Lots of interesting abstracts and cases were submitted for TCTAP 2024. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-165
Guiding Intervention for Venous Graft in Coronary Bypass Using Resting Full-Cycle Ratio: Evaluation of Successful Effectiveness
By Wei-Ting Liu, Yen-Lien Chou
Presenter
Wei-Ting Liu
Authors
Wei-Ting Liu1, Yen-Lien Chou2
Affiliation
Division of Cardiology, Department of Internal Medicine, Tri-Service General Hospital, National Defense, Taiwan1, Tri-Service General Hospital, Taiwan2,
View Study Report
TCTAP C-165
Coronary - Imaging & Physiology - FFR
Guiding Intervention for Venous Graft in Coronary Bypass Using Resting Full-Cycle Ratio: Evaluation of Successful Effectiveness
Wei-Ting Liu1, Yen-Lien Chou2
Division of Cardiology, Department of Internal Medicine, Tri-Service General Hospital, National Defense, Taiwan1, Tri-Service General Hospital, Taiwan2,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
A 77 male
History of CAD, TVD s/p CABG x4 (LIMA to LAD, VG to DB1, OM1, PDA) 13 years ago, HTN, Type 2 DM, COPD, s/p tracheostomy, under respiratory training.
Clinical presentation: Intermittent chest pain for weeks.
Vital sign: BP 112/51 mmHg, HR 55 b.p.m., SpO2 100% under PS mode Pressure 10 cmH2O, PEEP 6 cmH2O, FiO2 30%.
PE: Regular heart beats, no murmur.
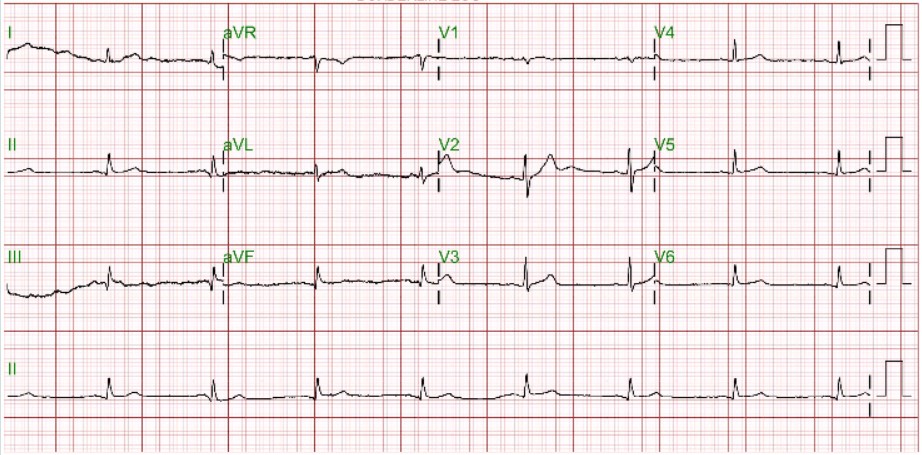
ECG: Sinus rhythm, Q wave in Lead II, III.
Relevant Test Results Prior to Catheterization
Echocardiogram: Normal LV systolic function.
Tl-201: moderate to severe CAD in LCX and RCA, mild in LAD area.
Relevant Catheterization Findings
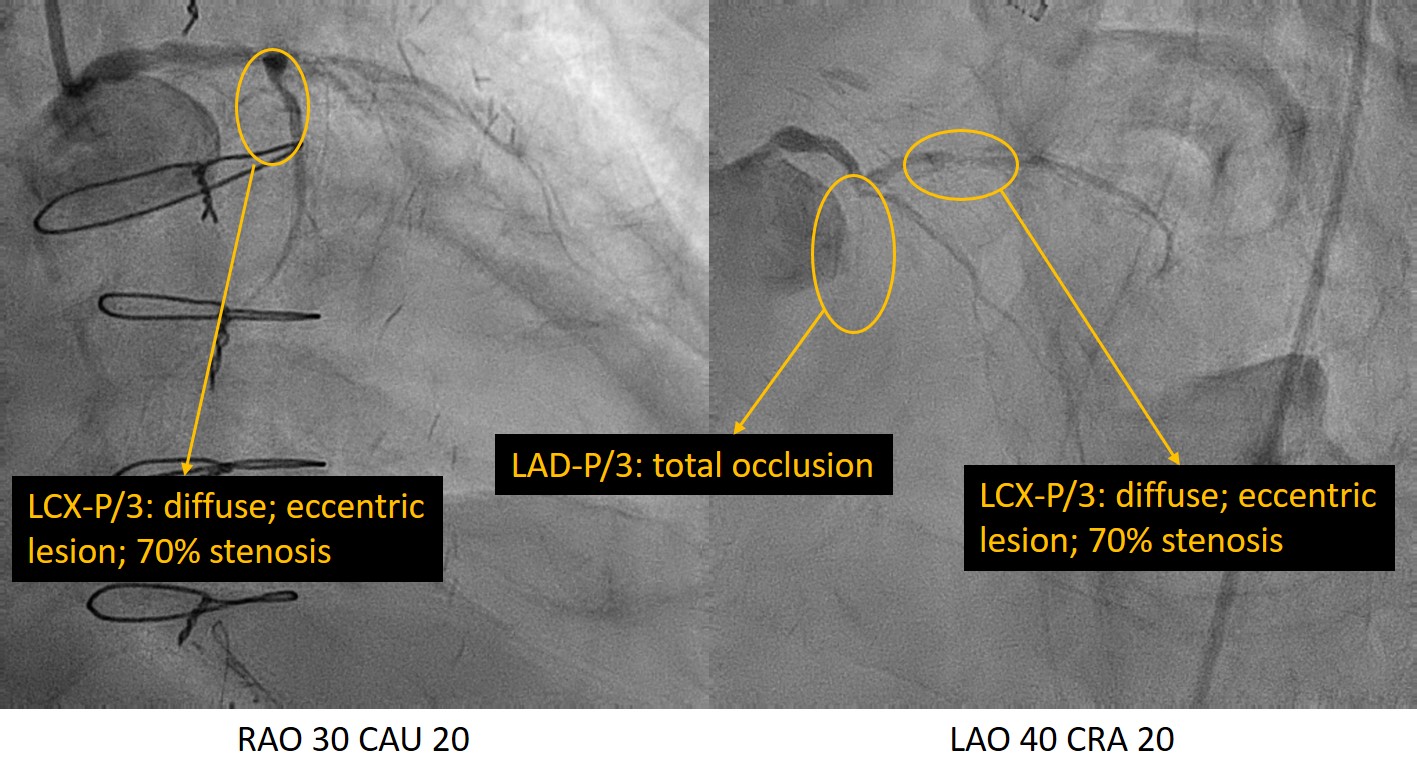
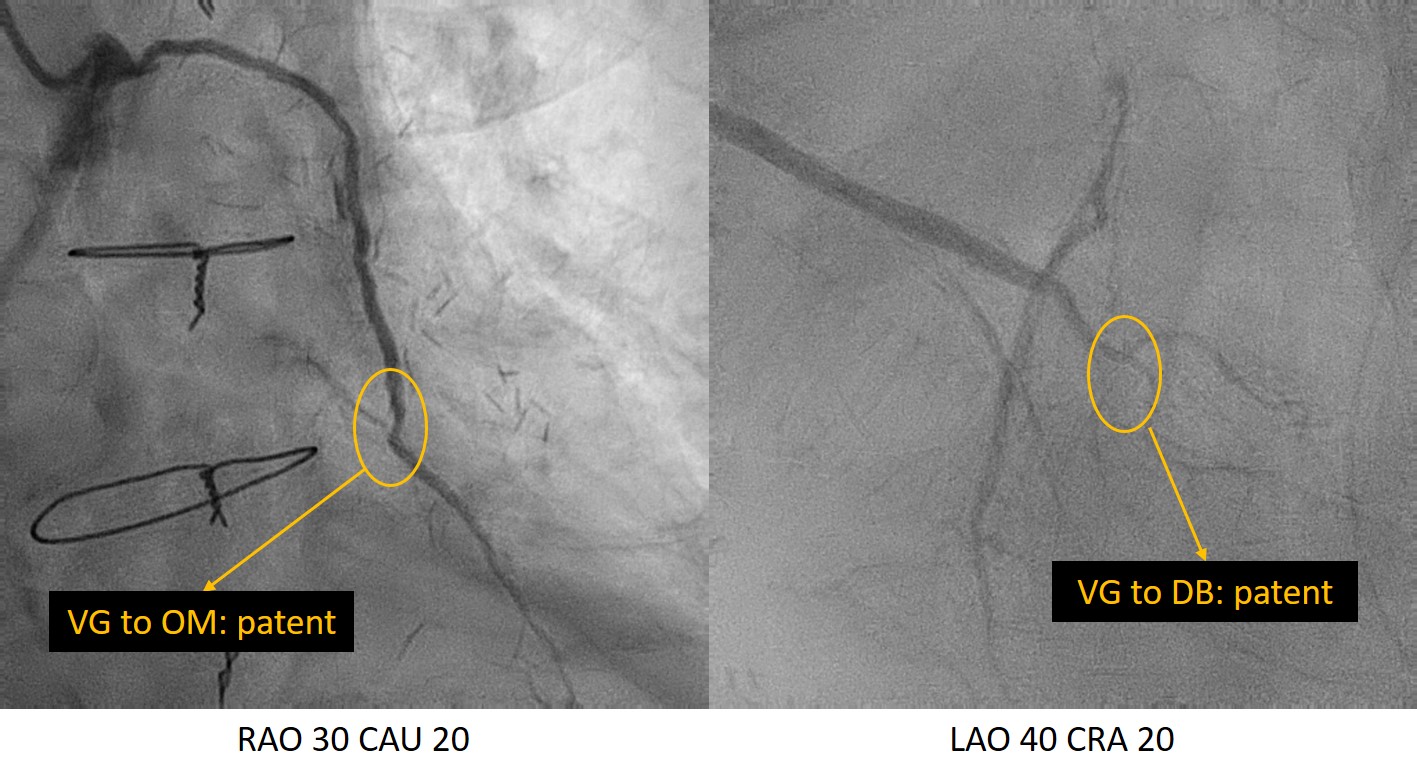
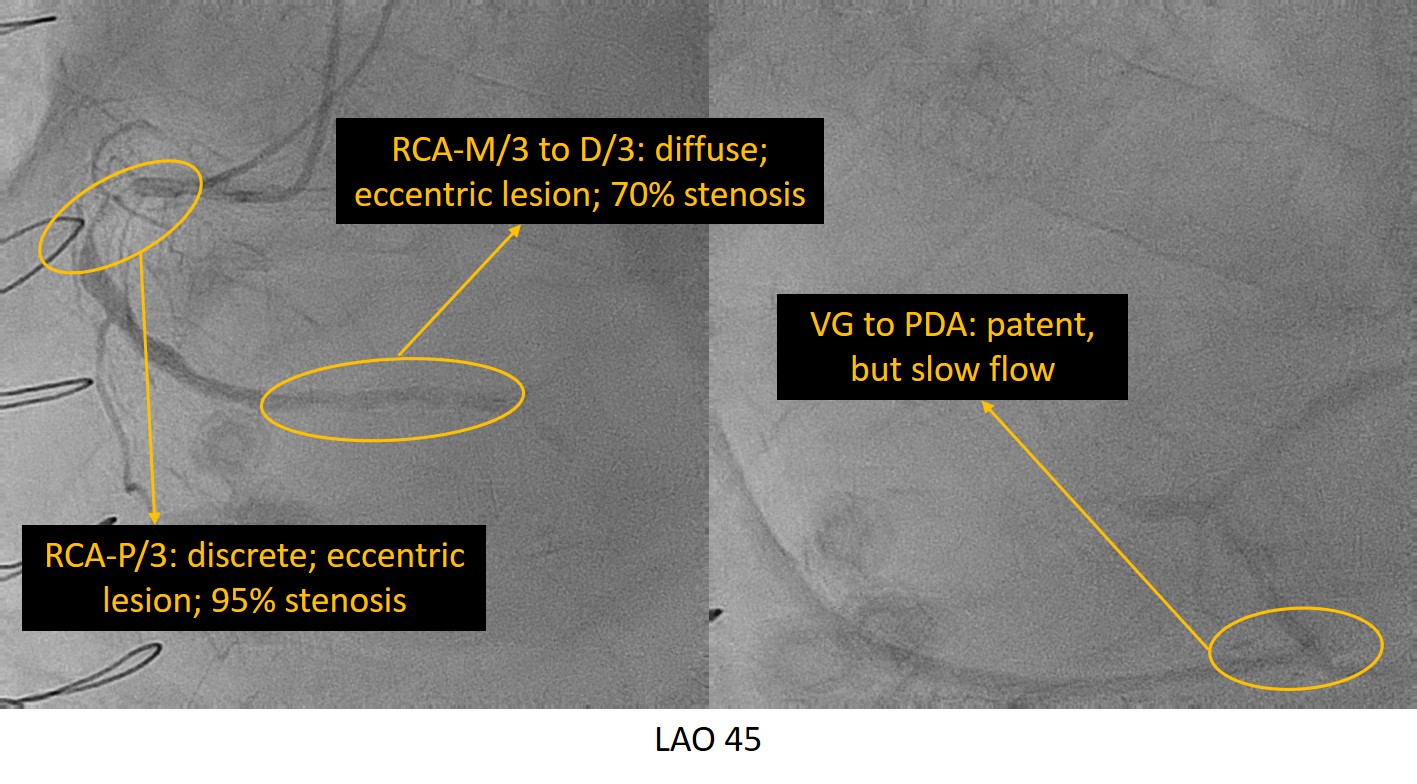
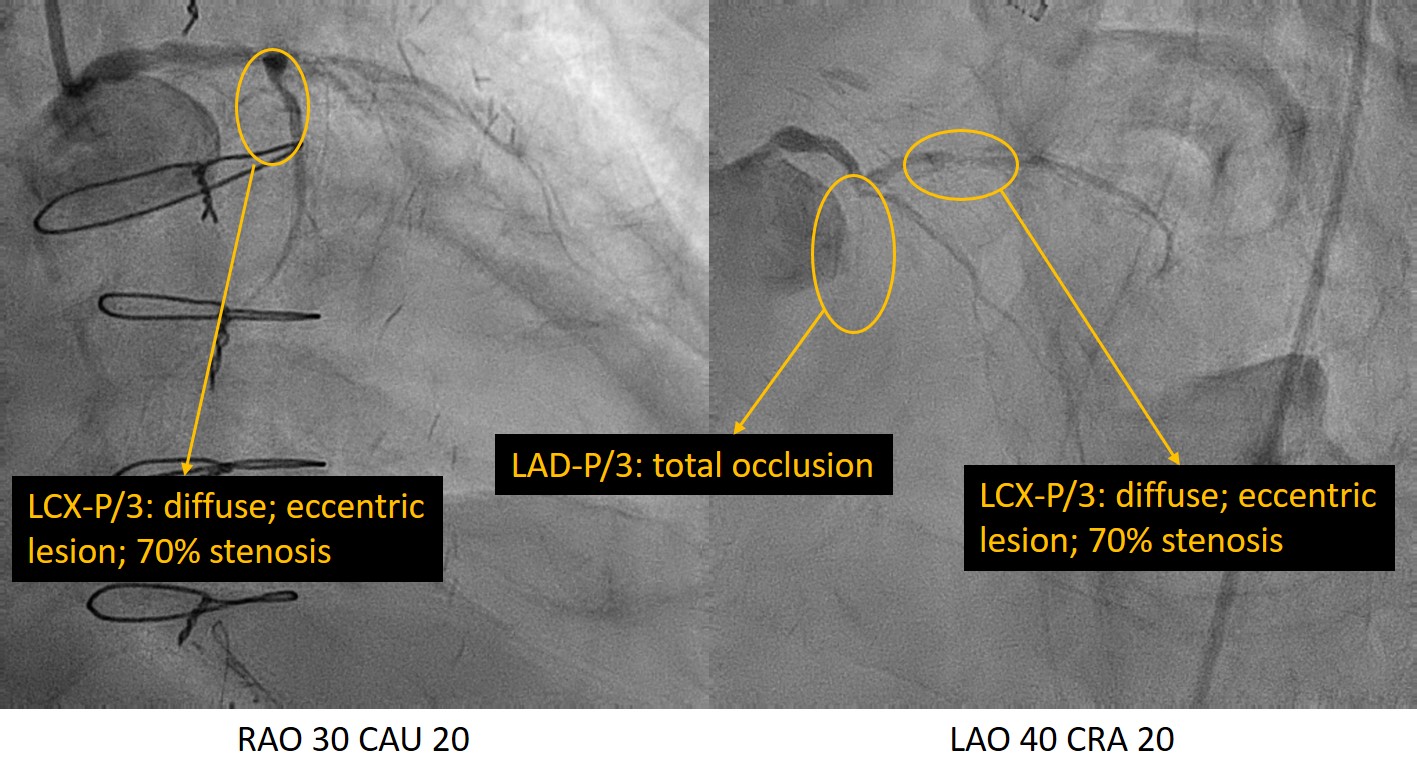
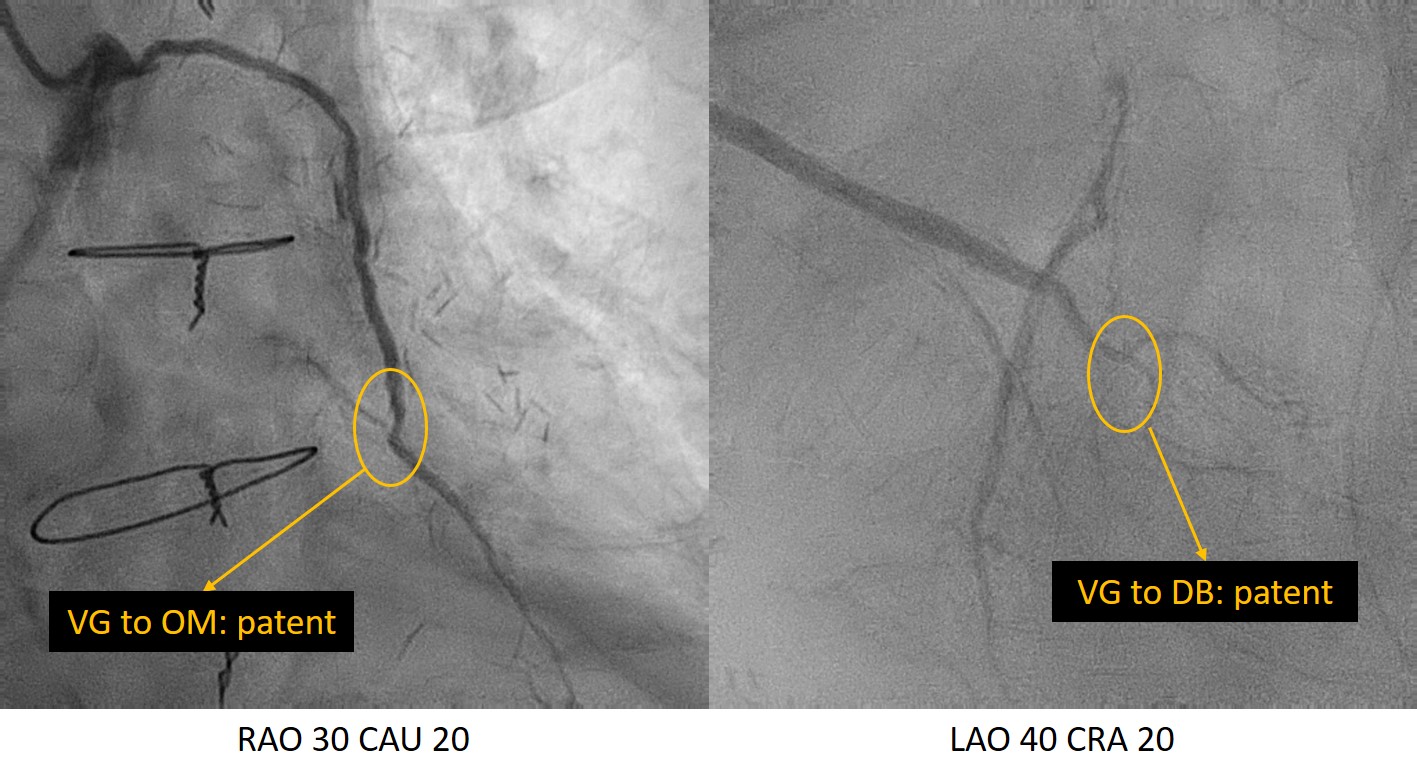
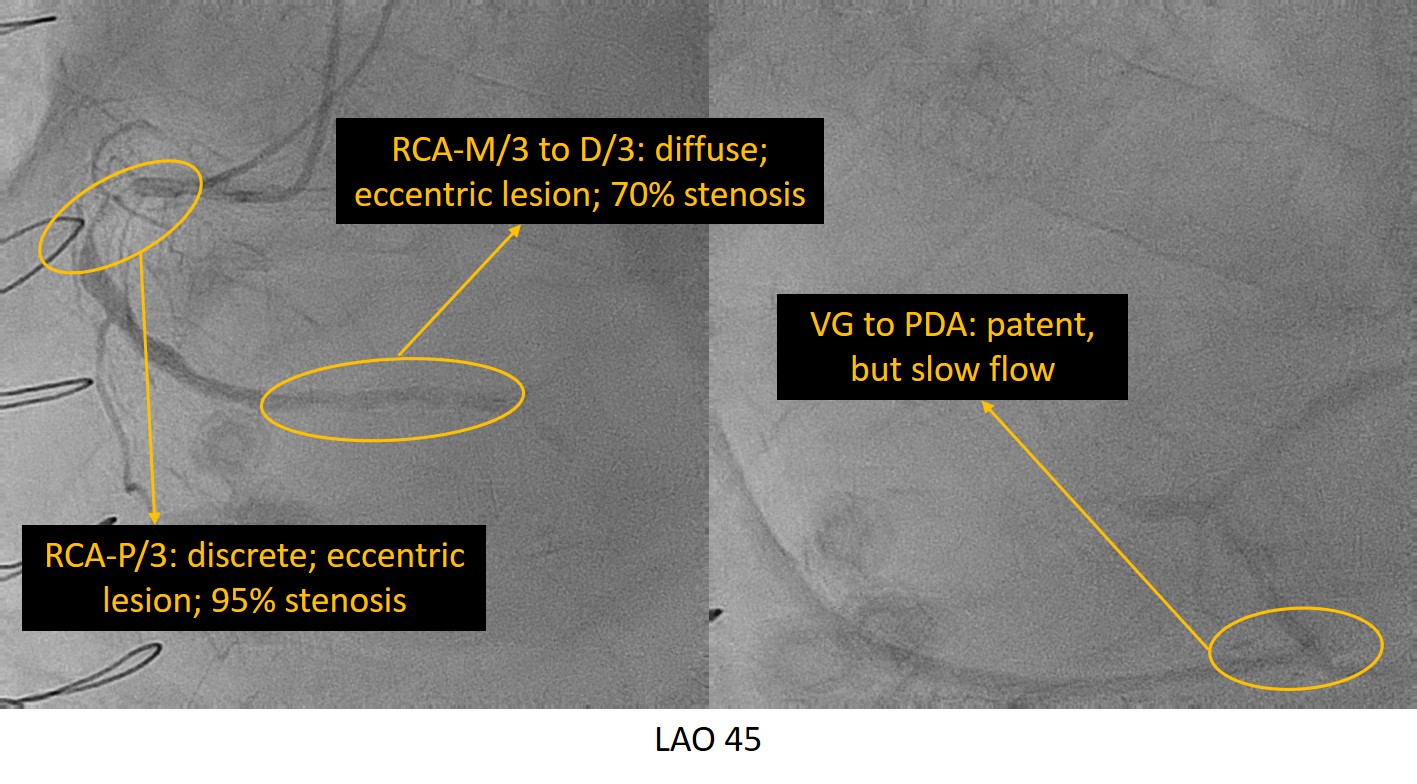
1) LMCA: atherosclerosis M/3: discrete; eccentric lesion; 40% stenosis; 2) LAD: atherosclerosis P/3: total occlusion 3) LCX: atherosclerosis P/3: diffuse; eccentric lesion; 70% stenosis; 4) RCA: atherosclerosis P/3: discrete; eccentric lesion; 95% stenosis; TIMI 2 flow M/3 to D/3: diffuse; eccentric lesion; 70% stenosis; TIMI 2 flow 5) VG to OM: patent 6) VG to DB: patent 7) VG to PDA: patent, but slow flow 8) LIMA to LAD: patent
Interventional Management
Procedural Step
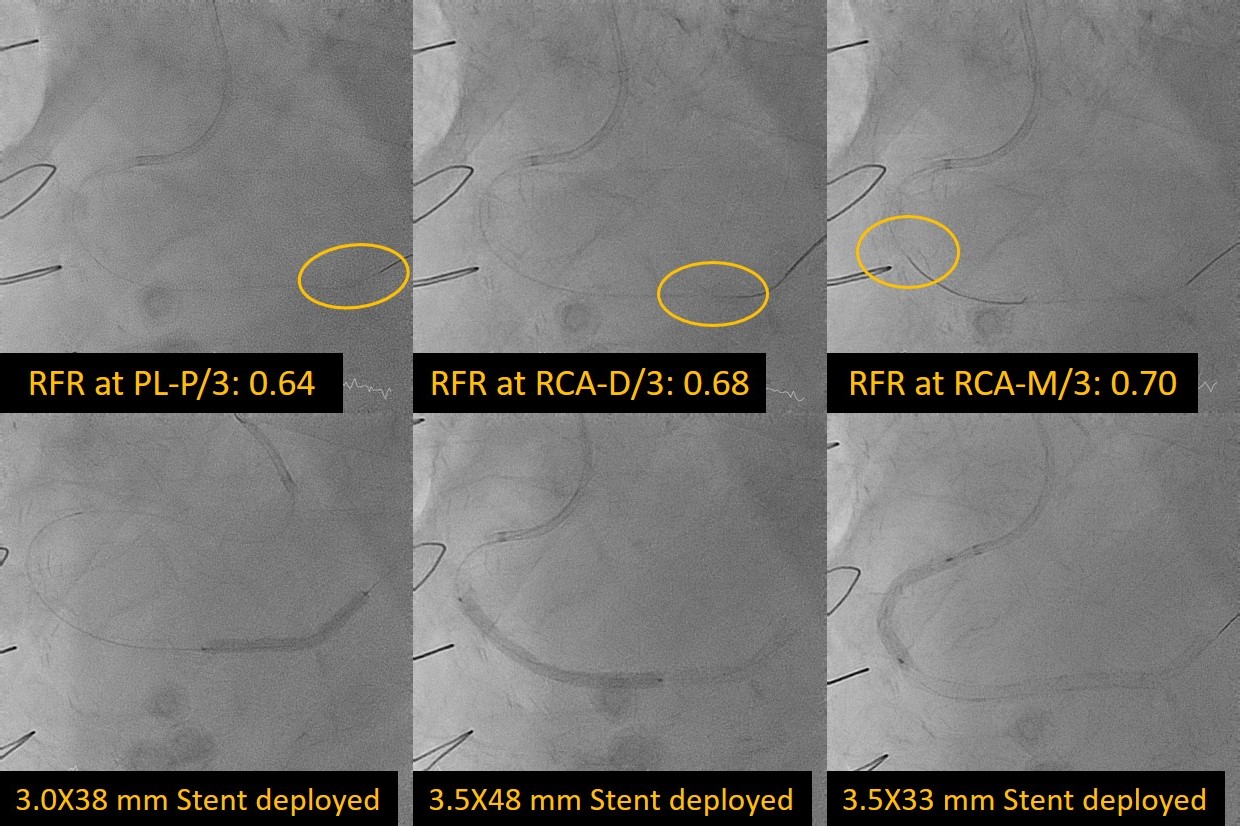
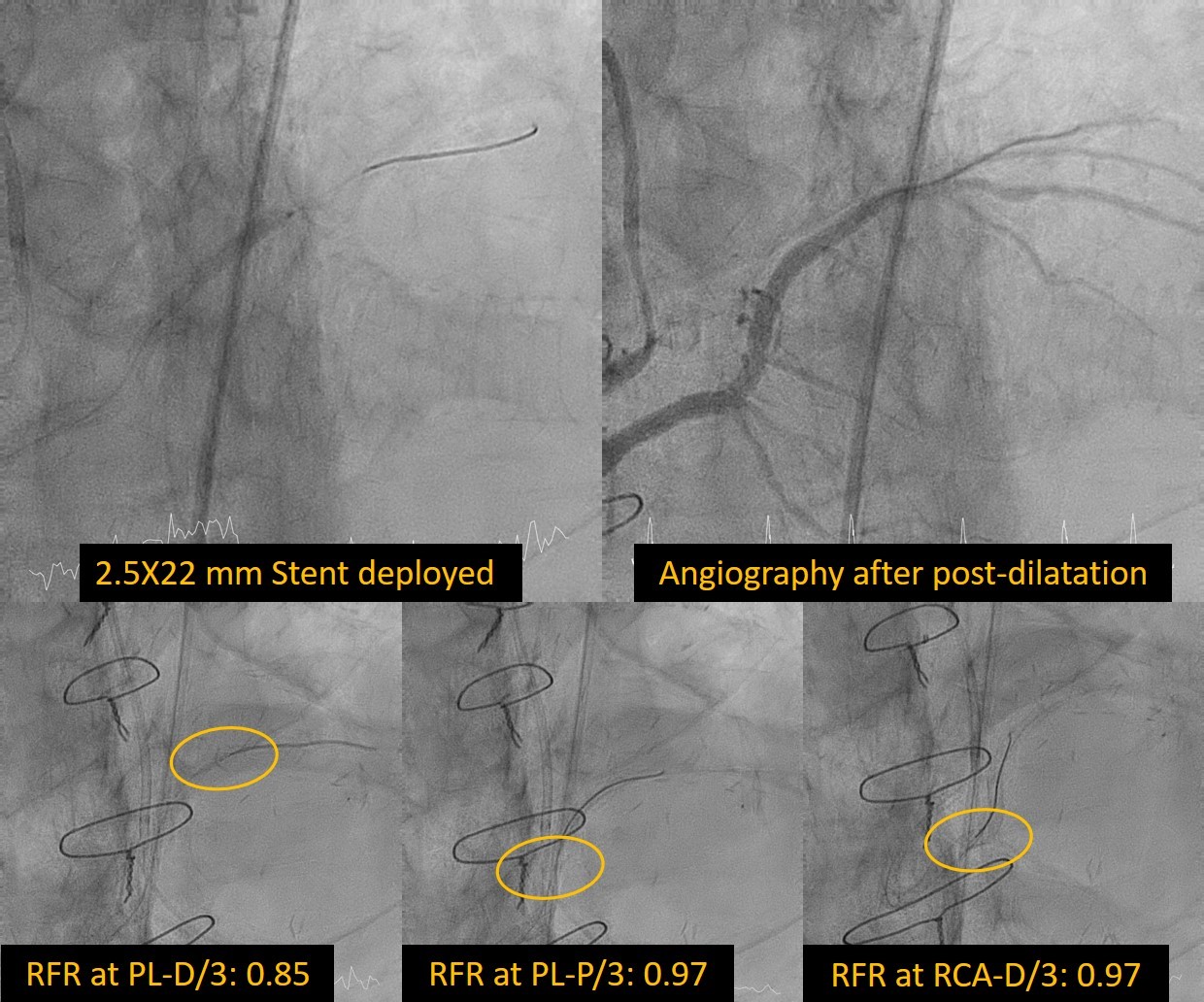
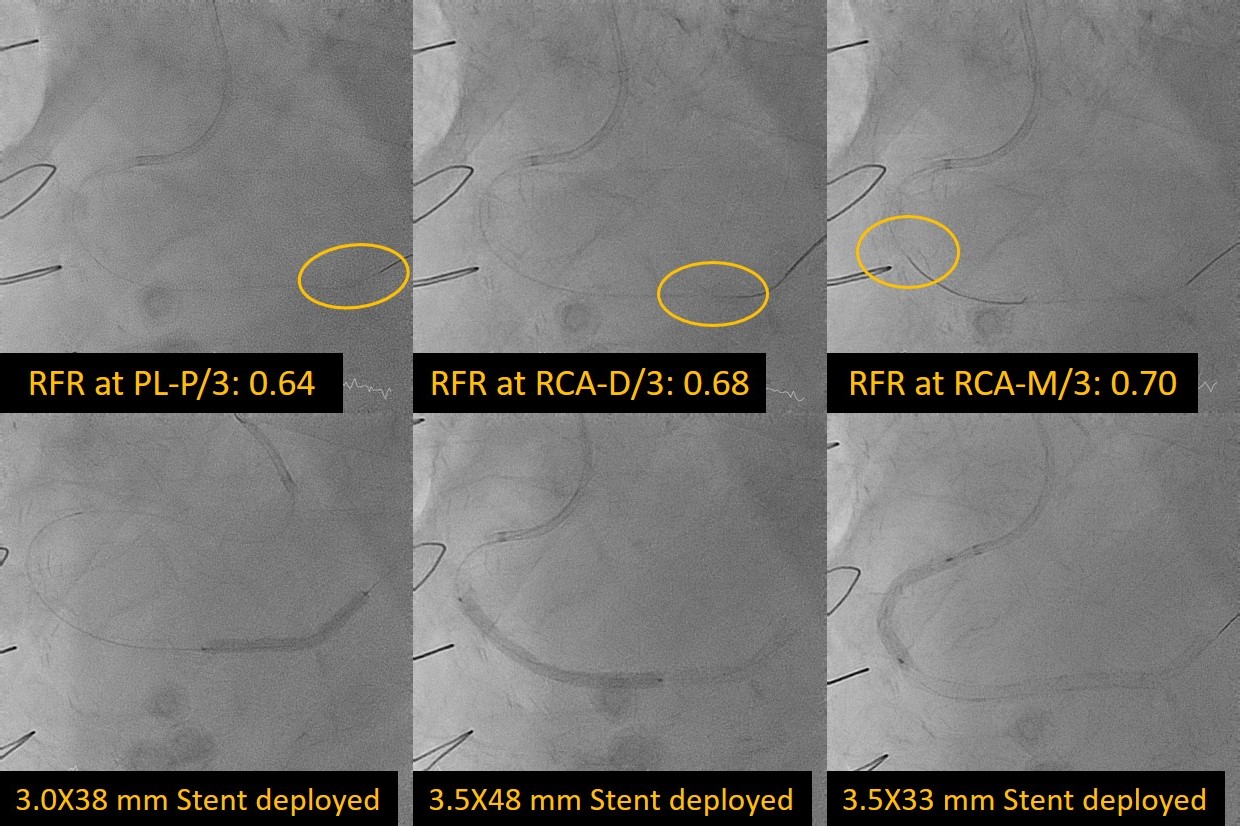
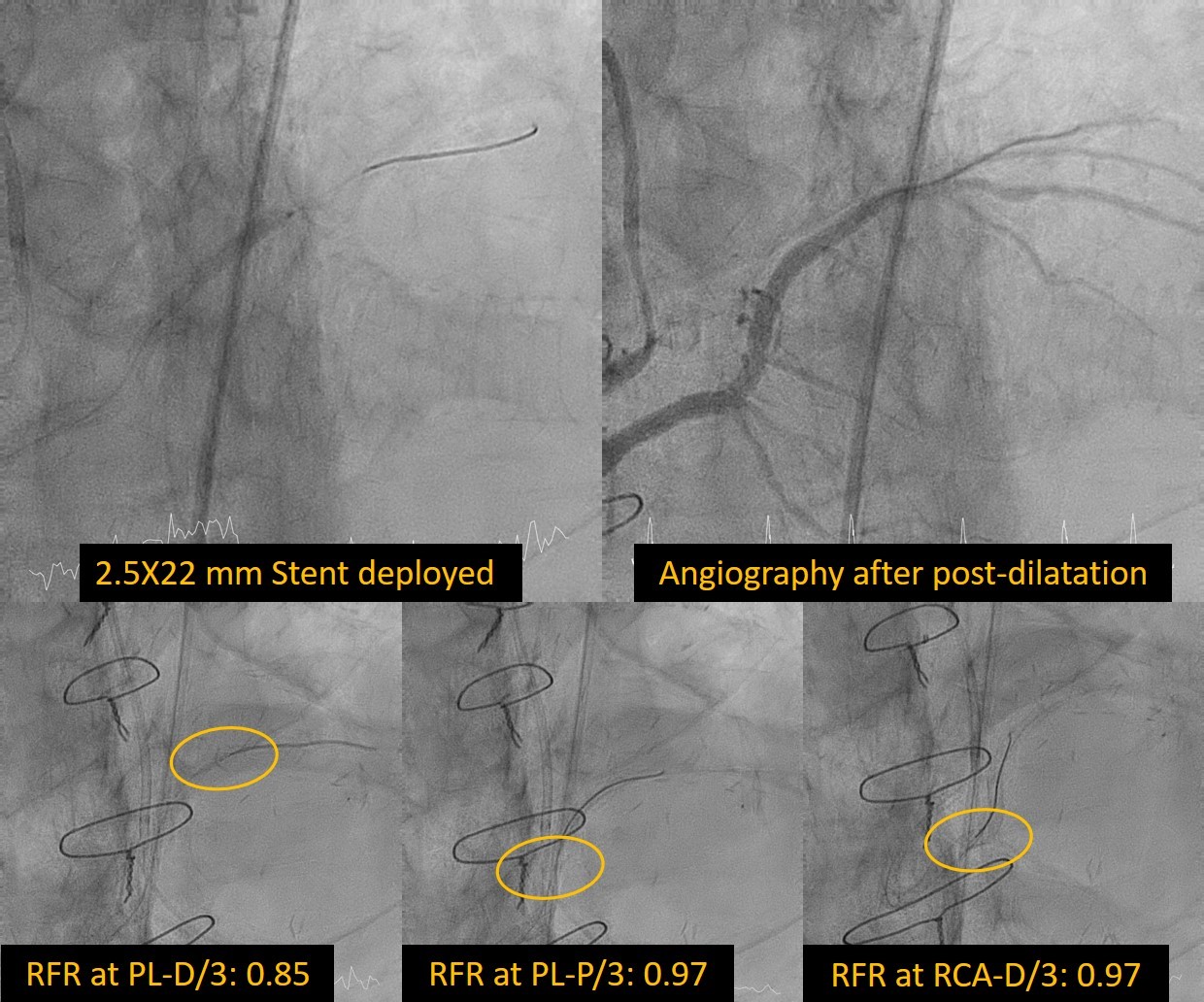
1. The RCA ostium was engaged by SAL 1.0 guiding catheter.2. The Sion black wire was used to cross the RCA lesion and landed at distal PL.3. The Proximal RCA lesion was dilated by a 1.5X20 mm balloon. 4. Pressure wire was used to evaluate the effect of PDA graft on RCA and PL. The RFR showed 0.64 at PL, 0.68 at D/3 RCA and 0.70 at M/3 RCA.5. The RCA lesion was dilated by a 3.0X20 mm NC balloon and the proximal PL lesion was dilated by a 2.0X20 mm balloon.[IVUS] The MLA of the lesion is 3.78 mm2, circumferential calcification was noted. The plague burden was 81%.6. The RCA lesion was dilated by a 2.5X10 mm Cutting balloon to break the circumferential calcification.7. The D/3 RCA to PL lesion was stented with a 3.0X38 mm Stent and post-dilated with a 3.5X15 mm NC balloon with stenosis from 50% to 0%.8. The M/3 to D/3 RCA lesion was stented with a 3.5X48 mm Stent and post-dilated with a 3.5X15 mm NC balloon.9. The P/3 RCA lesion was stented with a 3.5X33 mm Stent and post-dilated with a 4.0X12 mm NC balloon.10. The pressure wire was used to evaluate the stent effect. However, the RFR showed 0.75 at D/3 of PL, 0.92 at P/3 of PL and 0.93 at RCA.11. The distal PL was dilated by a 2.0X20 mm Trek balloon and then stented with a 2.5X22mm Stent. Post-dilatation with a 2.5X15 mm NC balloon.12. The RFR showed 0.85 at D/3 PL and 0.97 at RCA.[IVUS] MSA is 8.81 mm2, well position and expansion were noted.13. Final angiography showed <10% residual stenosis with TIMI 3 flow.


Case Summary
We present a case following CABG with recurrent angina pectoris. The patient exhibited a patent vein graft but with slow blood flow in both the native RCA and the vein graft to PDA. Physiological evaluation provided valuable guidance in determining the need for intervention and identifying the lesions requiring treatment. While the utilization of resting full-cycle ratio (RFR) in bypass vein grafts lacks extensive study, this case highlighted a functionally suboptimal distal myocardial segment using RFR, prompting intervention for the physiologically significant lesions. Following stenting, the patient experienced an improvement in angina symptoms and was discharged without complications.

