Lots of interesting abstracts and cases were submitted for TCTAP 2024. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-178
Zero Is Not Bad at All - Zero Contrast PCI
By Pragathi Gurram, Anuj A. Kapadia, Swaroop Govind Bharadi
Presenter
Pragathi Gurram
Authors
Pragathi Gurram1, Anuj A. Kapadia2, Swaroop Govind Bharadi1
Affiliation
AIG Hospitals, India1, Care Hospitals, India2,
View Study Report
TCTAP C-178
Coronary - Imaging & Physiology - Invasive Imaging (IVUS, OCT, NIRS, VH, etc)
Zero Is Not Bad at All - Zero Contrast PCI
Pragathi Gurram1, Anuj A. Kapadia2, Swaroop Govind Bharadi1
AIG Hospitals, India1, Care Hospitals, India2,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
A 38 year male, know case of diabetes, chronic kidney disease, recent Acute coronary syndrome – NTSEMI, post PCI to LCX with residual significant stenosis in LAD – D1, recovered acute kidney injury post procedure (baseline creatinine, 1.7 mg/dL elevated to 2.7 mg/dL). He presented with ACS – USA, in sinus rhythm, blood pressure – 126/78 mm hg, pulse – 78/min, cardiovascular examination - normal.
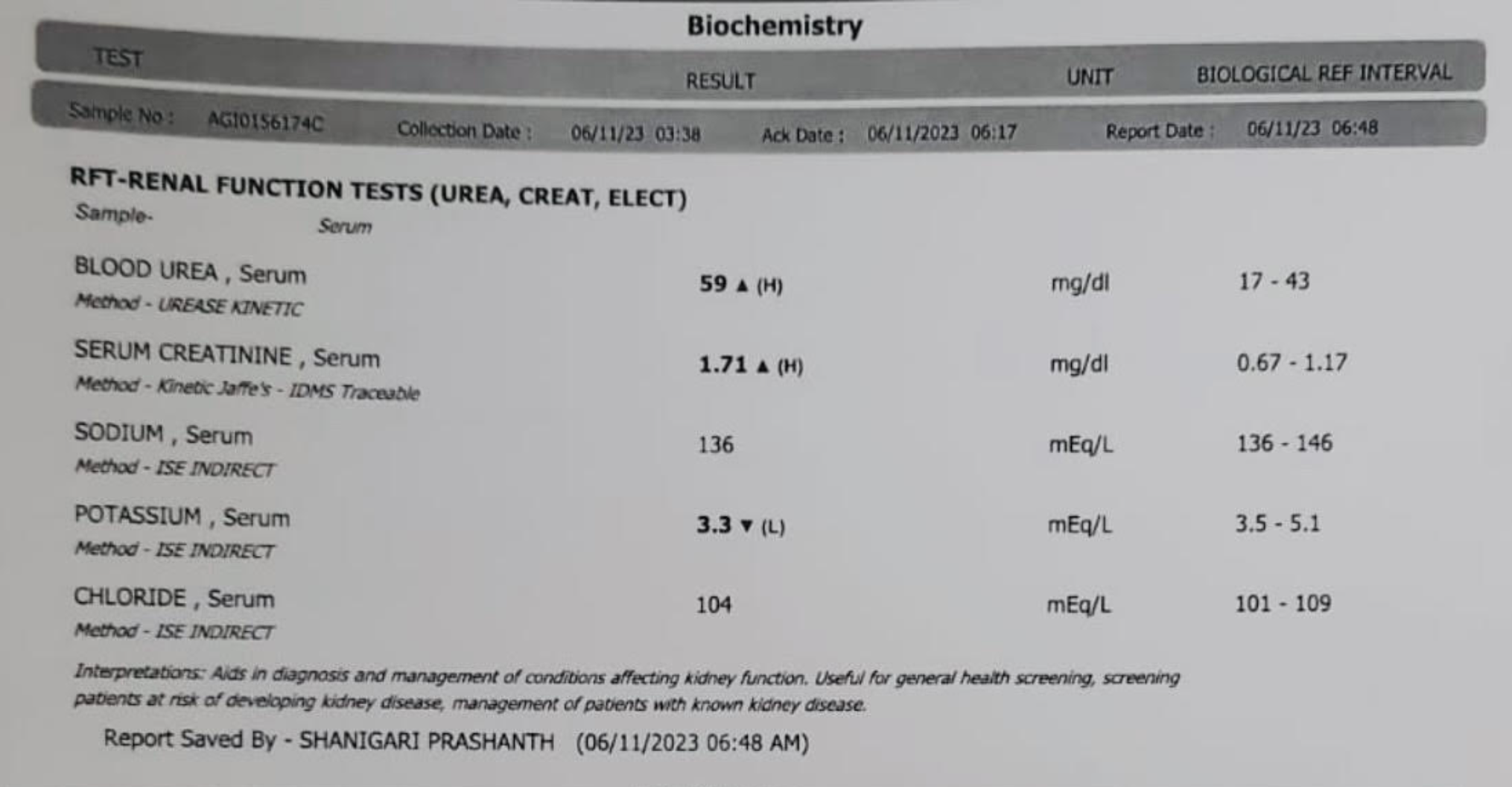
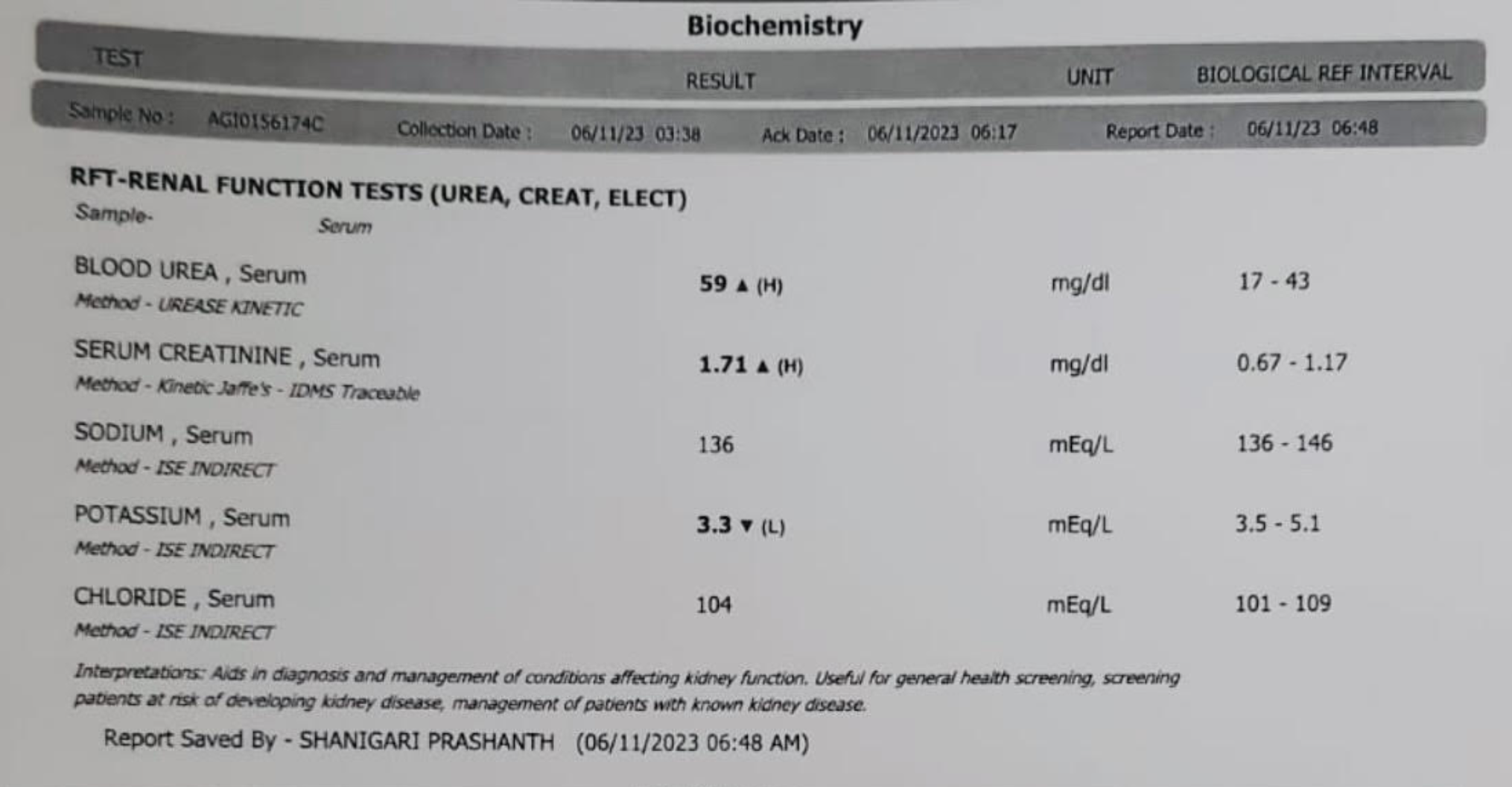
Relevant Test Results Prior to Catheterization
Hemoglobin - 13.5 g/dl, total leukocyte count - 6,500 cells/cu mm, platelet count - 2.3 lakhs, serum urea - 59 mg/dl, serum creatinine - 1.7 mg/dl, sodium - 136 m Eq/L, potassium - 3.5 m Eq/L, eGFR - 60 ml/min/1.73 m2. Electrocardiogram showed normal sinus rhythm with left ventricular hypertrophy and ST depression in lateral leads. 2D echo showed fair LV function with grade I diastolic dysfunction.


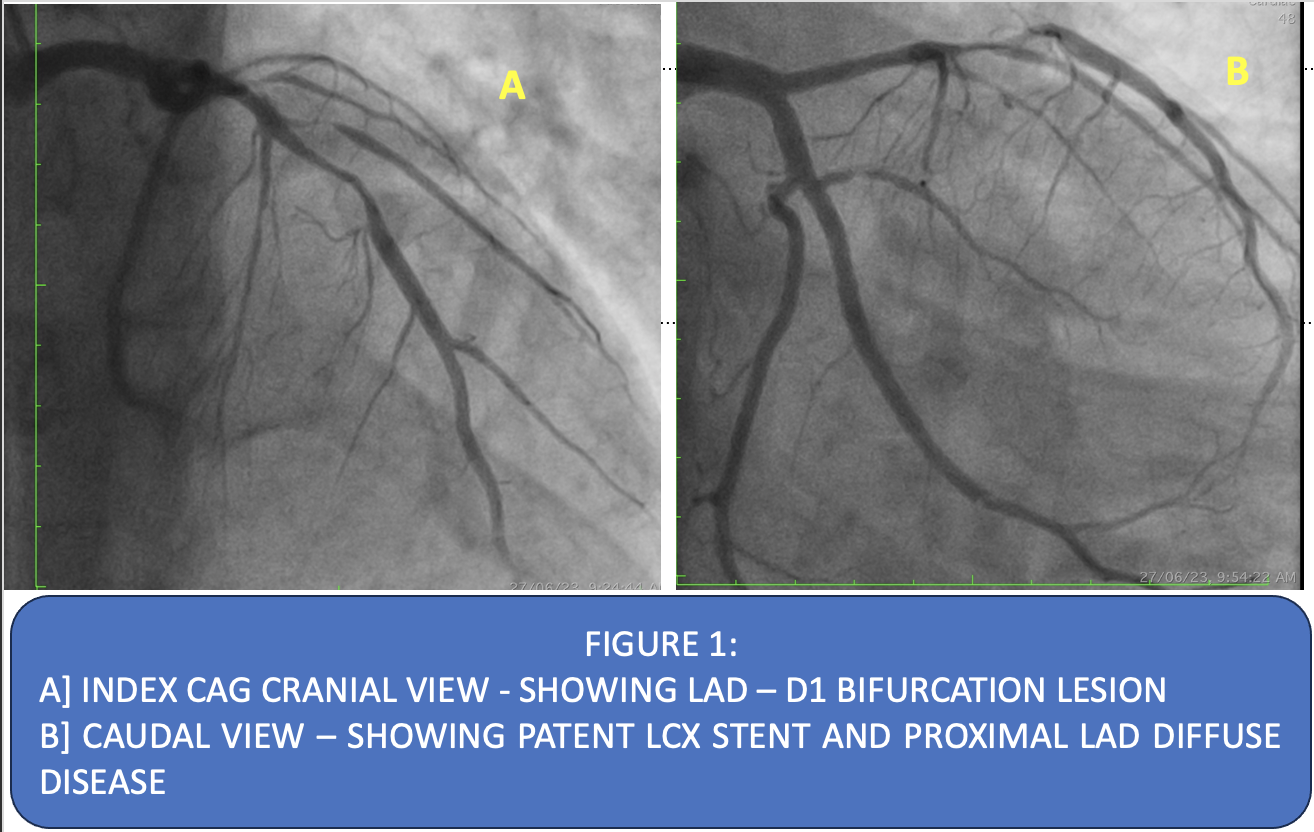
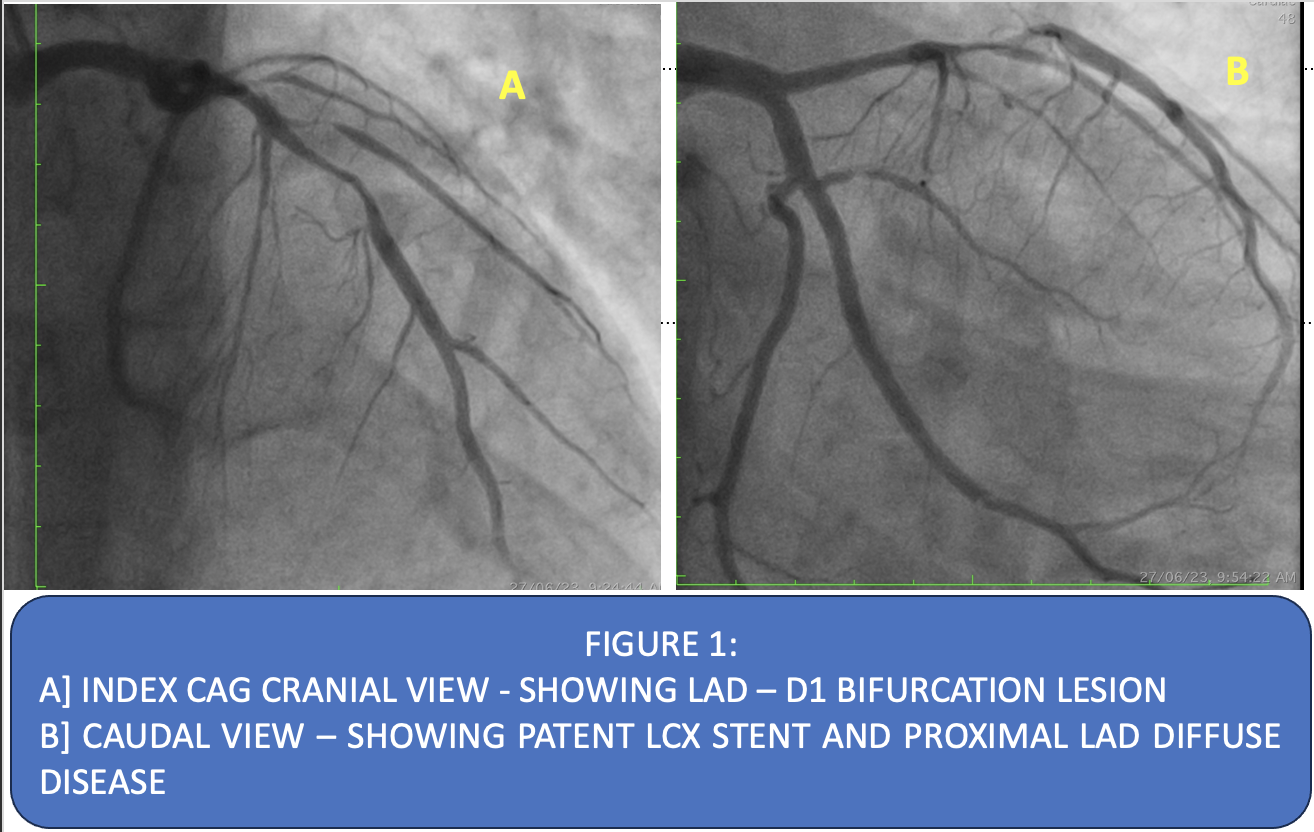
Relevant Catheterization Findings
Baseline coronary angiogram showed normal LMCA, LAD type – 3 with diffuse long segment disease extending to mid LAD, with critical narrowing at the level of first Diagonal with disease extending into it ( MEDINA – 1,1,1 ). Distal lad normal. LCX is non dominant with patent stent. OM normal. RCA is dominant system with mild plaquing. PDA, PLVB are normal.
Interventional Management
Procedural Step
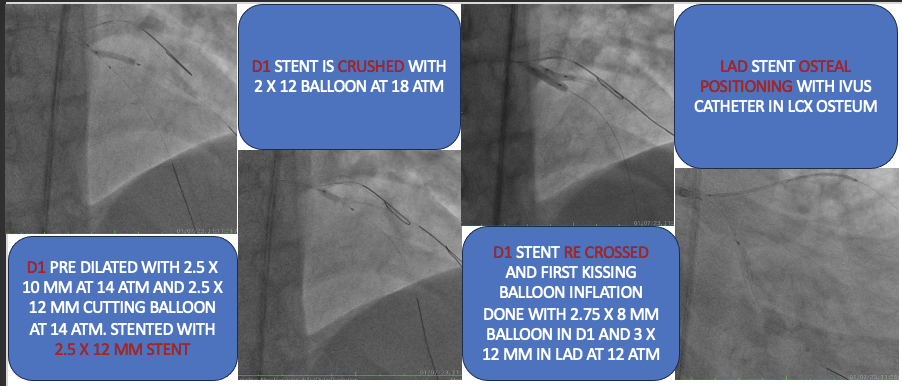
LMCA engaged with 6F XB 3.0. Engagement confirmed by 20ml saline infusion, which produced ST-T changes. LAD, D1, D2 are wired with workhorse wires making an EXOSKELETON of the indexed coronary. First IVUS run of D1 showed significant long segment disease in Diagonal (> 10 mm), vessel diameter was 2.25-25 mm with tight ostial involvement. Hence planned for dedicated “TWO STENT STRATEGY”. IVUS run of LAD showed diffuse disease with significant plaque burden all over above diagonal with disease extending upto ostium. Distal landing zone is 3 mm distal to distal septal. Length of lesion was around – 36 mm hence we decided to use 38 mm stent. PLAN- [1]Dedicated 2 stents – we selected DKC. [2] Moderate bed preparation of lesion in LAD [3] LAD – Long stent till Ostium [4] IVUS guided positioning of stent in LAD ostium. Diagonal was stented with 2.25 x 12 mm stent and post dilated with 2.75 x 8 mm balloon, and first kiss done with 3 X 12 mm NC in LAD and 2.75 x 8 mm NC in Diagonal. Bed preparation in LAD was done with 3 mm NC balloon. LAD stented with 3 x 38 mm stent with ivus guidance (ivus catheter In LCX ostium). Final kissing was done with 2.75 x 12 mm NC and 3.5 X 12 mm NC in LAD, followed by POT in LAD with 4 X 8 mm POT balloon.
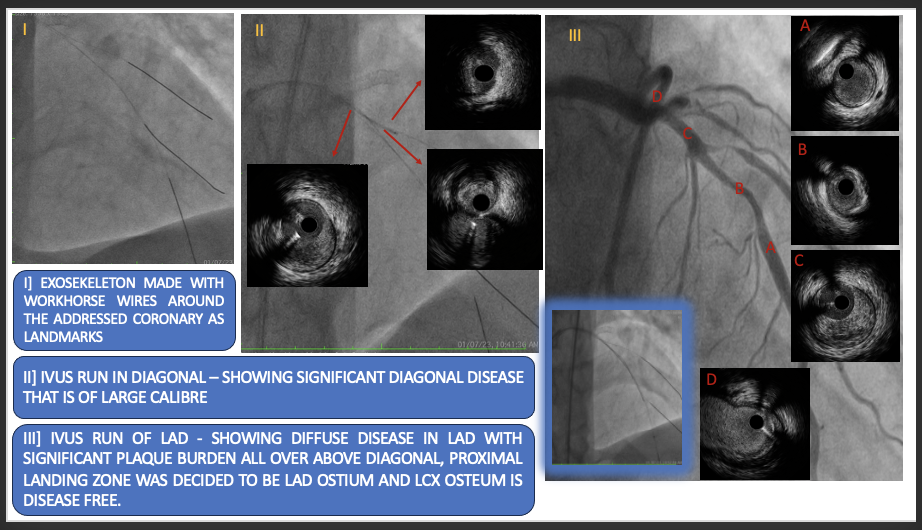
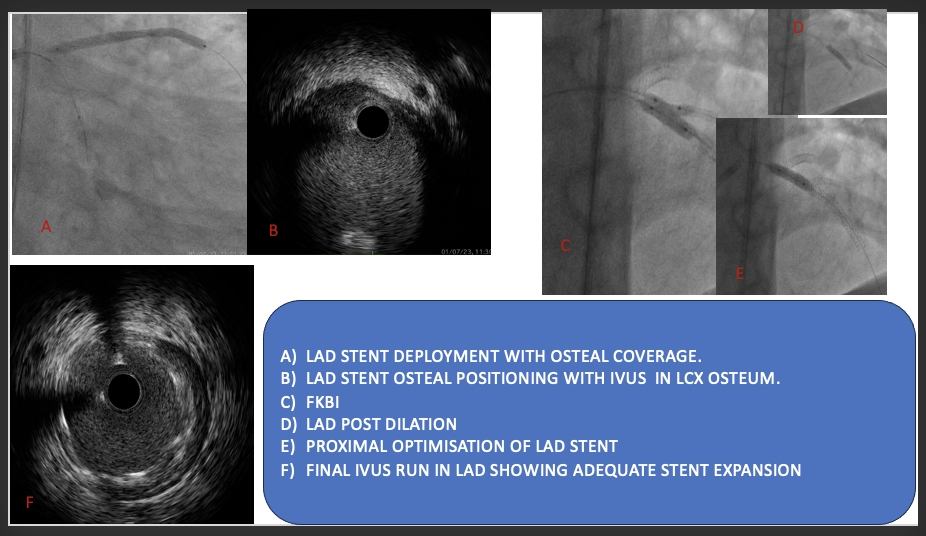
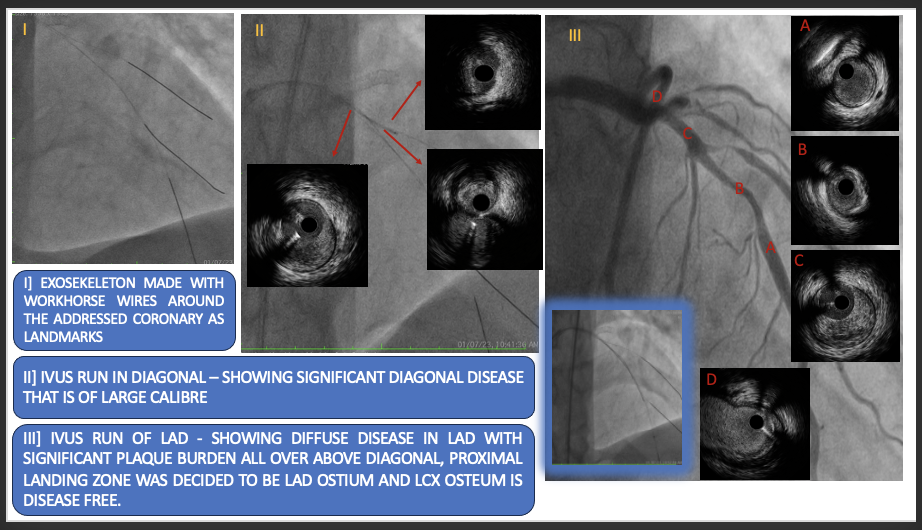
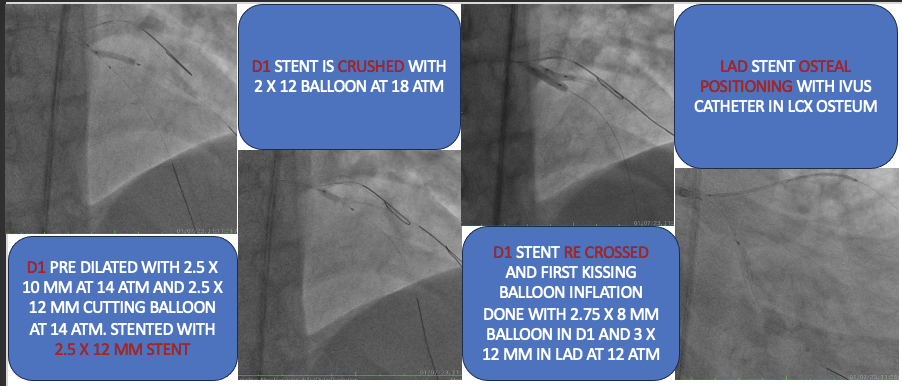
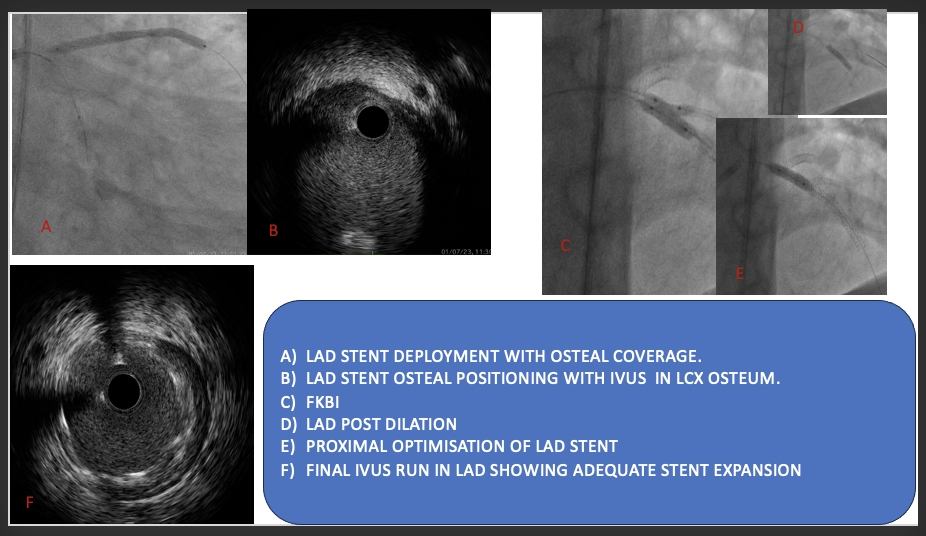
Case Summary
IVUS helped in stent sizing and choosing bed preparation strategy. Here the lesion is fibrotic with no thrombus and calcium. Hence aggressive bed preparation is not required. IVUS helped in zero contrast percutaneous coronary intervention in a complex bifurcation and ostial intervention which is very important for renal protection. Doing manual IVUS run in LCX-LMCA helps in exact positioning of LAD ostial stent.
|
Mohammad Shafiqur Rahman Patwary (NATIONAL INSTITUTE OF CARDIOVASCULAR DISEASES) Apr 25, 2024
|
|
| Good job. Cutting balloon in D1 is essential in this case? | |

