Lots of interesting abstracts and cases were submitted for TCTAP 2024. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-167
Clinical Nuances in the Management of Coexisting Diffuse and Focal Coronary Artery Disease: A Case of Angiographically Underestimated Lesions With Significant Physiological Impact
By Minju Han, Doyeon Hwang, Bon-Kwon Koo
Presenter
Minju Han
Authors
Minju Han1, Doyeon Hwang1, Bon-Kwon Koo1
Affiliation
Seoul National University Hospital, Korea (Republic of)1,
View Study Report
TCTAP C-167
Coronary - Imaging & Physiology - FFR
Clinical Nuances in the Management of Coexisting Diffuse and Focal Coronary Artery Disease: A Case of Angiographically Underestimated Lesions With Significant Physiological Impact
Minju Han1, Doyeon Hwang1, Bon-Kwon Koo1
Seoul National University Hospital, Korea (Republic of)1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
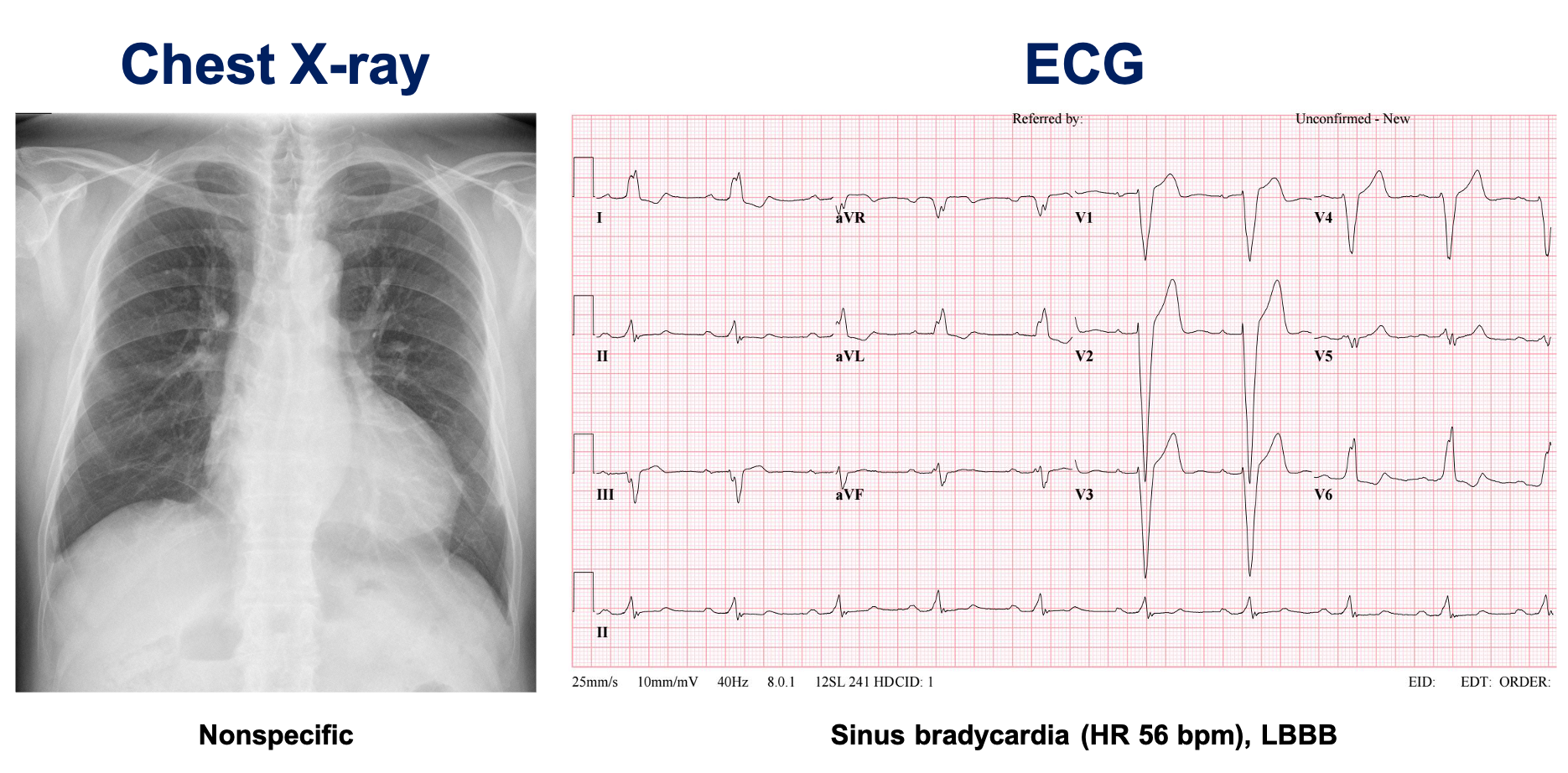
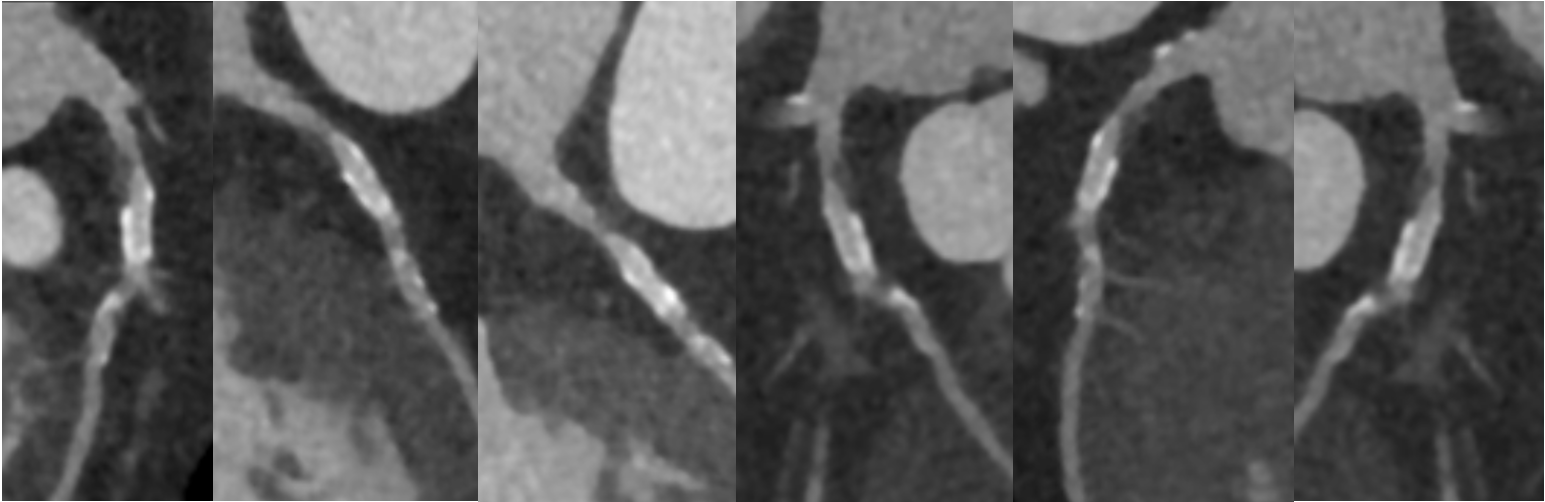
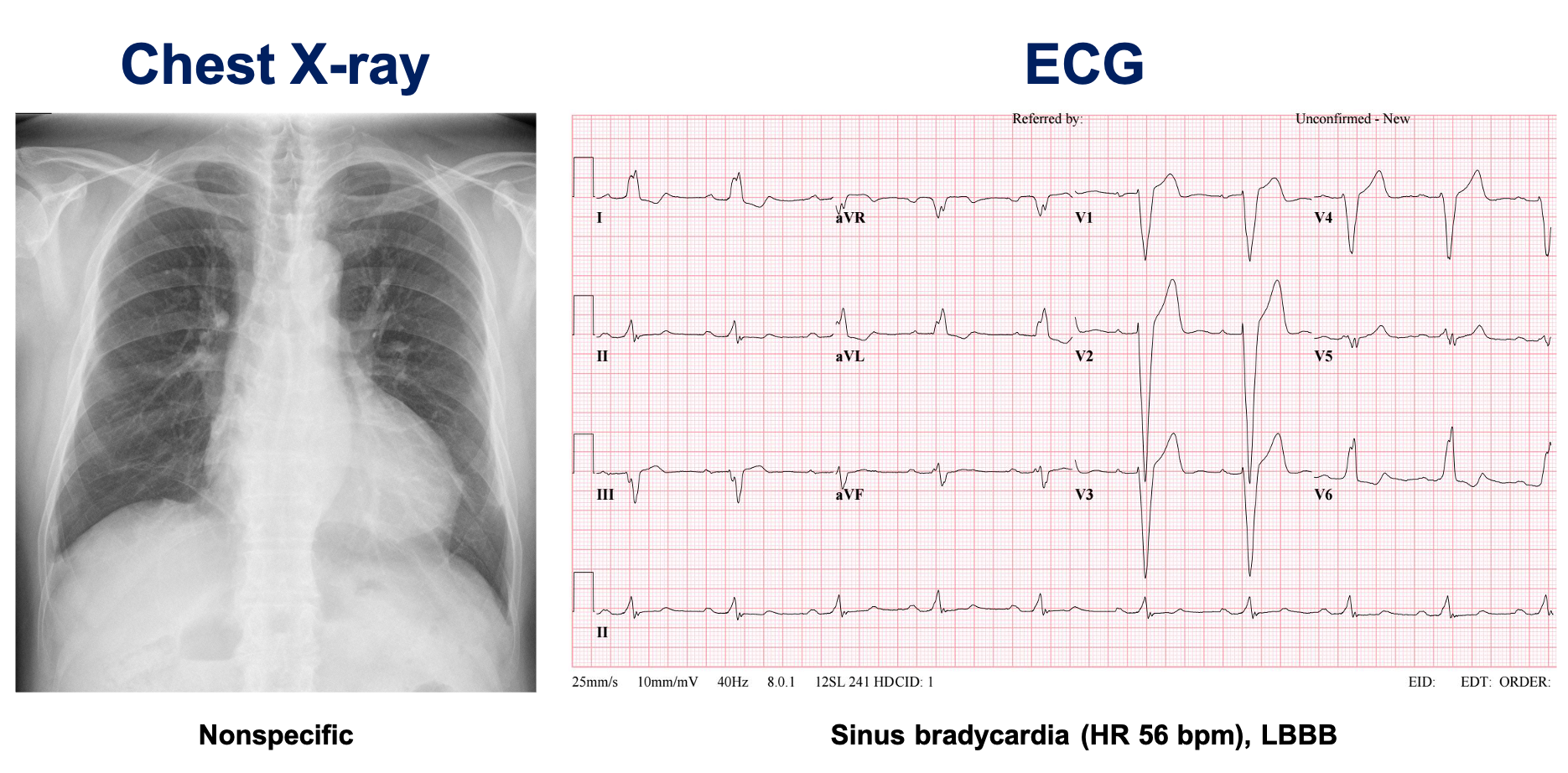
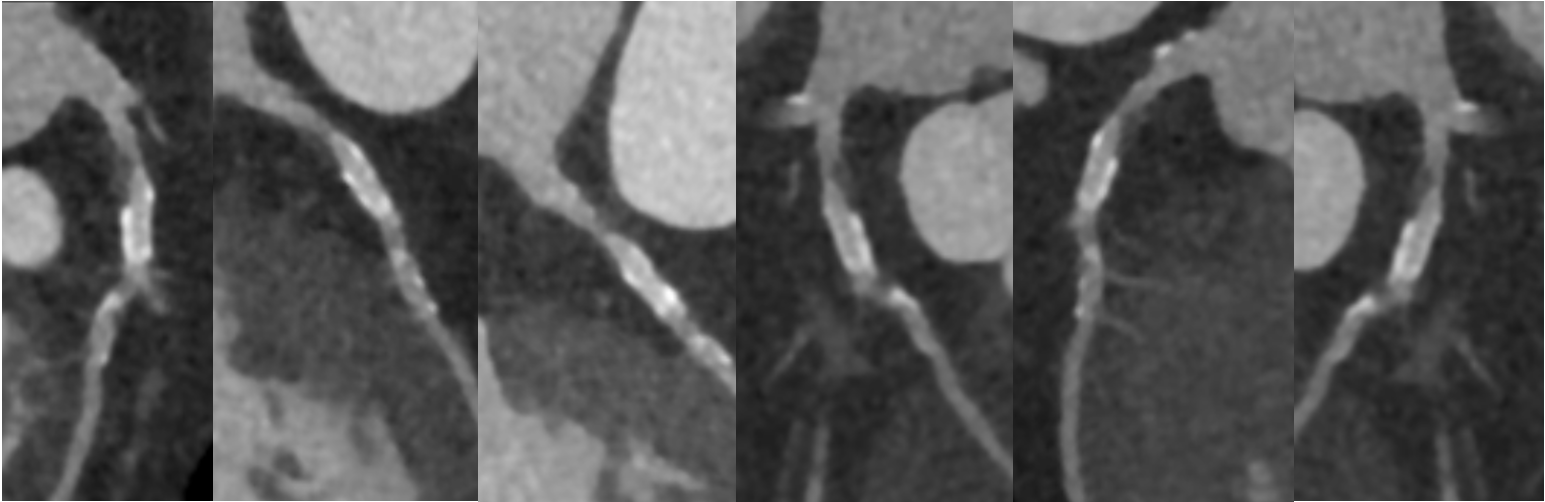
A 70-year-old male visited the outpatient clinic with typical angina that worsened with exertion and resolved after 10 minutes of rest. He had a medical history of hypertension, chronic kidney disease, bronchiectasis and gout. His ECG showed LBBB pattern. On CT coronary angiography, there was an 8-90% stenosis with a vulnerable plaque at the proximal LAD, and also a 70% mid-LAD stenosis. Echocardiography showed reduced systolic function (LVEF=40%) with global hypokinesia and dyssynchronous LV.


Relevant Test Results Prior to Catheterization
Relevant Catheterization Findings
Interventional Management
Procedural Step
Inconsistent with previous CCTA, his invasive CAG showed only angiographically insignificant lesions of 40% proximal LAD stenosis and diffuse downstream luminal irregularities. After reviewing his CT images, we decided to perform a physiological study with FFR.
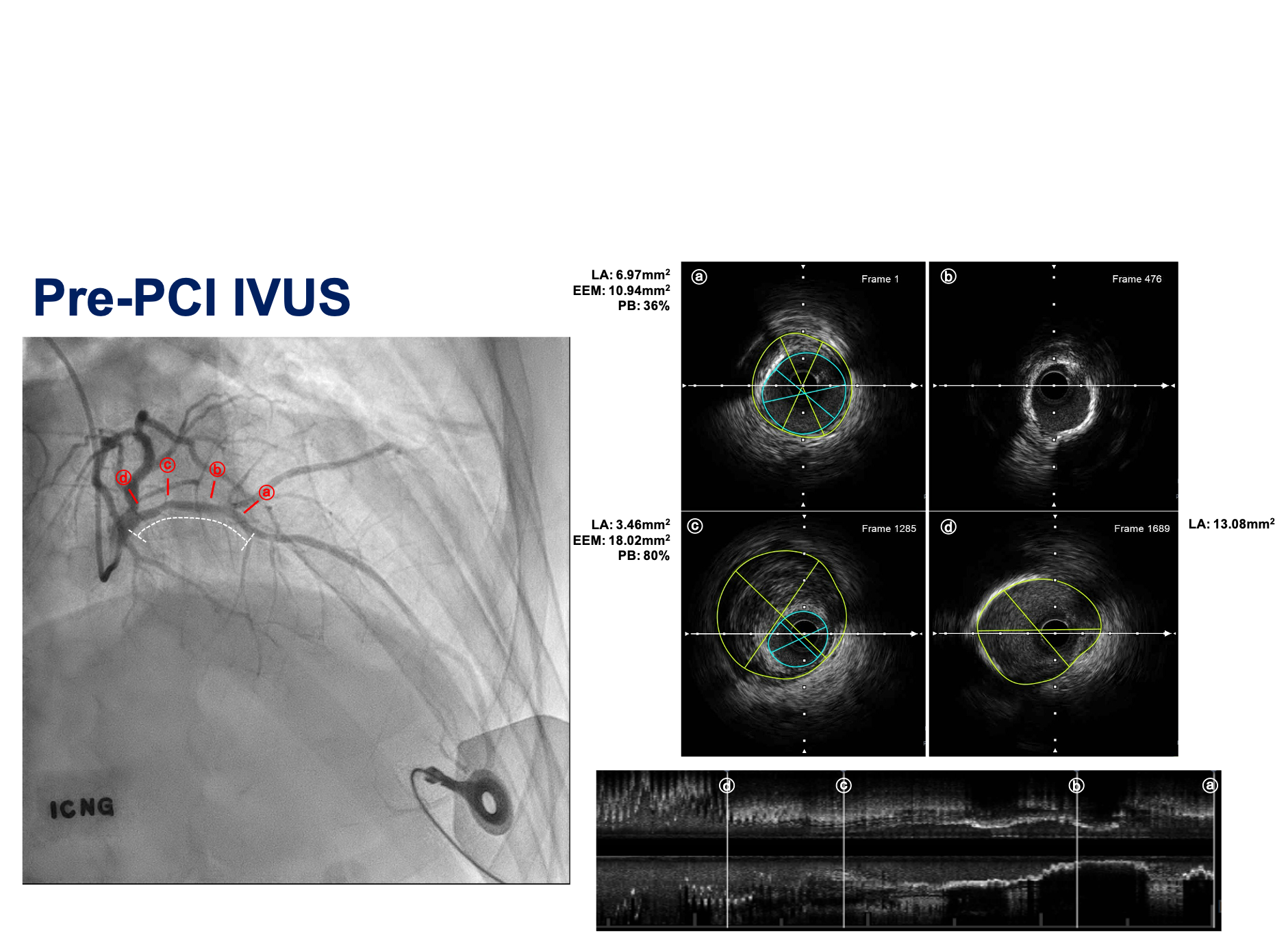
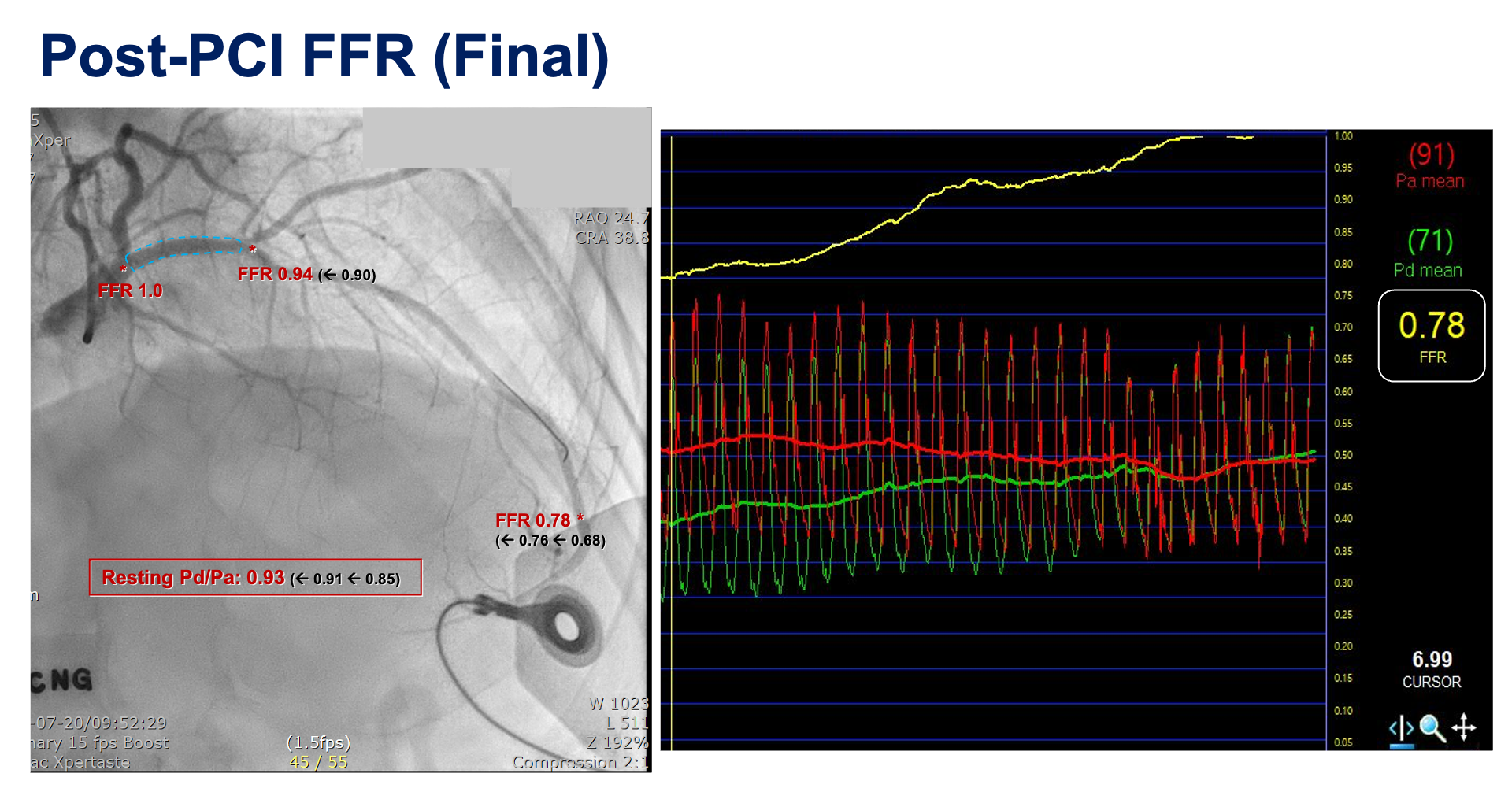
The fractional functional reserve (FFR) at the distal LAD was 0.68; a large step-up on pullback was observed at the proximal LAD lesion where a focal vulnerable plaque was located on CT. After the decision to proceed with PCI, intravascular ultrasound was used to evaluate the lesion in detail: a dense atheromatous plaque at the proximal LAD lesion with a plaque burden of 80% and diffuse circumferential calcification distal to the lesion were observed. The patient was treated with a Xience Skypoint 3.0x15 mm DES after careful lesion preparation with a 2.5x15 mm Angiosculpt scoring balloon.The stent was well-apposed and dilated on post-PCI IVUS with an MSA of 6.50 mm2; however, post-PCI FFR was still 0.76 at the distal LAD and a significant trans-stent step-up of 0.1 was observed (stent distal: 0.90, stent proximal: 1.00). We performed adjunctive balloon dilatation of the stent with a 3.5x10 mm noncompliant balloon (up to 18 atm, diameter 3.63 mm). The final FFR was still 0.78 at the distal LAD without a definite step-up at pullback, indicating residual diffuse disease, but ∆FFR across the stent was reduced to 0.06.

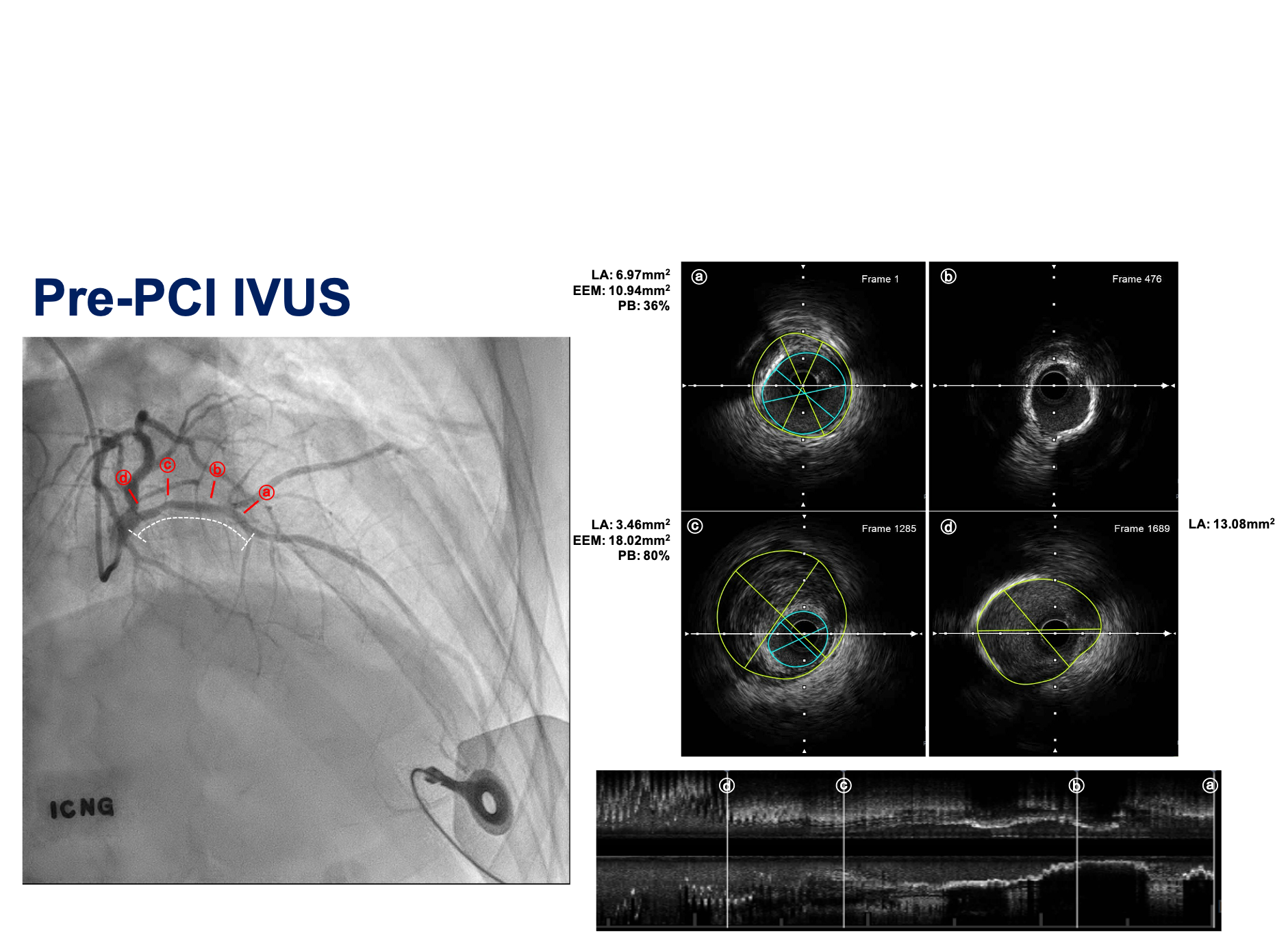
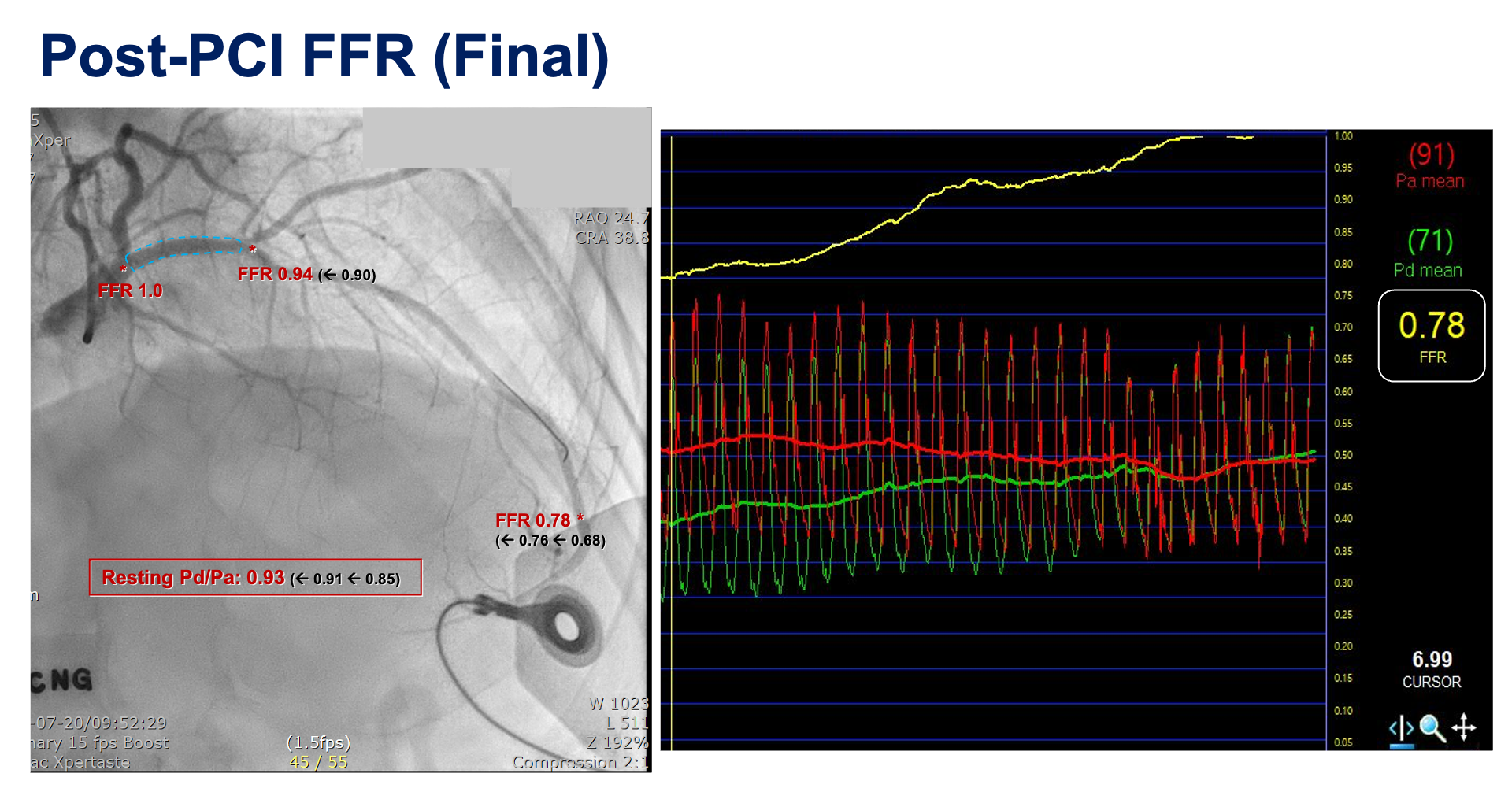
The fractional functional reserve (FFR) at the distal LAD was 0.68; a large step-up on pullback was observed at the proximal LAD lesion where a focal vulnerable plaque was located on CT. After the decision to proceed with PCI, intravascular ultrasound was used to evaluate the lesion in detail: a dense atheromatous plaque at the proximal LAD lesion with a plaque burden of 80% and diffuse circumferential calcification distal to the lesion were observed. The patient was treated with a Xience Skypoint 3.0x15 mm DES after careful lesion preparation with a 2.5x15 mm Angiosculpt scoring balloon.The stent was well-apposed and dilated on post-PCI IVUS with an MSA of 6.50 mm2; however, post-PCI FFR was still 0.76 at the distal LAD and a significant trans-stent step-up of 0.1 was observed (stent distal: 0.90, stent proximal: 1.00). We performed adjunctive balloon dilatation of the stent with a 3.5x10 mm noncompliant balloon (up to 18 atm, diameter 3.63 mm). The final FFR was still 0.78 at the distal LAD without a definite step-up at pullback, indicating residual diffuse disease, but ∆FFR across the stent was reduced to 0.06.

Case Summary
Selecting a treatment strategy for patients with diffuse and focal coronary artery disease is a challenge requiring an individualized approach. In this case, we encountered a lesion that appeared to be angiographically insignificant, but demonstrated significant significance on advanced intravascular imaging and physiological assessment. PCI was done for the focal lesion, given its potential impact on the patient's clinical outcome. We planned an outpatient-based optimal medical therapy first. This case highlights the critical role of comprehensive diagnostics in guiding targeted interventions and underscores the importance of individualized therapy in complex coronary disease.

