Lots of interesting abstracts and cases were submitted for TCTAP 2024. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-009
Atrial Septal Occlusion Device in an Ischemic Ventricular Septal Rupture
By Jerome Joseph Sioson, Jhoanna Marcelo, Ronaldo Estacio
Presenter
Jerome Joseph Sioson
Authors
Jerome Joseph Sioson1, Jhoanna Marcelo2, Ronaldo Estacio2
Affiliation
Brokenshire Medical Center, Philippines1, Philippine Heart Center, Philippines2,
View Study Report
TCTAP C-009
Coronary - ACS/AMI
Atrial Septal Occlusion Device in an Ischemic Ventricular Septal Rupture
Jerome Joseph Sioson1, Jhoanna Marcelo2, Ronaldo Estacio2
Brokenshire Medical Center, Philippines1, Philippine Heart Center, Philippines2,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
RC is a 57 year old Filipino male admitted to the ICU and managed as one vessel coronary artery disease and ventricular septal defect. He was previously diagnosed as anterior wall STEMI but medically managed. There was a grade 4/6 holosystolic murmur on the left sternal border. He had hypotension with BP of 80/60 mmHg with worsening of dyspnea during ICU stay and underwent emergency IABP insertion with percutaneous closure of the VSR using an ASD occluder device with no complications.
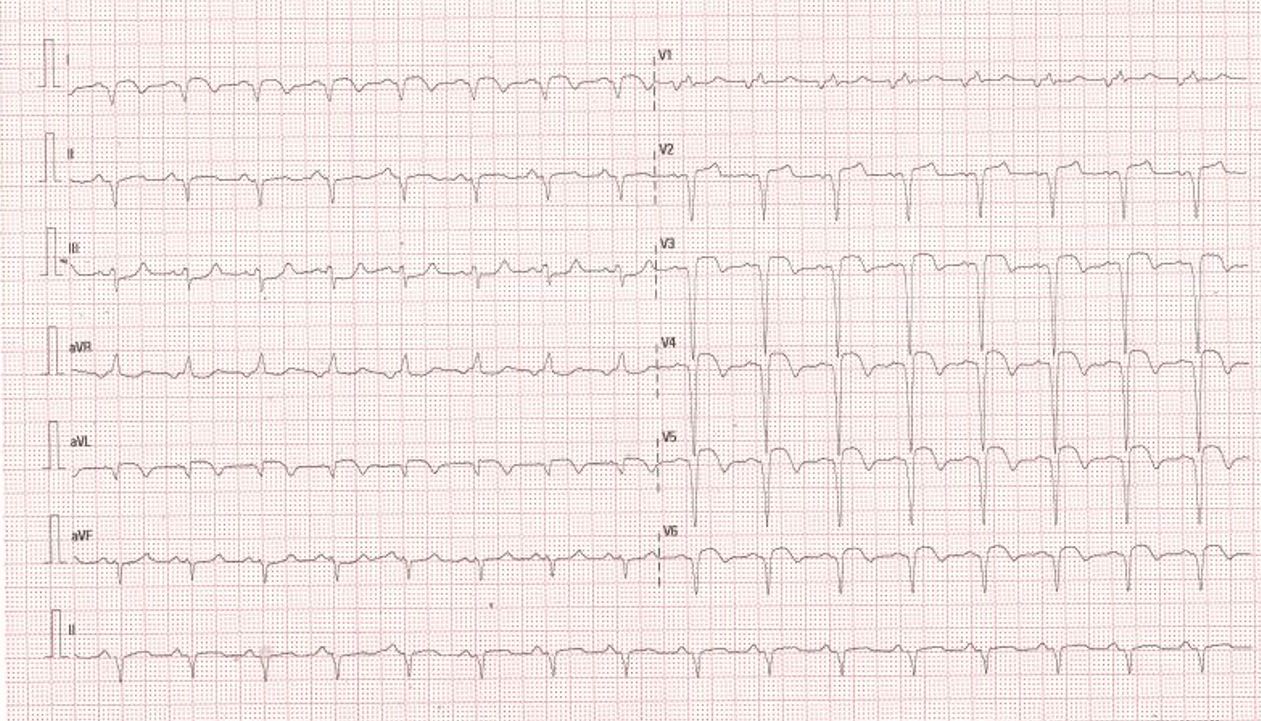
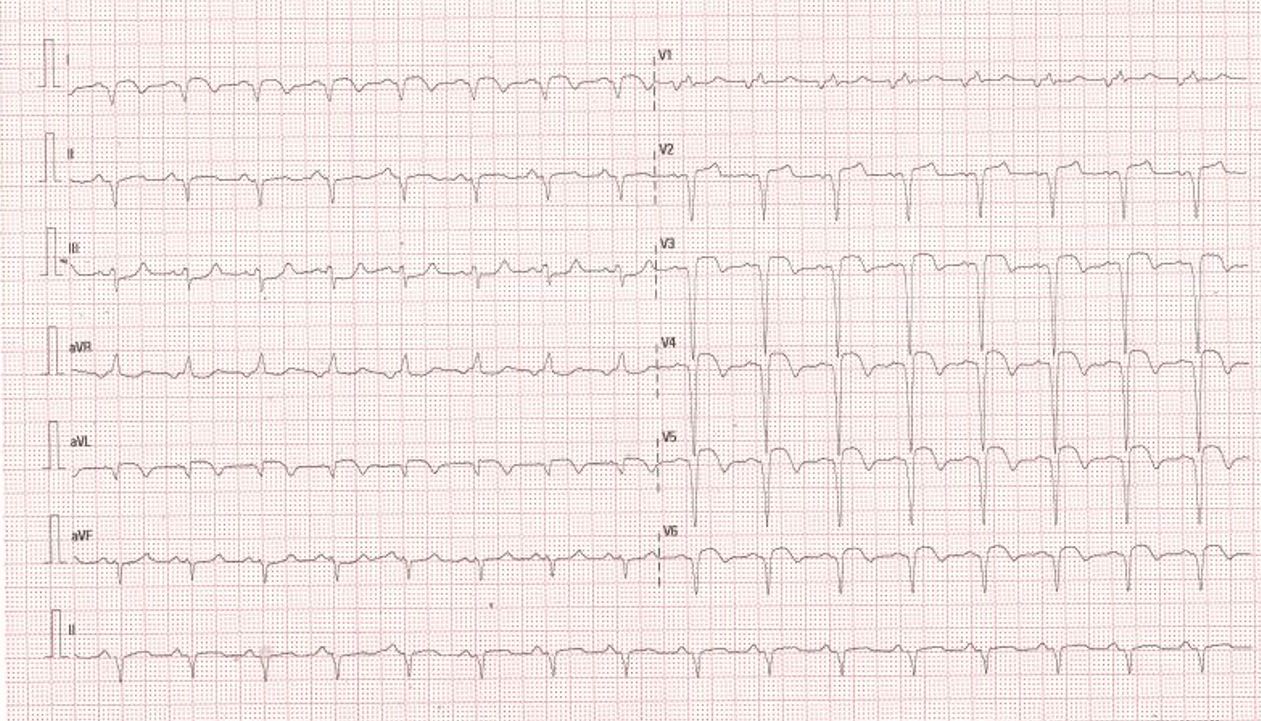
Relevant Test Results Prior to Catheterization
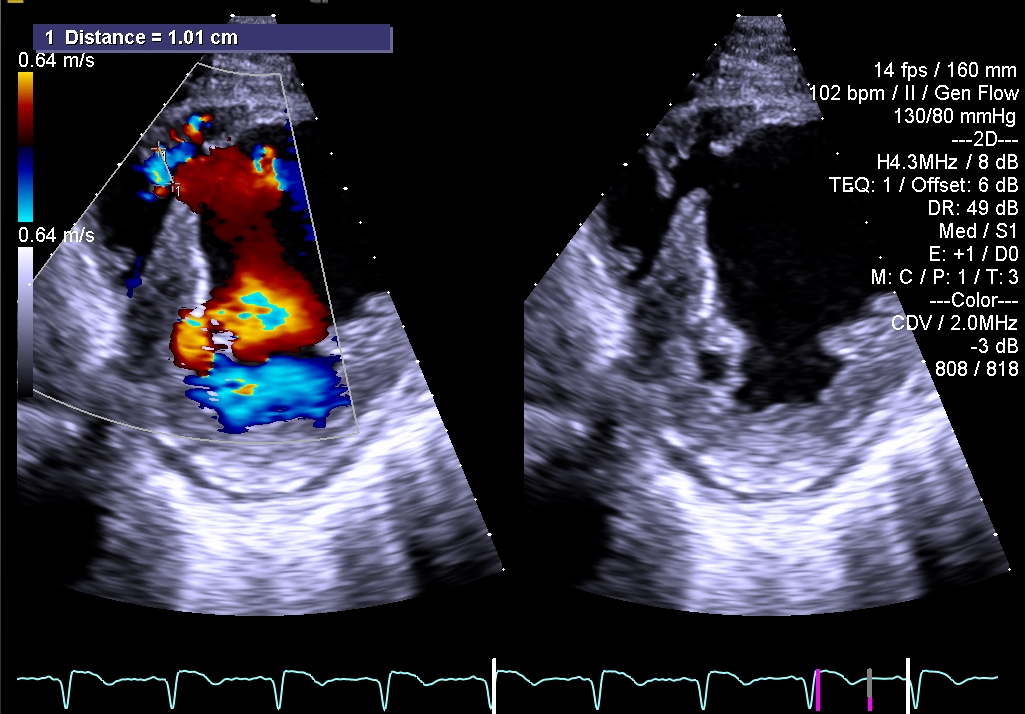
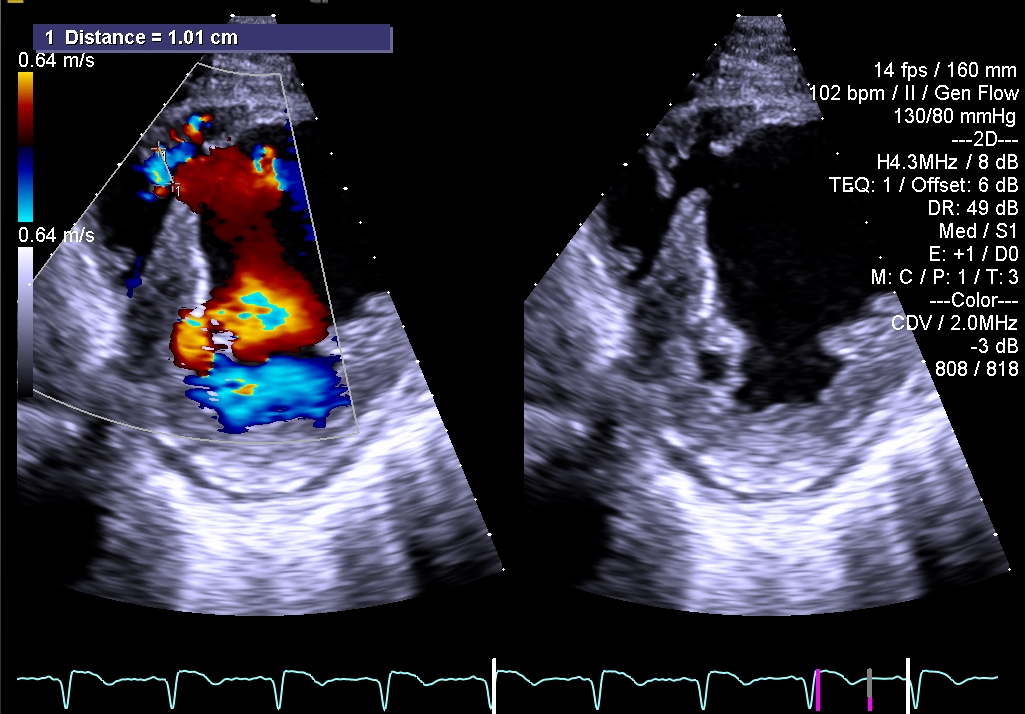
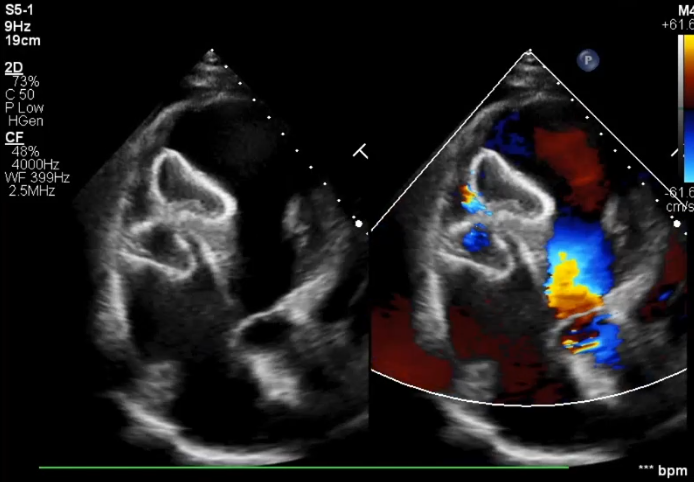
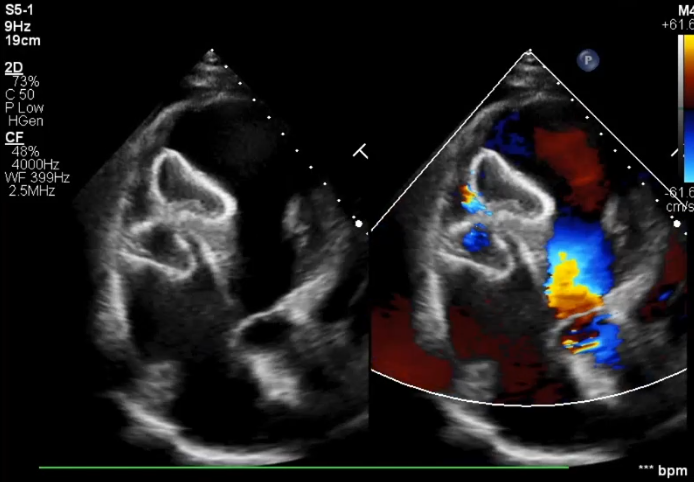
Transthoracic echocardiogram showed an echo dropout seen at the apical portion of the interventricular septum measuring 1.44cm. There was hypokinesia of the basal and mid anterior septum, apical lateral segment and mid anterior segment with akinesia of the apical septal segment, apical anterior and apex with ejection fraction of 35%. Myocardial perfusion scan showed mainly scarred anterior, septal and lateral myocardium.




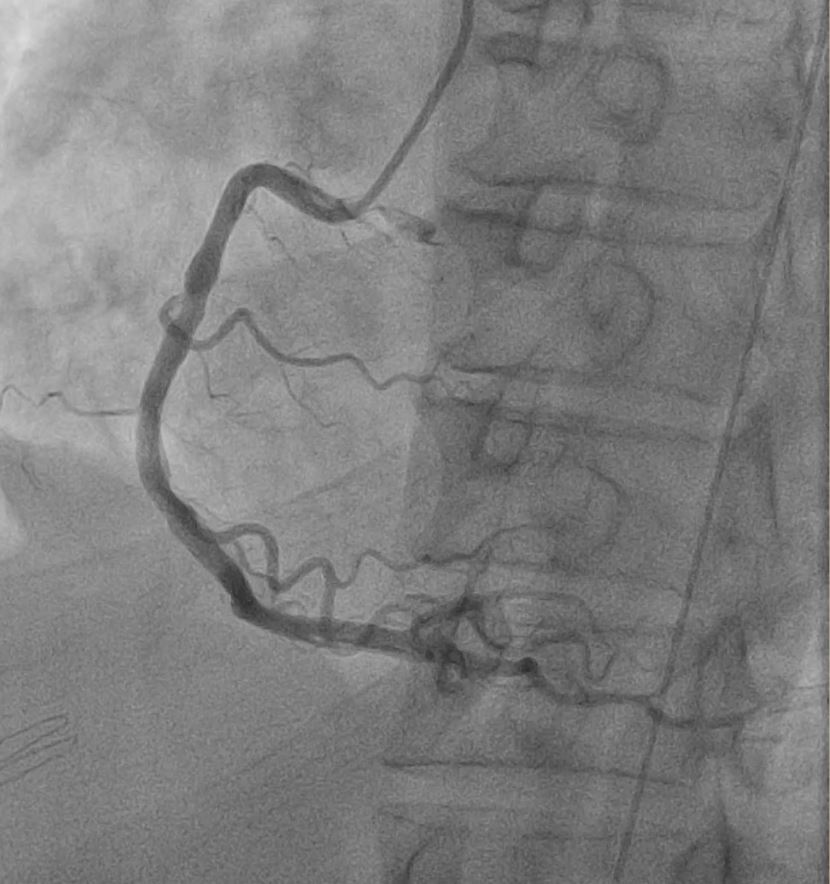
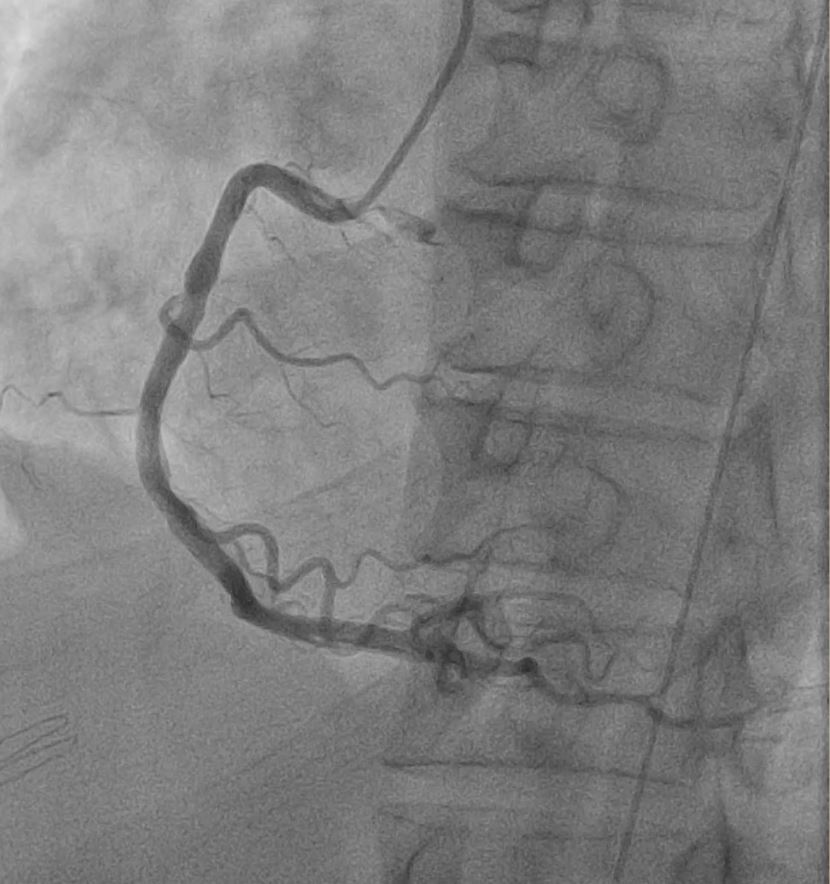
Relevant Catheterization Findings
The coronary angiogram showed a left anterior descending artery with a 95% mid segment stenosis. Intra-aortic balloon pump was inserted. Left Ventriculogram showed contrast extravasation into the right ventricle from the left ventricle. Pressure recordings showed an elevated pulmonary artery pressure of 73/31 mmHg, elevated RV systolic pressure at 80 mm Hg. Oximetry saturation showed a step up in the right ventricle with 91% saturation and mixed venous oxygen saturation of 61%




Interventional Management
Procedural Step
A right femoral arterial access and a right internal jugular venous access was obtained. Left ventriculography was done on LAO 30 and Cranial 30 projection to outline the defect. A transesophageal echocardiogram was also used to accurately assess the ventricular septal defect. A modified 6F pigtail catheter with a hydrophilic wire was used to cross the defect while using a snare system to externalize the wire from the right internal jugular vein to obtain an arteriovenous circuit. The delivery system was then advanced from the right internal jugular vein and across the defect until the tip was at the left ventricle. An atrial septal defect occluder 36 mm was used and advanced to the defect. The distal disk was opened and gently pulled back while the sheath was slowly retracted with eventual complete deployment of the device. A repeat left ventriculogram showed no contrast extravasation across the defect with confirmation on transesophageal echocardiogram. The device was then released by turning counterclockwise.




Case Summary
Surgical management is the mainstay for treatment for ventricular septal rupture but appropriate timing has been difficult. A percutaneous approach has been developed to provide a definitive treatment or bridge to surgery. This case highlights that a primary transcatheter closure using an ASD occlusion device for ischemic ventricular septal defect can be a safe and feasible definitive option. Timely closure of the left to right shunt has improved systemic circulation with decrease in heart failure symptoms leading to improved clinical status and eventual discharge.

