Lots of interesting abstracts and cases were submitted for TCTAP 2024. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-210
Patient-Specific Computer Simulation of Virtual Balloon Pre-dilatation and Accurate Assessment of a High-Risk Patient Before Transcatheter Aortic Valve Replacement
By Xinlei Wu, Zhu Jinyun, Xing Liu, YiQiu Jiang, Yongfang Liu, Daozhu Wu, Xinmin Zhang, Lianpin Wu
Presenter
Xinlei Wu
Authors
Xinlei Wu1, Zhu Jinyun1, Xing Liu1, YiQiu Jiang1, Yongfang Liu2, Daozhu Wu1, Xinmin Zhang1, Lianpin Wu1
Affiliation
The Second Affiliated Hospital of Wenzhou Medical University, China1, Second Affiliated Hospital Wenzhou Medical University , China2,
View Study Report
TCTAP C-210
Structural - Aortic Valve Intervention - Complex TAVR
Patient-Specific Computer Simulation of Virtual Balloon Pre-dilatation and Accurate Assessment of a High-Risk Patient Before Transcatheter Aortic Valve Replacement
Xinlei Wu1, Zhu Jinyun1, Xing Liu1, YiQiu Jiang1, Yongfang Liu2, Daozhu Wu1, Xinmin Zhang1, Lianpin Wu1
The Second Affiliated Hospital of Wenzhou Medical University, China1, Second Affiliated Hospital Wenzhou Medical University , China2,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
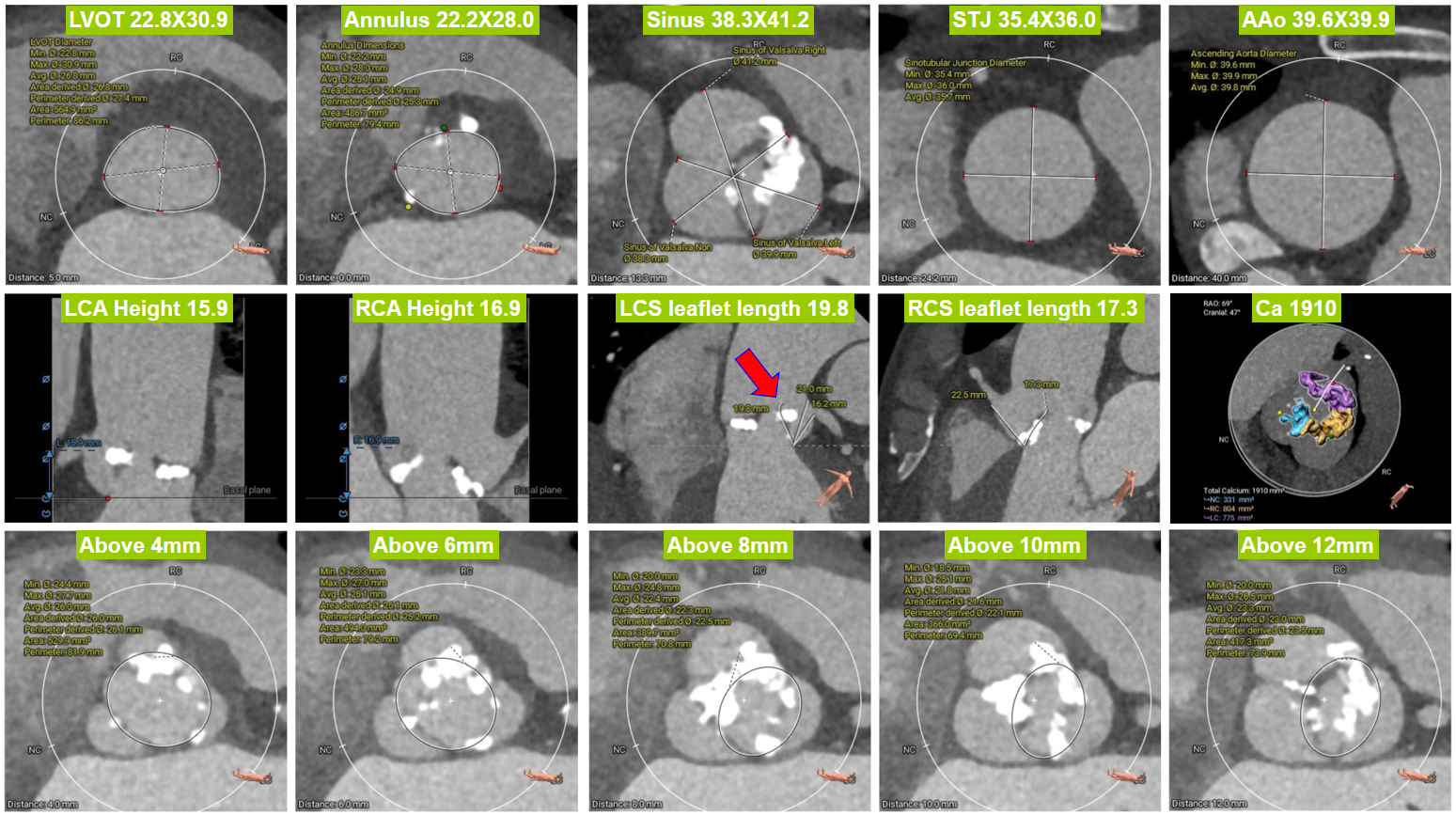
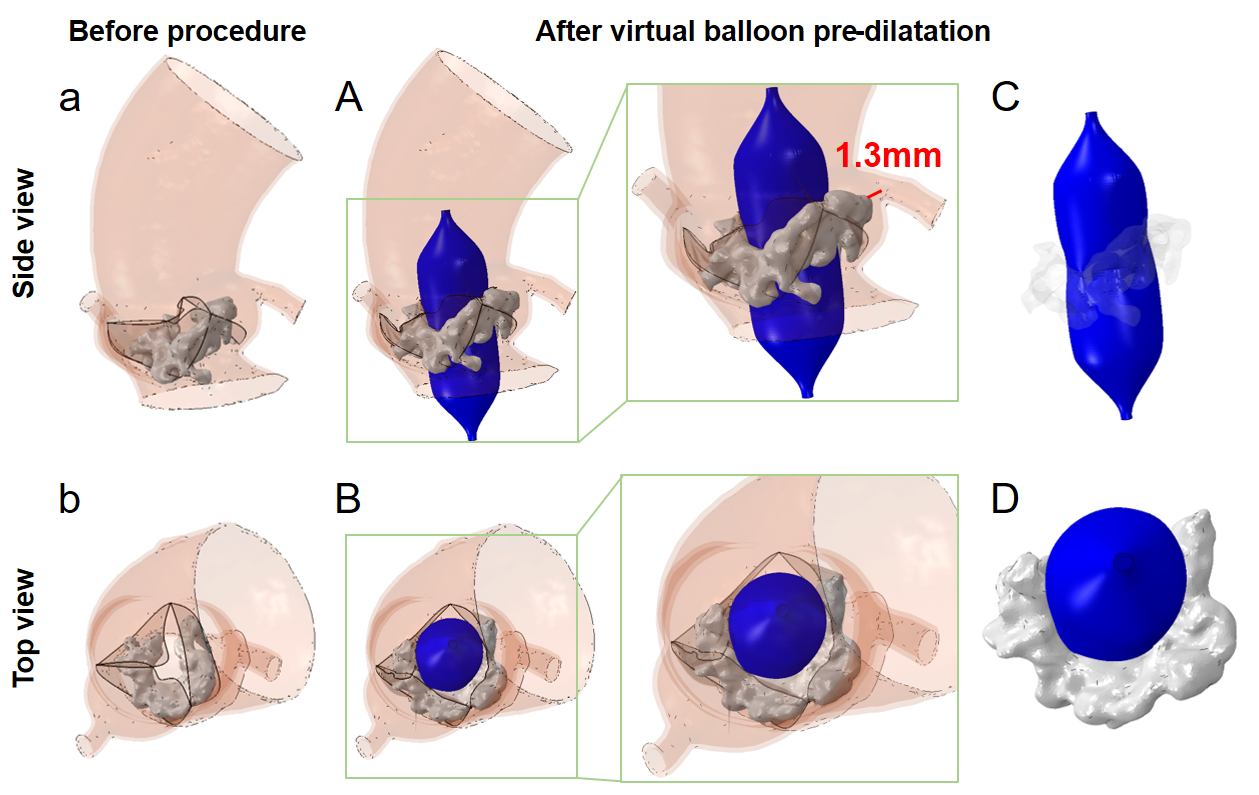
A 59-year-old man (H: 168cm, W: 56kg, BMl: 19.84) was referred to our hospital due to recurrent dyspnea for the past two weeks and lower limb edema for three days. Echo revealed that he had a bicuspid aortic valve (BAV) with severe calcification, severe stenosis, and insufficiency (Fig. 3G) (MPG: 40 mmHg, EF: 31%). CCTA confirmed functioning BAV with severe stenosis and calcification with LVOT 22.8X30.9mm, Annulus 22.2X28.0mm, SoV 38.3X41.2mm, STJ 35.4X36.0mm, and AAo 39.6X39.9mm (Fig. 1).
Relevant Test Results Prior to Catheterization
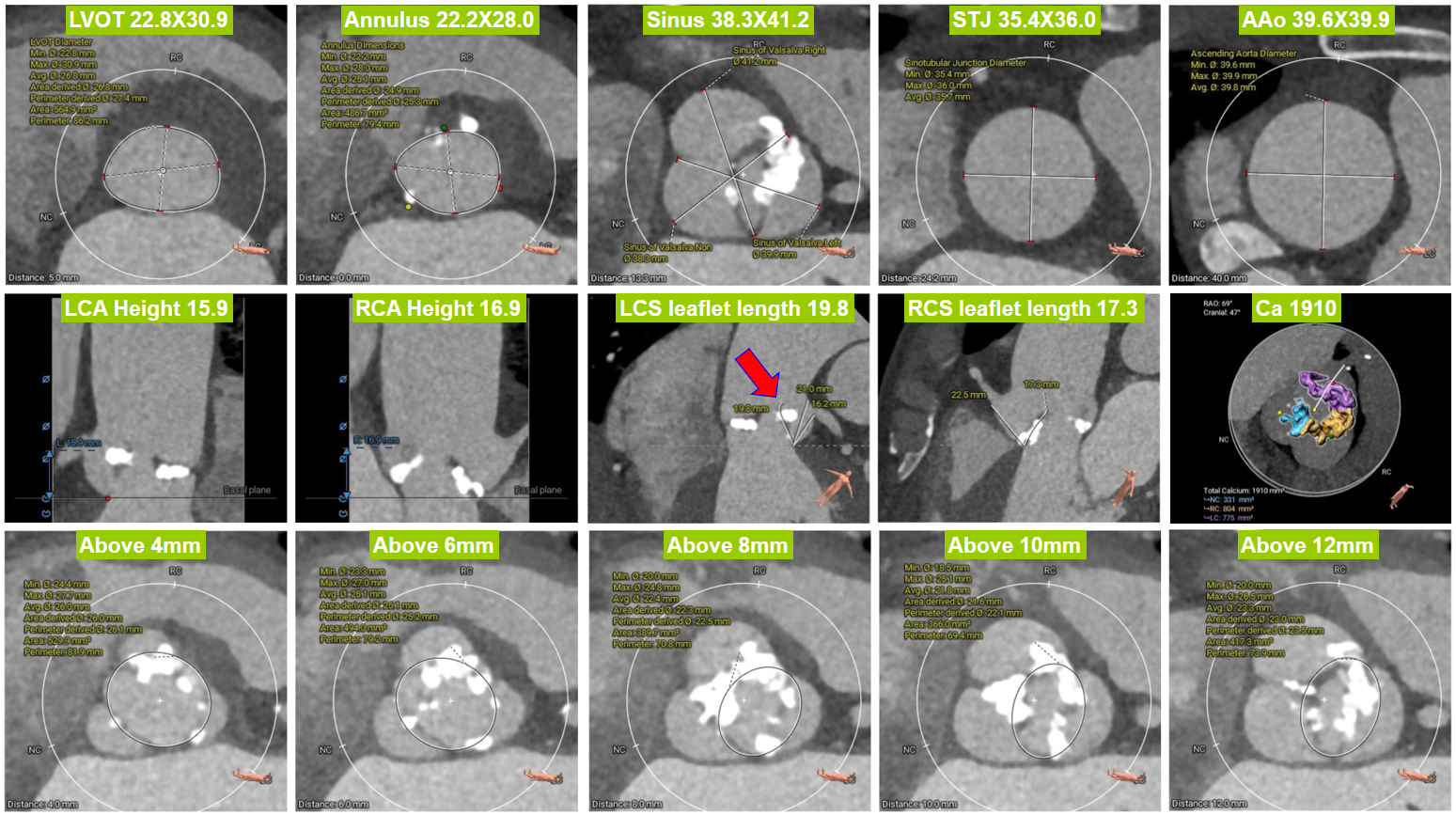
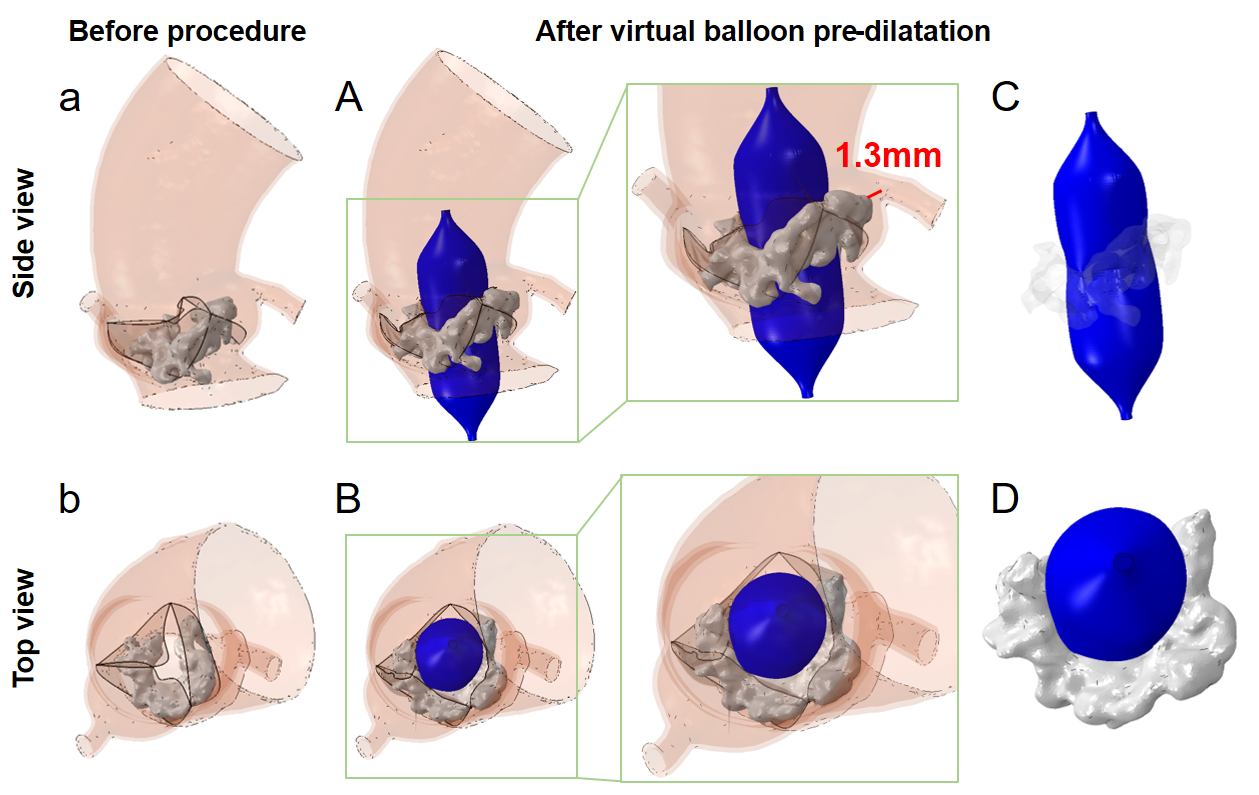
Severe calcification was around leaflet edges with a volume of 1910mm3. LCA height 15.9mm, RCA height 16.9mm. BUT left sinus leaflet length was 19.8mm, longer than distance to lower margin of LCS (16.2mm). A new computer simulation method for virtual balloon pre-dilation was performed on this case using a 20mm balloon and showed effective aortic valve blockage with a mild waist sign around calcification. A 1.3mm gap was observed between calcification and the left coronary artery ostium (Fig. 2A-C).
Relevant Catheterization Findings
A mild waist sign was noted at the right sinus during pre-dilation using a 20mm balloon, tilted towards the left coronary sinus with minor curvature. Severe calcification hindered optimal valve stent expansion, resulting in significant perivalvular leakage. Post-balloon dilation improved prosthesis shape, reducing leakage. TEE was performed several times every few minutes to determine good left coronary artery blood flow (Fig. 3I), with an aortic valve transvalvular PG of ~18 mmHg.
Interventional Management
Procedural Step
Digital subtraction angiography (DSA) showed that the leaflets had severe calcification with very poor mobility (Fig. 3A). According to the preoperative strategy suggested by the in-silicon simulation, a 20X40 mm balloon was used to pre-dilate the native valves with a rapid pacing rate of 150 beats per minute. A mild “waist sign” during aortic valvuloplasty was observed. It further confirmed that the size of the prosthesis should be "downsizing". A self-expanding Venus L26 valve was selected and released at the location of 5mm below the annulus. The valve was under-expansion and TEE found there was massive perivalvular leakage. This could be most likely due to the heavy calcific mass resulting in the malposition of the local prosthesis frame. The post-dilatation was performed with a 22mm balloon to improve the shape of the prosthesis, with continuous check of blood flow at the ostium of the left coronary artery under DSA. TEE was also conducted every 5 minutes several times to confirm whether the obstruction of the left coronary artery caused by the delayed expansion of the stent. Subsequent angiography and echocardiography revealed no significant paravalvular leakage, and the procedure was deemed successful and concluded.


Case Summary
The computer simulation of a virtual balloon pre-dilatation could be a useful method to predict the balloon sizing for TAVR valves and help to assessment for the risk of coronary obstruction. This could optimize the pre-procedural accurate evaluation of TAVR for high-risk patients.

