Lots of interesting abstracts and cases were submitted for TCTAP 2024. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-098
A Gush of Anxiety: Coronary perforation or Coronary-Cameral Fistula Following Revascularization of Occluded Left Anterior Descending Artery
By Khai Chih Teh, Aslannif Roslan
Presenter
Khai Chih Teh
Authors
Khai Chih Teh1, Aslannif Roslan1
Affiliation
National Heart Institute, Malaysia1,
View Study Report
TCTAP C-098
Coronary - Complex PCI - Long Lesion
A Gush of Anxiety: Coronary perforation or Coronary-Cameral Fistula Following Revascularization of Occluded Left Anterior Descending Artery
Khai Chih Teh1, Aslannif Roslan1
National Heart Institute, Malaysia1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
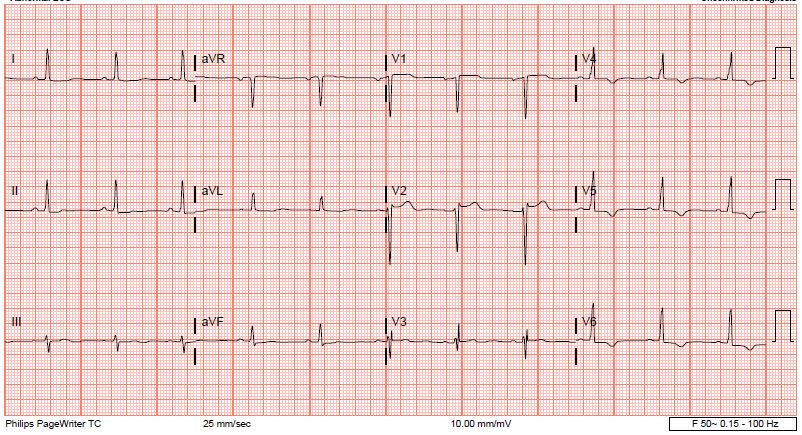
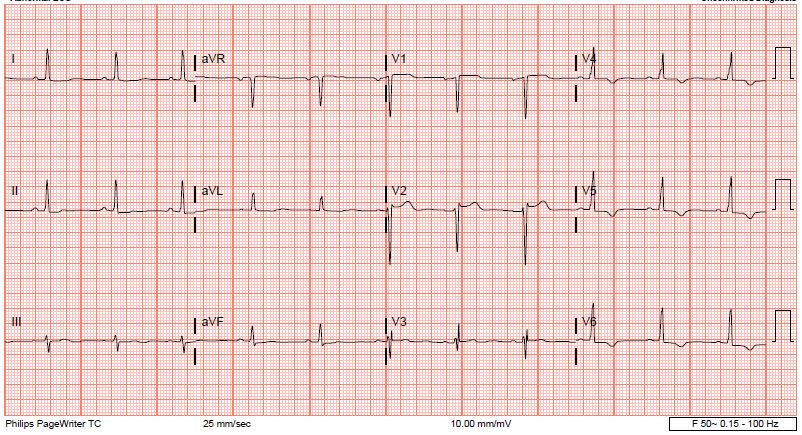
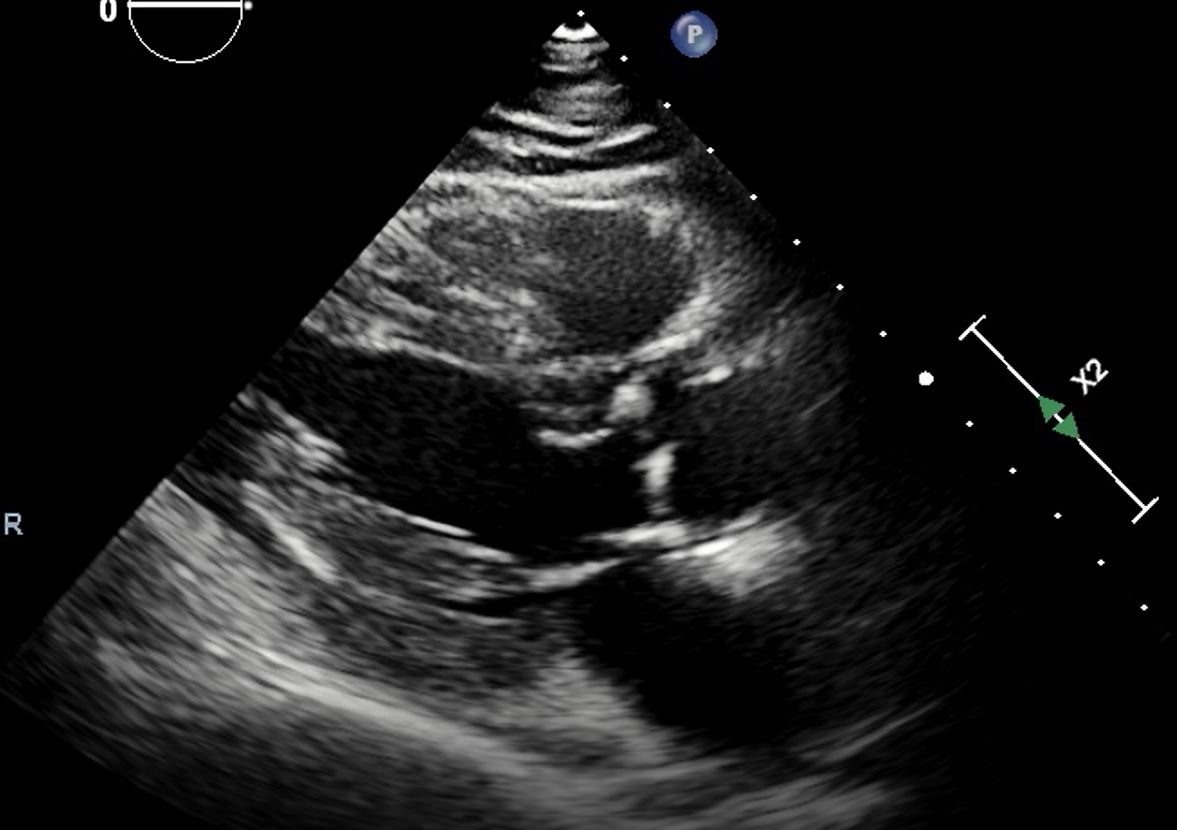
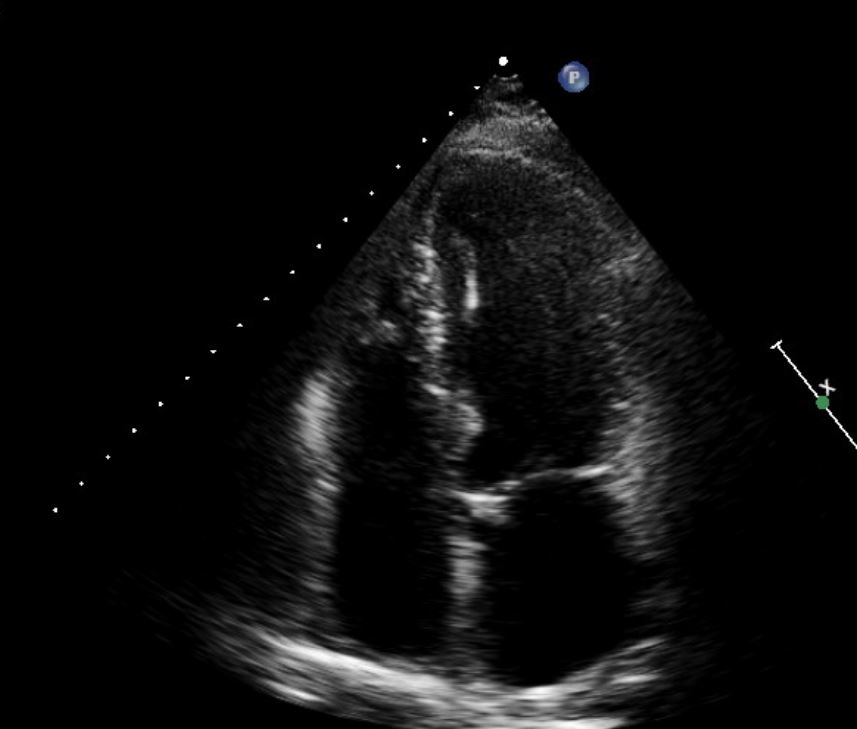
61 year old man with history of hypertension and hyperlipidemia presented with chest pain and reduced effort tolerance. He has history of NSTEMI treated medically at a community hospital 1 month ago. Physical examination was uneventful; ECG showed Q waves in V1 and V2 with T inversions in V5 to V6. Echocardiogram showed preserved LVEF 50% with apical and posterior regional hypokinesia.MSCT was performed showing diffuse triple vessel disease.


Relevant Test Results Prior to Catheterization
BP: 110/56HR: 62 bpm regularphysical examination: uneventful
Echocardiogram: LVEF 50%, RMWA at apical and posterior; thickened aortic valve with no significant pathologyMSCT coronary artery: mixed calcified plaque with severe luminal stenosis in LAD, LCx and RCA

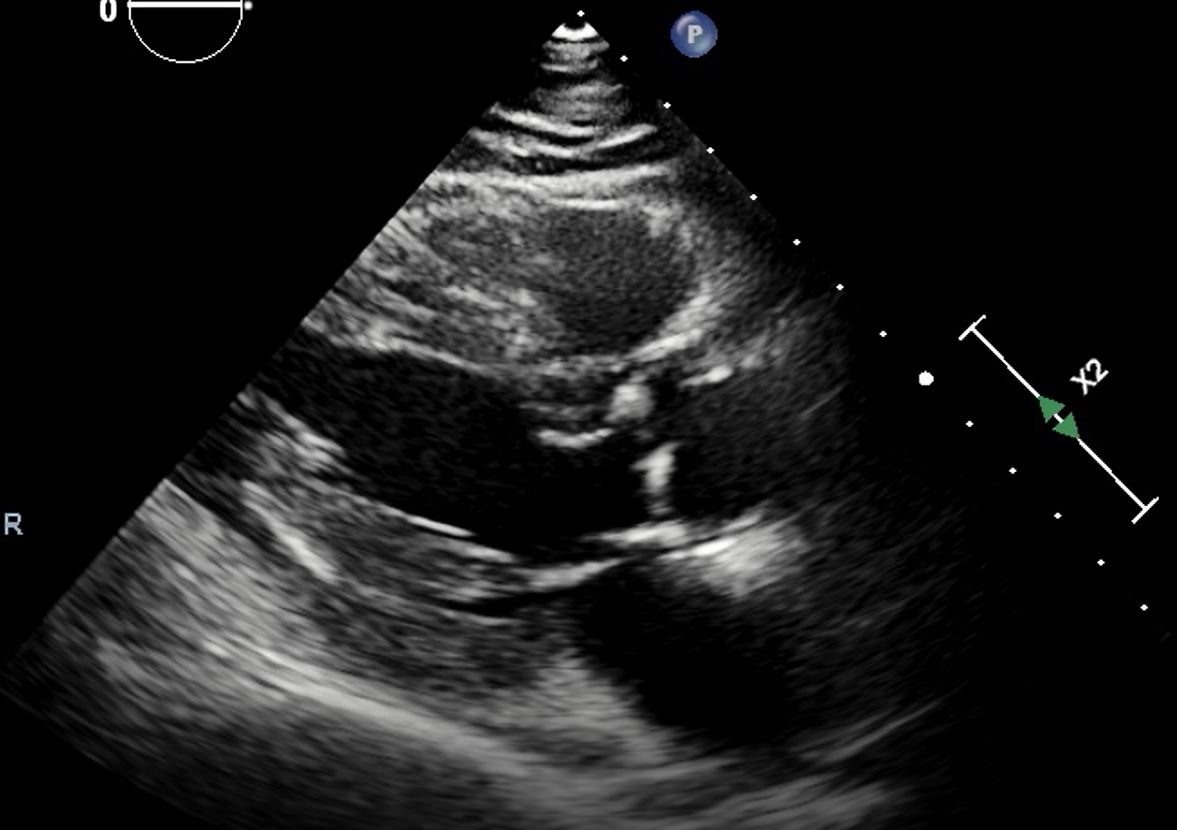
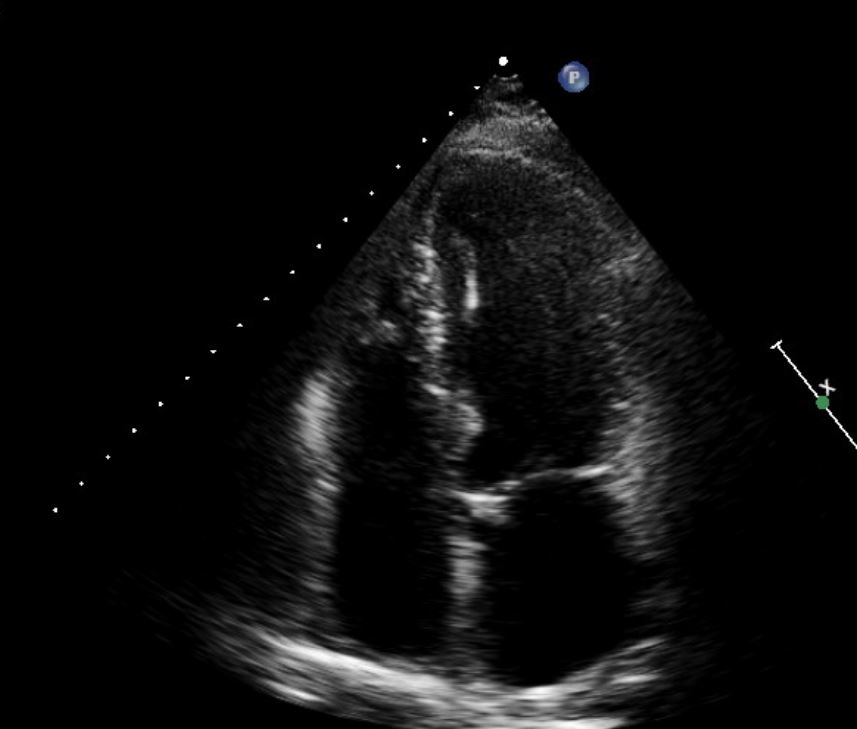
Echocardiogram: LVEF 50%, RMWA at apical and posterior; thickened aortic valve with no significant pathologyMSCT coronary artery: mixed calcified plaque with severe luminal stenosis in LAD, LCx and RCA

Relevant Catheterization Findings
Left main: short vesselLeft Anterior Descending: Diffuse tubular stenosis from ostium, near total occlusion in mid LAD after diagonal branch with TIMI 1 distal flowLeft Circumflex: Co-dominant vessel, severe stenosis in proximal OM 1; total occlusion mid OM2Right Coronary artery: Co-dominant vessel, multiple tandem severe stenosis in proximal and distal RCA; retrograde to distal LAD via posterior descending branch






Interventional Management
Procedural Step
The LCx OM lesion successfully treated with DCB 2.5 x 20mm.LAD proximal and distal vessel was visualized with dual injection. Lesion crossed with FIELDER-XT wire in CARAVEL microcatheter and position confirmed with retrograde injection. After predilatation with 1.5 balloon, noted a wedge shaped contrast retention in mid LAD with free-flowing jet of contrast originating from distal small branches causing suspicion of perforation. Prolonged balloon inflation resulted in resolution of the suspected extravasation. Urgent transthoracic ECHO showed no pericardial effusion and patient was hemodynamically stable. Further predilatation with SC 2.0 and scoring NC 2.5 balloons were done, with non flow limiting type B dissections in mid LAD. Proximal to mid LAD was stented with SYNERGY 2.5 x 38mm and distal lesion treated with two 2.0 x 20mm DCBs. Following DCB there was significant distal stent edge dissection which was treated with a SYNERGY 2.0 x 28mm stent. Postdilatation with NC 2.5 and NC 3.0 balloons completed the procedure.Final shots revealed persistence of small free flowing contrast jets, repeat bedside TEE showed no pericardial effusion. Patient was stable after 3 days observation with repeat TEE and discharged well.Staged PCI to RCA was planned a week later but patient defaulted and only readmitted after 2 months. Restudy angiogram showed persistence of contrast jets indicating likely Coronary Cameral Fistula into left ventricle. PCI to RCA done and patient discharged well.


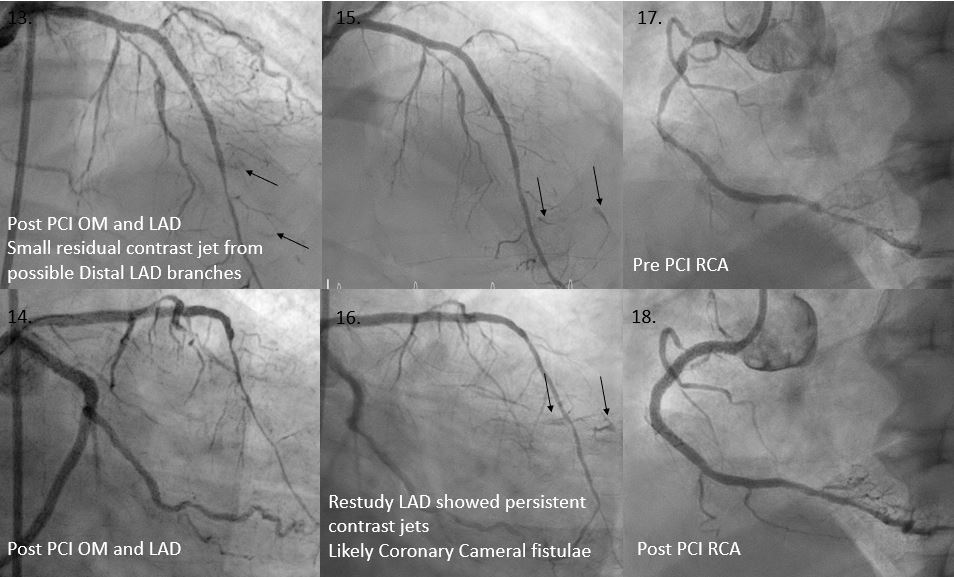


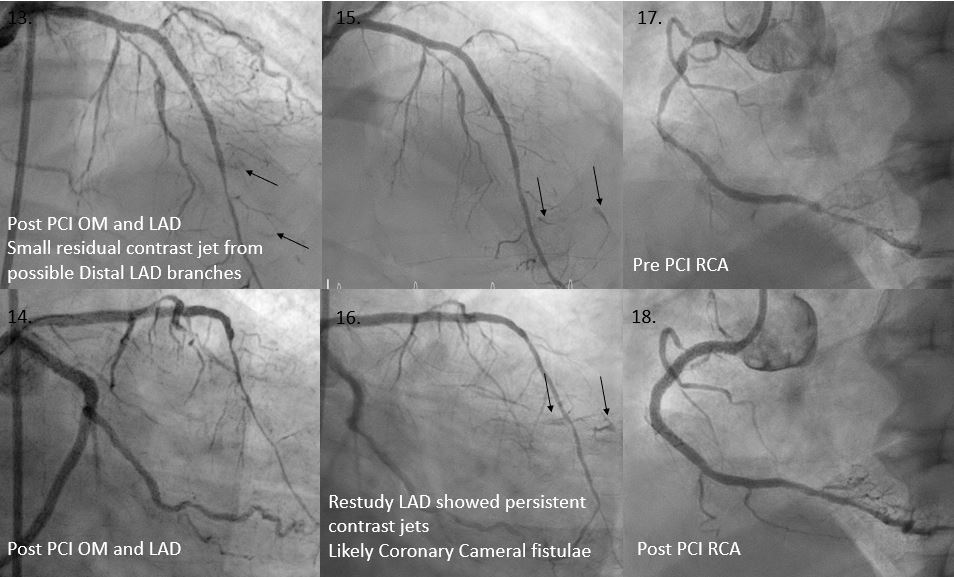
Case Summary
The commonest differential diagnosis for appearance of contrast extravasation during PCI is coronary artery perforation. Another possible differential is Coronary artery fistulae. Coronary cameral fistulae into cardiac chambers can be congenital or a rare complication of high atherosclerotic burden and myocardial injury following myocardial infarctions. In this case, it is likely the fistulae were unmasked following successful revascularization of the occluded LAD. Absence of pericardial effusion, hemodynamic stability and persistence of contrast jets in the restudy 2 months later highlights the likelihood of this diagnosis. Coronary cameral fistulae are usually managed conservatively well.

