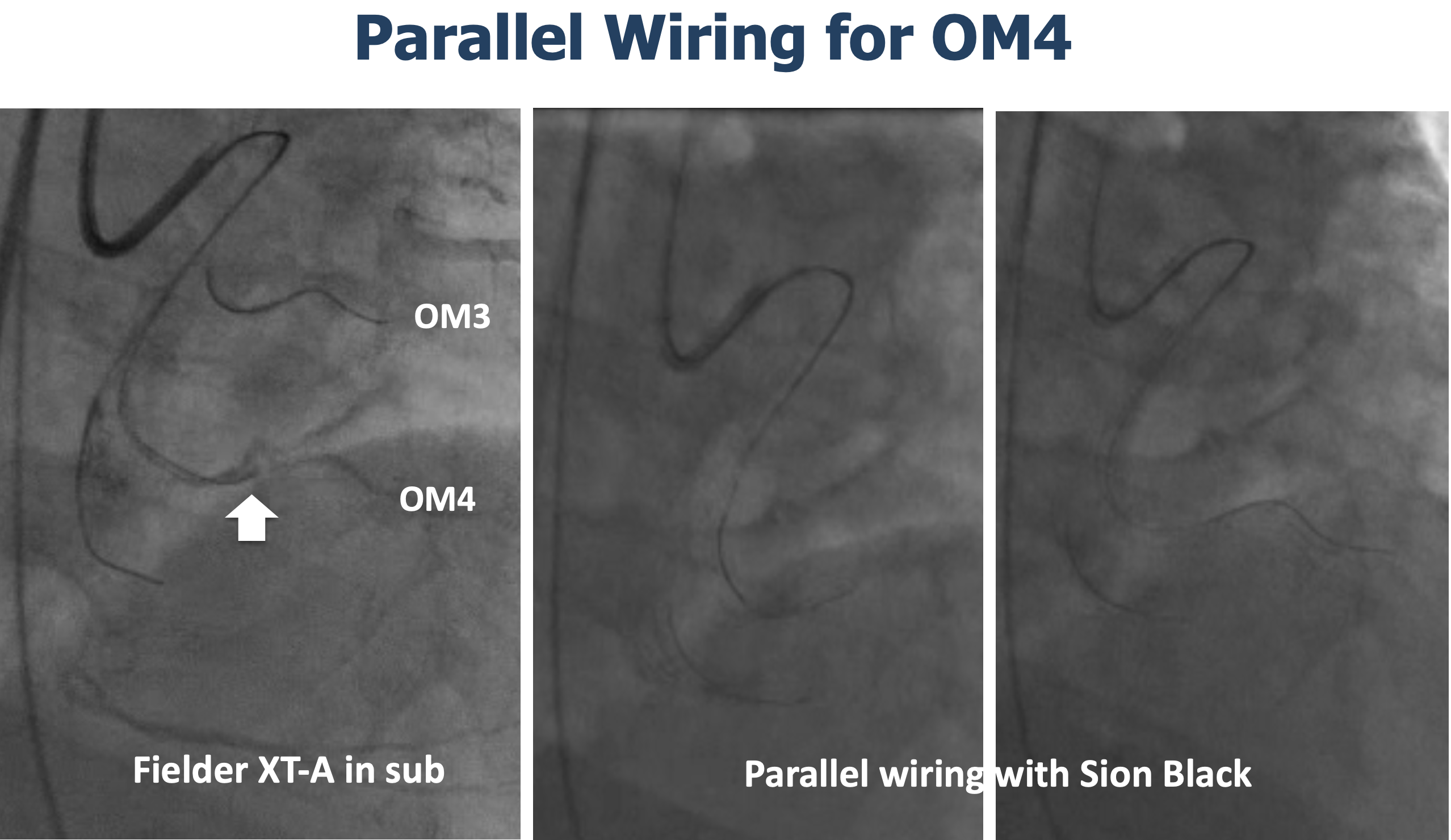
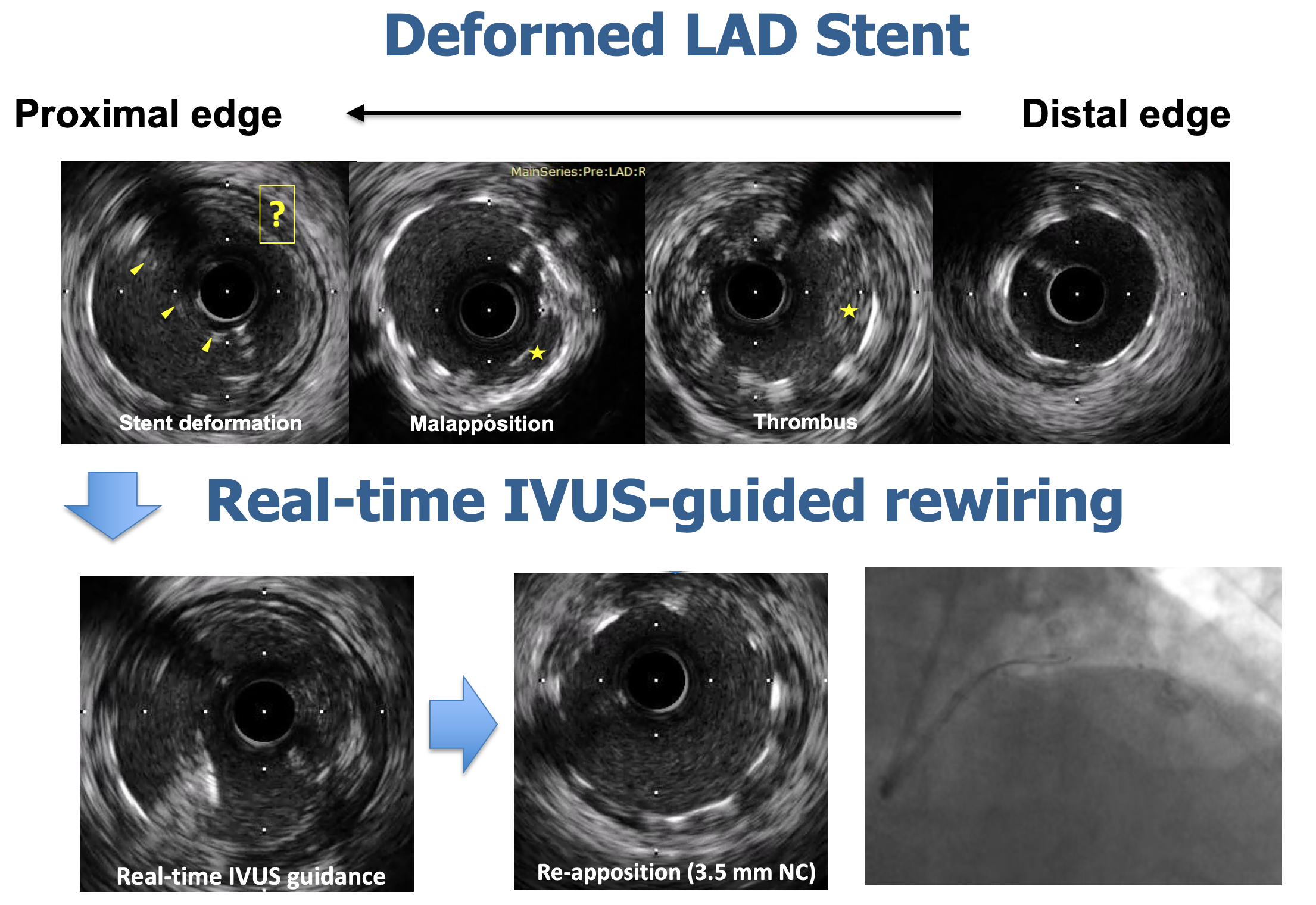
After stabilization, the patient underwent a staged procedure to assess the LAD stent and to address the LCx CTO. The proximal cap of the LCx CTO was ambiguous (type 2 bifurcation CTO). Proximal cap puncture was performed with IVUS-guided parallel wiring. Another parallel wiring was successfully performed to enter distal true lumen. IVUS revealed deformed proximal LAD stent struts, which were restored under realtime IVUS-guided wiring.
Interventional Management
Procedural Step
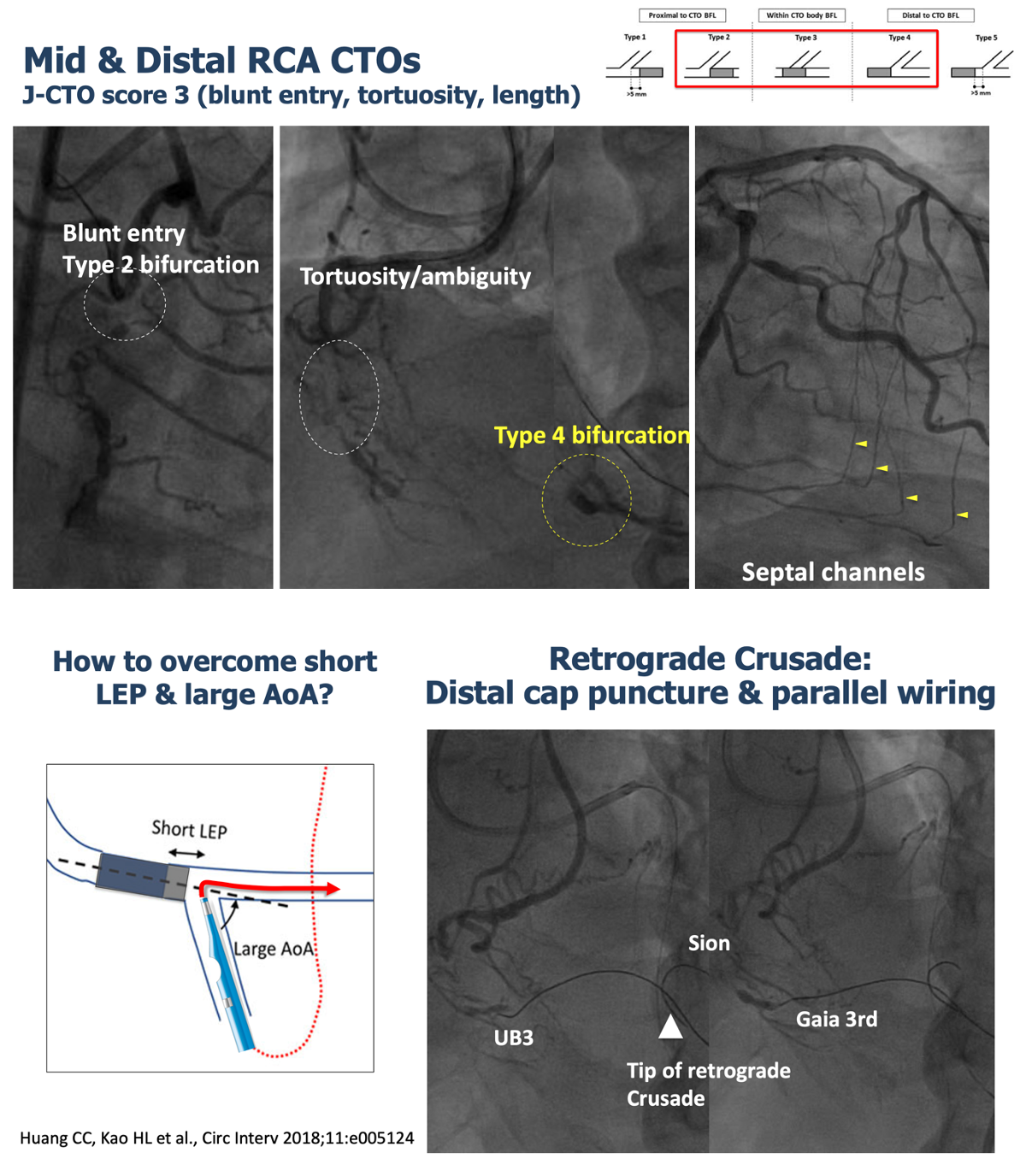
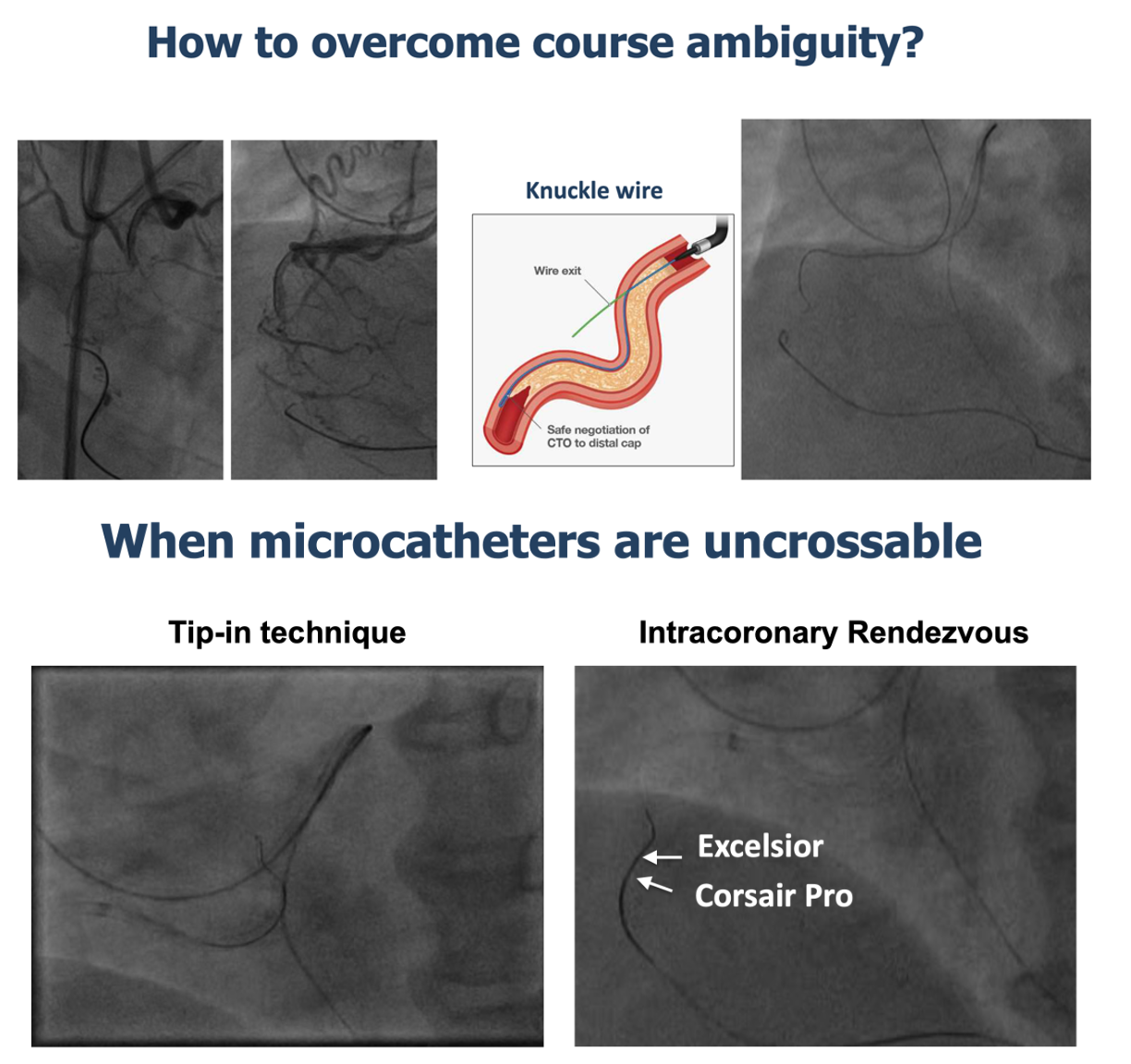
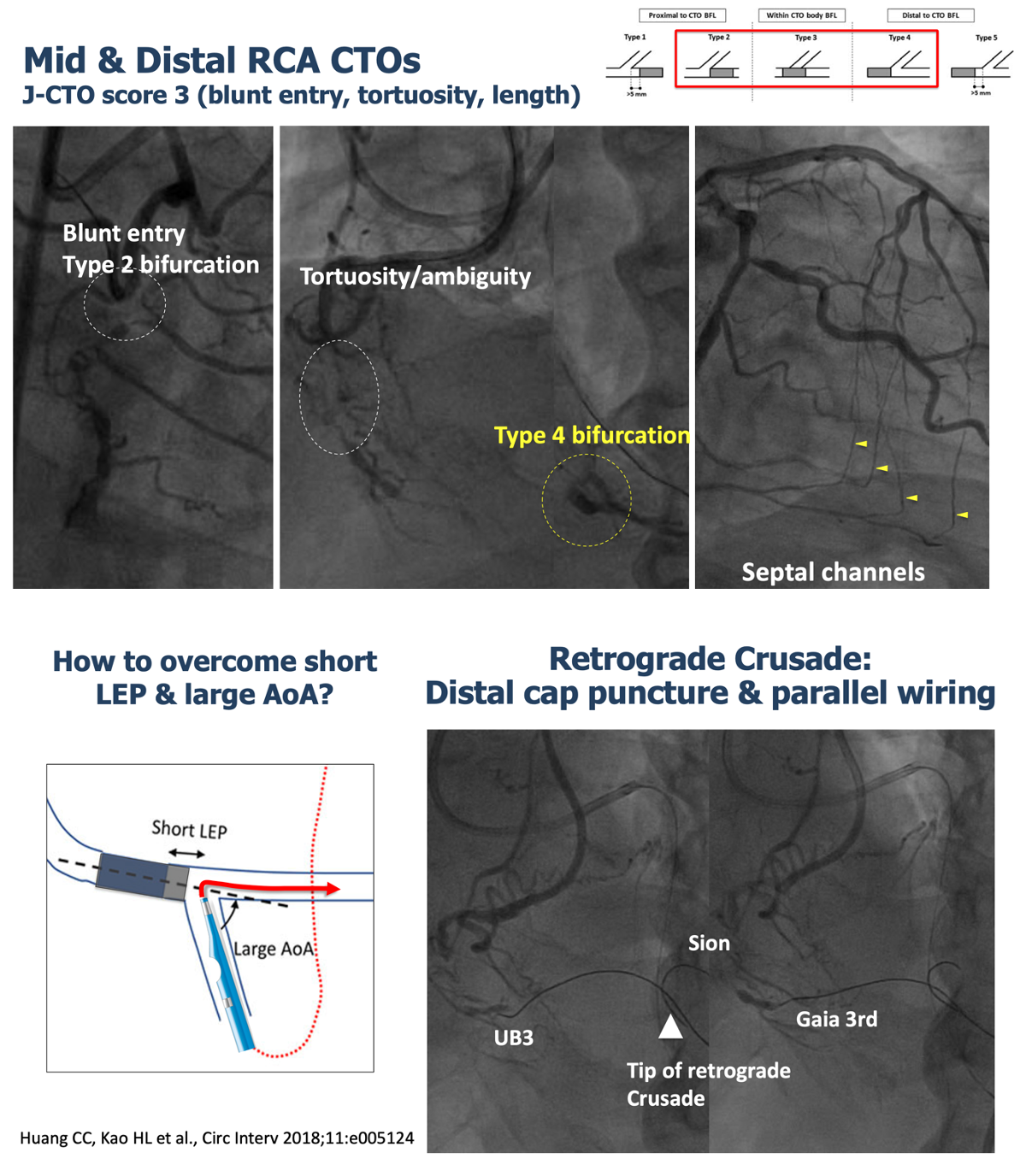
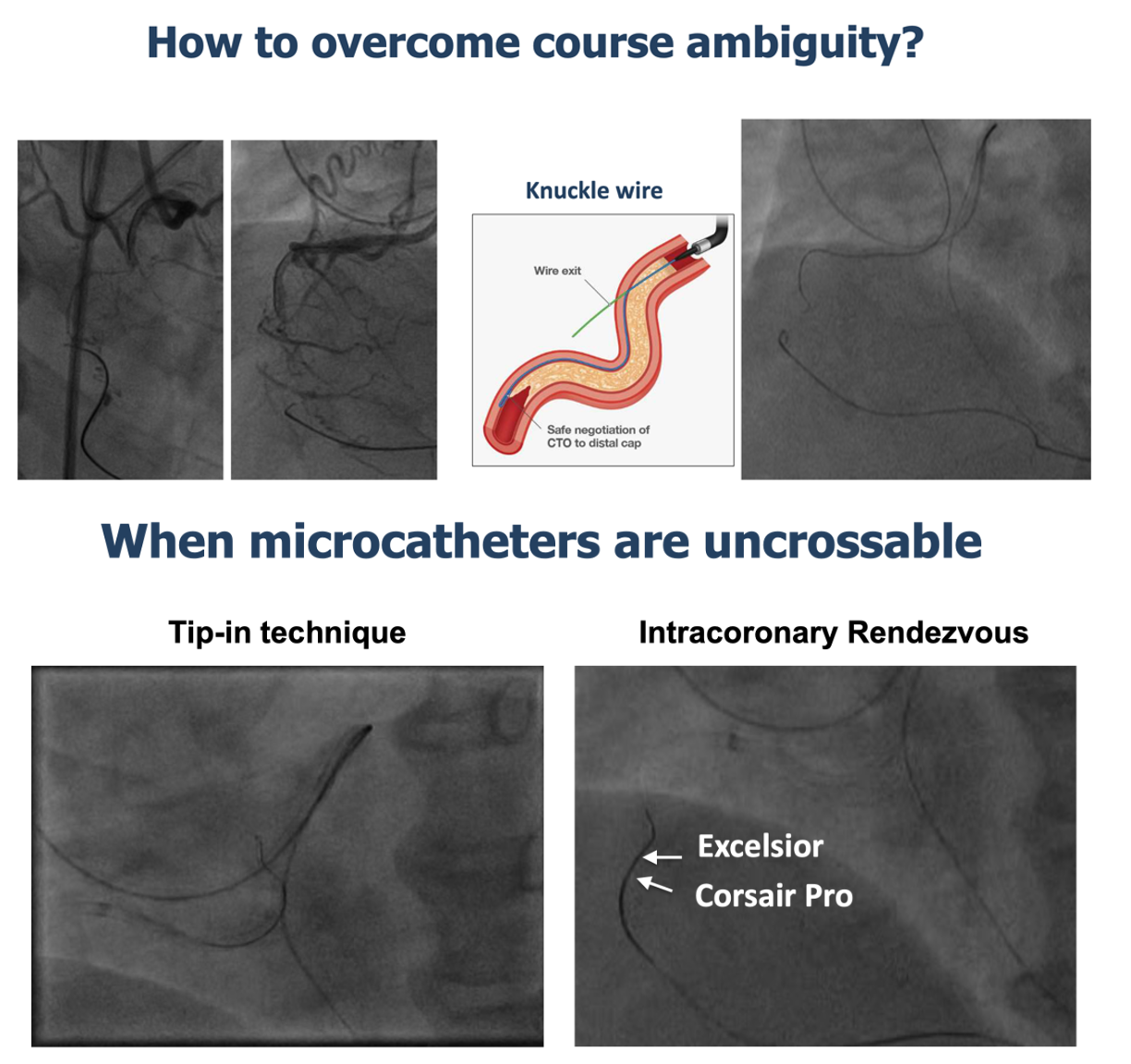
Another staged procedure was conducted for the mid and distal RCA CTOs. Following antegrade preparation, a retrograde approach was employed via the septal collateral channel. To address the large angle of attack at the exit of the distal RCA CTO at the bifurcation, a dual lumen catheter was retrogradely utilized. Successful retrograde wiring reached a contrast island at the junction of segments 2 and 3. Navigating the tortuosity of the mid RCA CTO involved the use of a retrograde knuckle wire. Tip-in and Intracoronary Rendezvous techniques become necessary as both the antegrade and retrograde microcatheters encountered difficulty crossing the mid RCA CTO. IVUS revealed intraplaque tracking in both the mid and distal RCA CTOs.
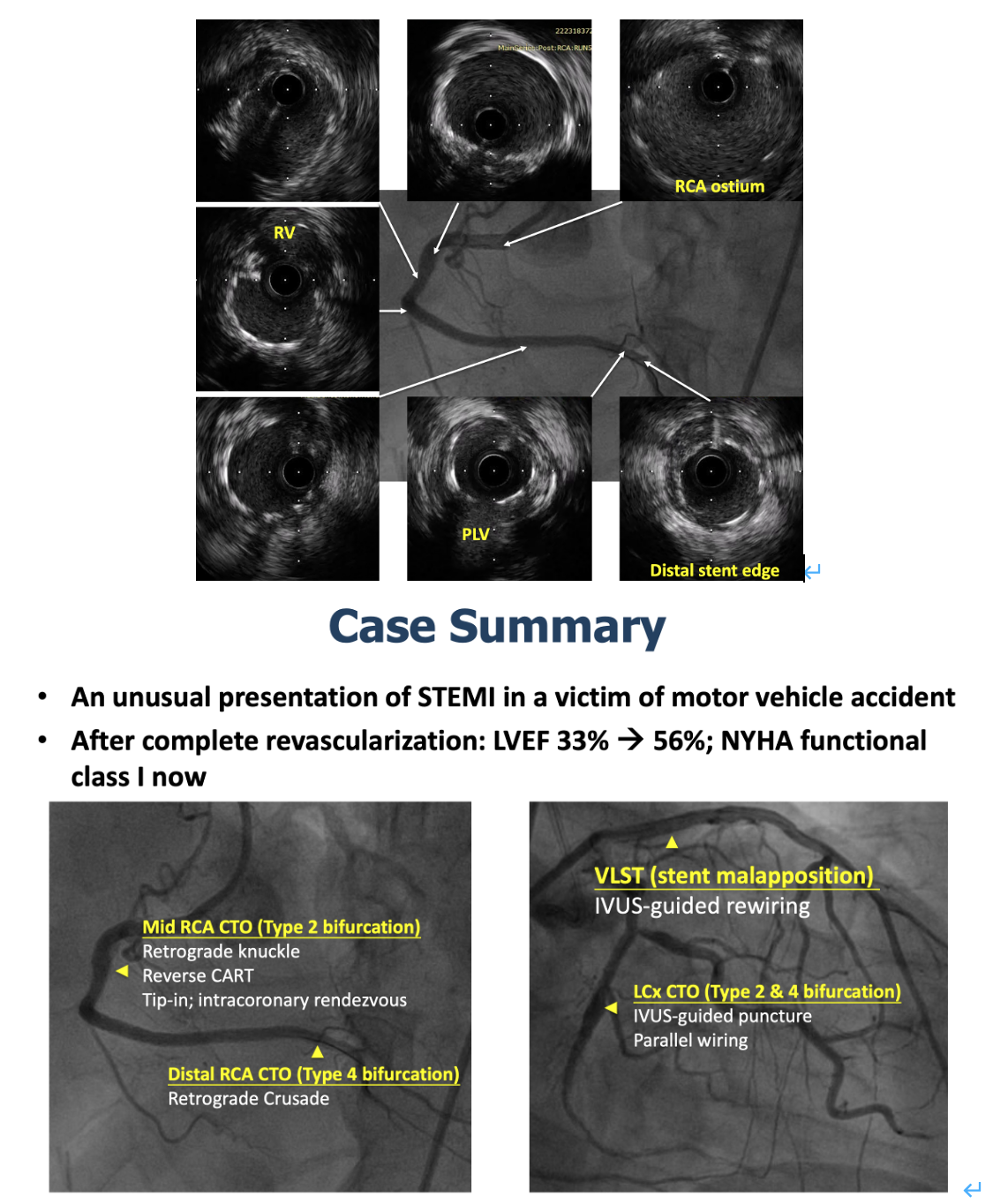
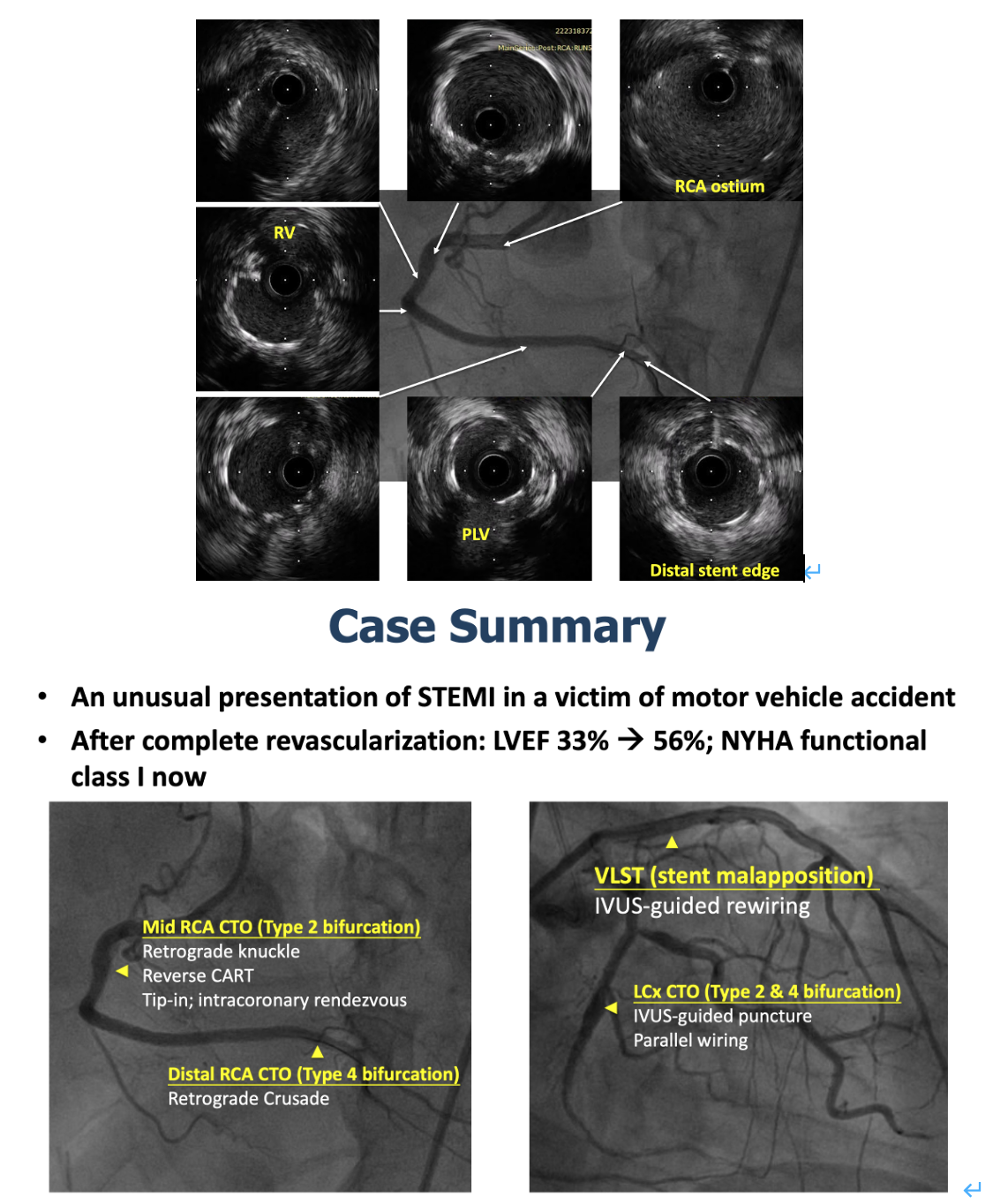
Case Summary
1. The cause of LAD stent thrombosis in the patient may be due to interrupted antiplatelet agent and systemic inflammation in the presence of malapposed stent struts.2. Revascularization of multivessel CTO should be considered to avoid catastrophic outcomes that may occur in the last remaining coronary artery.

