Lots of interesting abstracts and cases were submitted for TCTAP 2024. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-201
Embolic Odyssey: Overcoming Challenges in the Battle Against Massive Pulmonary Embolism
By Nay Thu Win, George Besis, Tushar Kotecha
Presenter
Nay Thu Win
Authors
Nay Thu Win1, George Besis2, Tushar Kotecha1
Affiliation
Royal Free London, United Kingdom1, North Wales Cardiac Center, United Kingdom2,
View Study Report
TCTAP C-201
Endovascular - Thrombus Removal Devices and Techniques
Embolic Odyssey: Overcoming Challenges in the Battle Against Massive Pulmonary Embolism
Nay Thu Win1, George Besis2, Tushar Kotecha1
Royal Free London, United Kingdom1, North Wales Cardiac Center, United Kingdom2,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
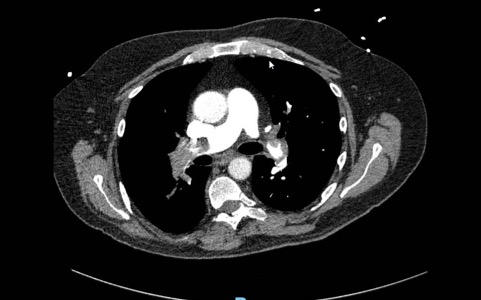
A 69-year-old male with a history of HIV, hepatitis B, and a previous pulmonary embolism (PE) in 2018 presented to a district general hospital with acute shortness of breath, pleuritic chest pain, and pre-syncope. ECG showed sinus tachycardia and right ventricular strain pattern. Blood pressure was 95/50, HR 112 bpm, Respiratory rate 30 per min. CTPA revealed a heavy burden of bilateral massive PE along with evidence of early right heart strain. ABG showed lactic acidosis.
Relevant Test Results Prior to Catheterization
He underwent EKOS procedure and started a treatment dose of dalteparin. However, he experienced deterioration with increasing oxygen requirements and on he experienced deterioration with increasing oxygen requirements and ongoing tachycardia following the procedure. A repeated CTPA two days later showed an increasing burden of PE bilaterally, including a saddle PE and evidence of right heart strain. Then, proceed for percutaneous thrombectomy using the FlowTriever system after counselling.


Relevant Catheterization Findings
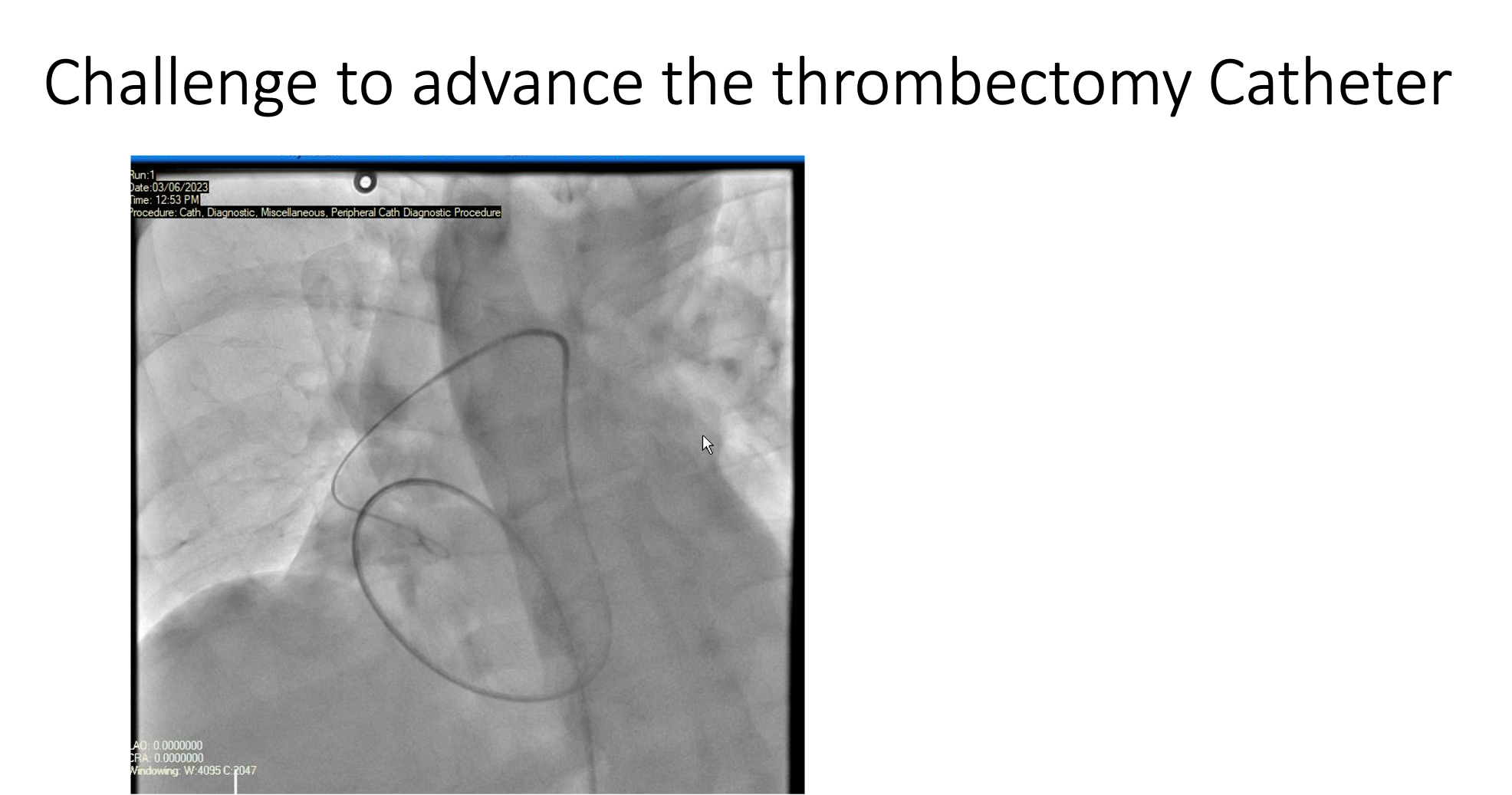
Femoral ultrasound revealed the presence of a clot in the right femoral vein. 9F sheath was inserted via left femoral vein. FlowTriever catheter was unable to pass into the right pulmonary artery (RPA) was unsuccessful due to tortuousity and poor support. 26F Gore Dryseal sheath was inserted, providing improved access and a pigtail catheter was advanced into the PA.At this stage, PAP was 67/25 mmHg with mPAP at 39 mmHg, while PA sat was 29%.
Interventional Management
Procedural Step
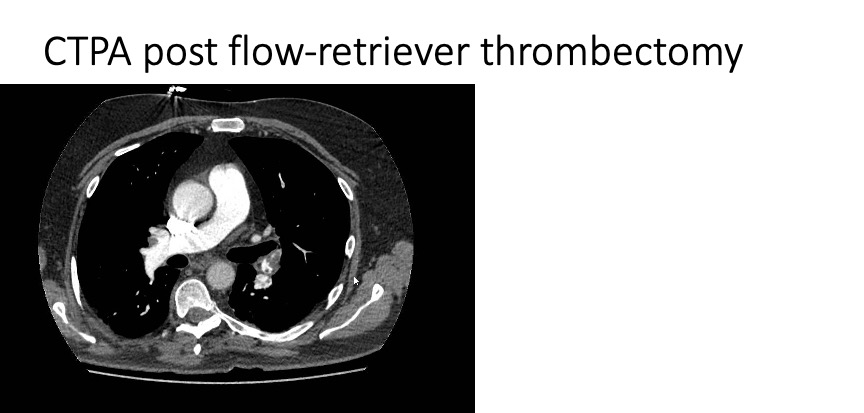
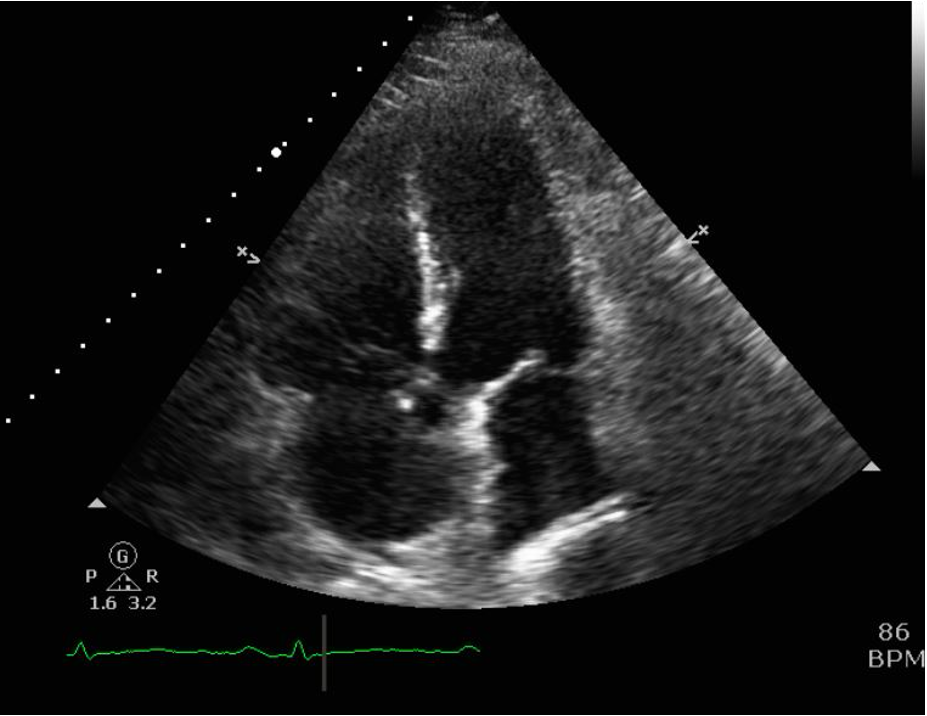
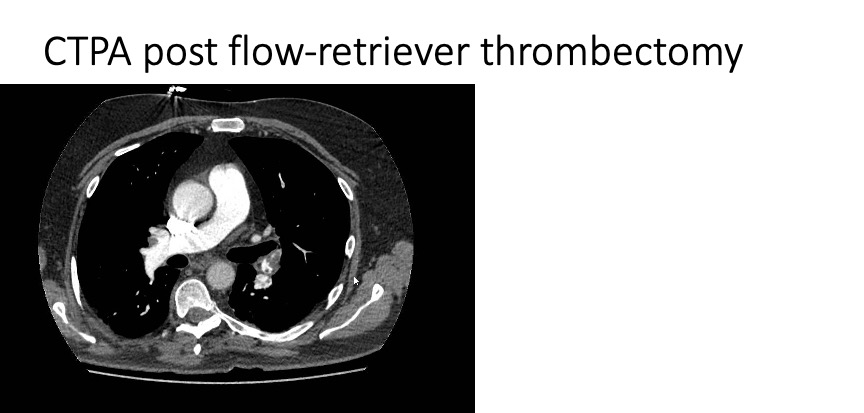
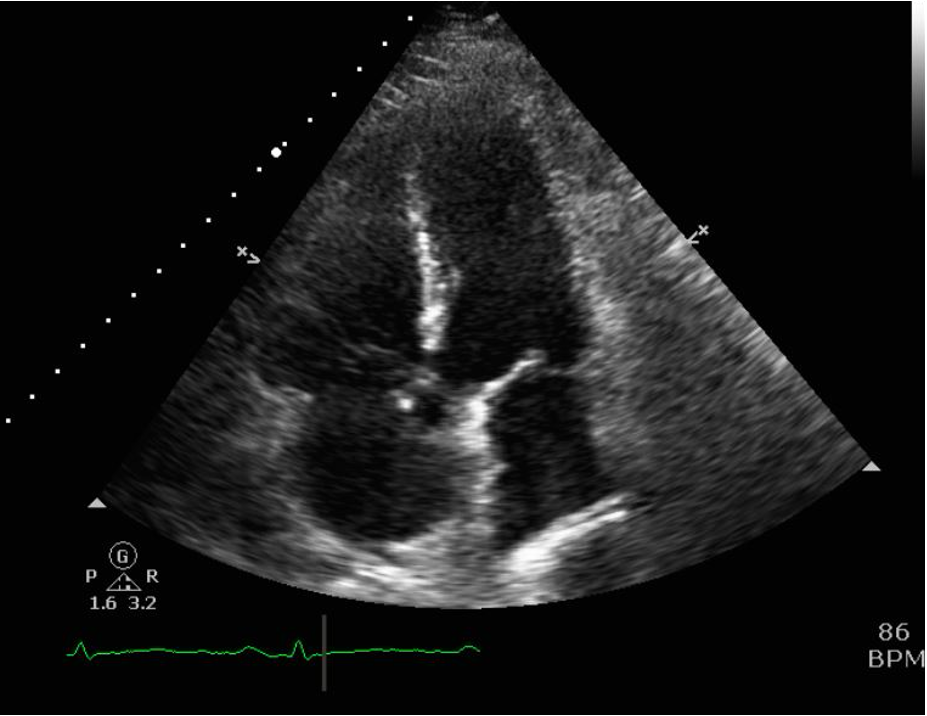
Pulmonary angiography revealed the presence of a large occlusive clot in the right main PA. Additionally, the left mid pulmonary artery appeared occluded, although adequate perfusion was observed in the lower and upper branches. A FlowTriever catheter (24F) was then directed into the RPA, followed by four aspirations that successfully removed a large volume of clot. Some residual clot remained in the right upper branch, but perfusion was satisfactory. The PA pressure decreased to 53/18 mmHg with mPAP of 30 mmHg, while the PA sat improved to 37%. The FlowTriever catheter was directed into the left PA, resulting in the successful aspiration of a single large clot. Pulmonary angiography demonstrated residual clot in the middle lobe artery; however, overall perfusion in this region improved. The final hemodynamic assessment after the procedure revealed PAP 46/20 mmHg with an mPAP of 28 mmHg, along with a PA sat of 45%. Closure of the LFV access site was achieved using a purse-string suture. Echocardiogram after 48 hours showed improvement of RV strain and pressure with Good LV and RV function. A repeat CTPA after 48 hours demonstrated significantly reduced clot burden with reveals a decreased right heart strain as evidenced by the RV:LV ratio measuring 1.5, demonstrating improvement when compared to the previous ratio of 2.1. Patient was discharged well after 3 days with longterm oral anticoagulation.


Case Summary
Despite the initial attempt with EKOS treatment and the initiation of anticoagulation, the patient experienced clinical deterioration with increasing oxygen requirements and ongoing tachycardia. This suggests that EKOS treatment alone was insufficient to adequately address the severity of the PE burden in some patients. Subsequent successful treatment with mechanical thrombectomy using FlowTriever thrombectomy proved to be beneficial in this patient. The consideration of alternative methods, such as percutaneous thrombectomies, becomes imperative for patients who exhibit inadequate response to EKOS and systemic thrombolysis.

