Lots of interesting abstracts and cases were submitted for TCTAP 2024. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-122
Stent Balloon Loss in Complex Coronary Intervention : How We Handle It
By Shi-Chue Hsing, Yen-Lien Chou
Presenter
Shi-chue Hsing
Authors
Shi-Chue Hsing1, Yen-Lien Chou1
Affiliation
Tri-Service General Hospital, Taiwan1,
View Study Report
TCTAP C-122
Coronary - Complication Management
Stent Balloon Loss in Complex Coronary Intervention : How We Handle It
Shi-Chue Hsing1, Yen-Lien Chou1
Tri-Service General Hospital, Taiwan1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
The 50 y/o man has a history of DM nephropathy leading to ESRD requiring maintenance HD. He underwent coronary artery stenting in the middle to distal RCA five years ago, experienced IE post AVR with CABG using a vein graft to the LAD, and had AVB following PPM implantation three years ago.Recently, he presented with symptoms of respiratory distress, orthopnea, and lower limb edema, leading to his intubation upon arrival. He was admitted for decompensated HF and NSTEMI.
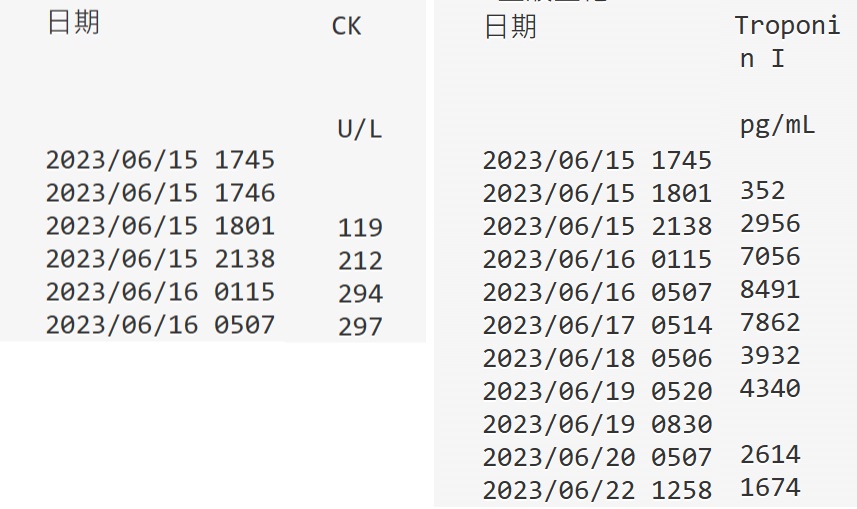


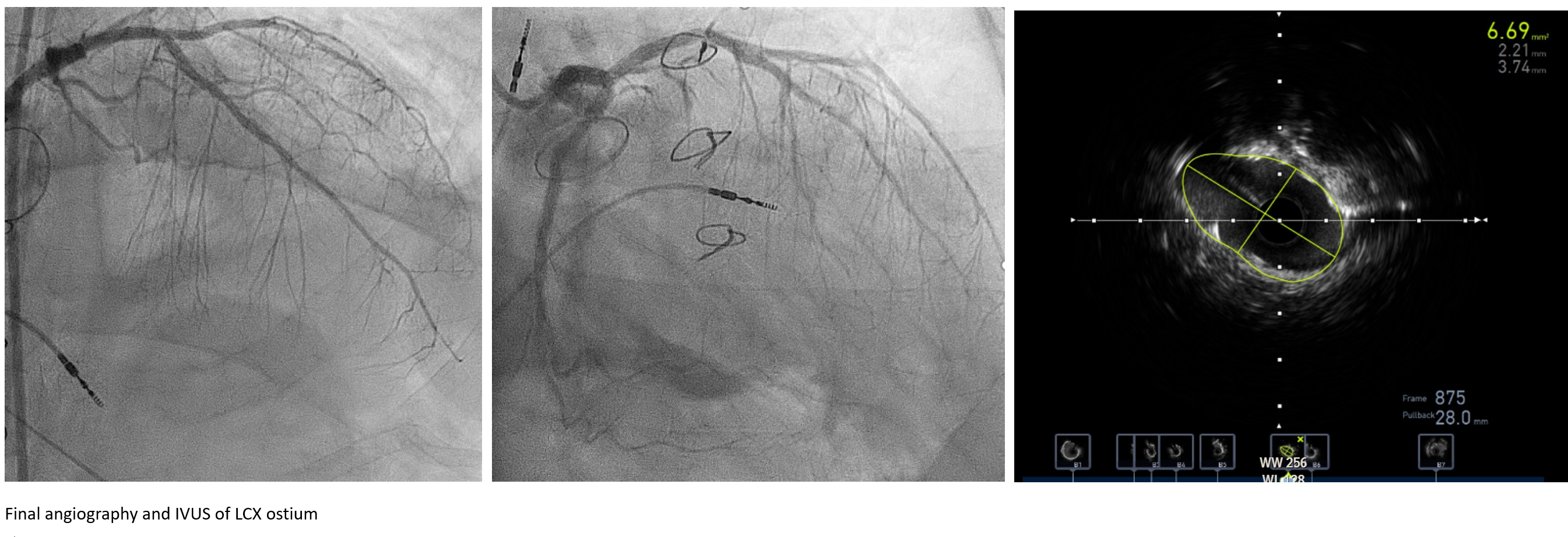
Relevant Test Results Prior to Catheterization
The EKG revealed an AV dual pacing rhythm, while the cardiac echo displayed overall reduced contractility (general hypokinesia) with an ejection fraction (EF) of 35%. Notably, his cardiac troponin I levels were significantly elevated at 7862 pg/mL (normal range <40). Given these findings, he was scheduled for cardiac catheterization.
Relevant Catheterization Findings
A 60% stenosis at the d-LM, an 80% diffuse disease from the p~m-LAD, and a bifurcation lesion at the ostium to the p-DB, oculuded VG to the LAD. The d-LAD showed CTO or critical stenosis with collateral supply from the RCA. A CTO of the LCX was also noted. The RCA showed 95% ISR at the d-RCA stent. The family chose multivessel PCI over redo-bypass. PCI treated the RCA stent, followed by a complex PCI, managing CTO in the LAD and LCX, and addressing the complex LM bifurcation over several days.






Interventional Management
Procedural Step
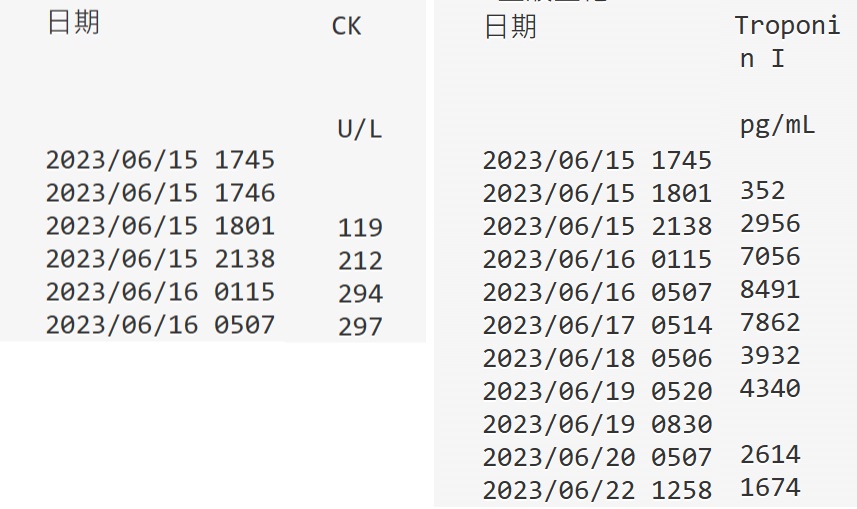
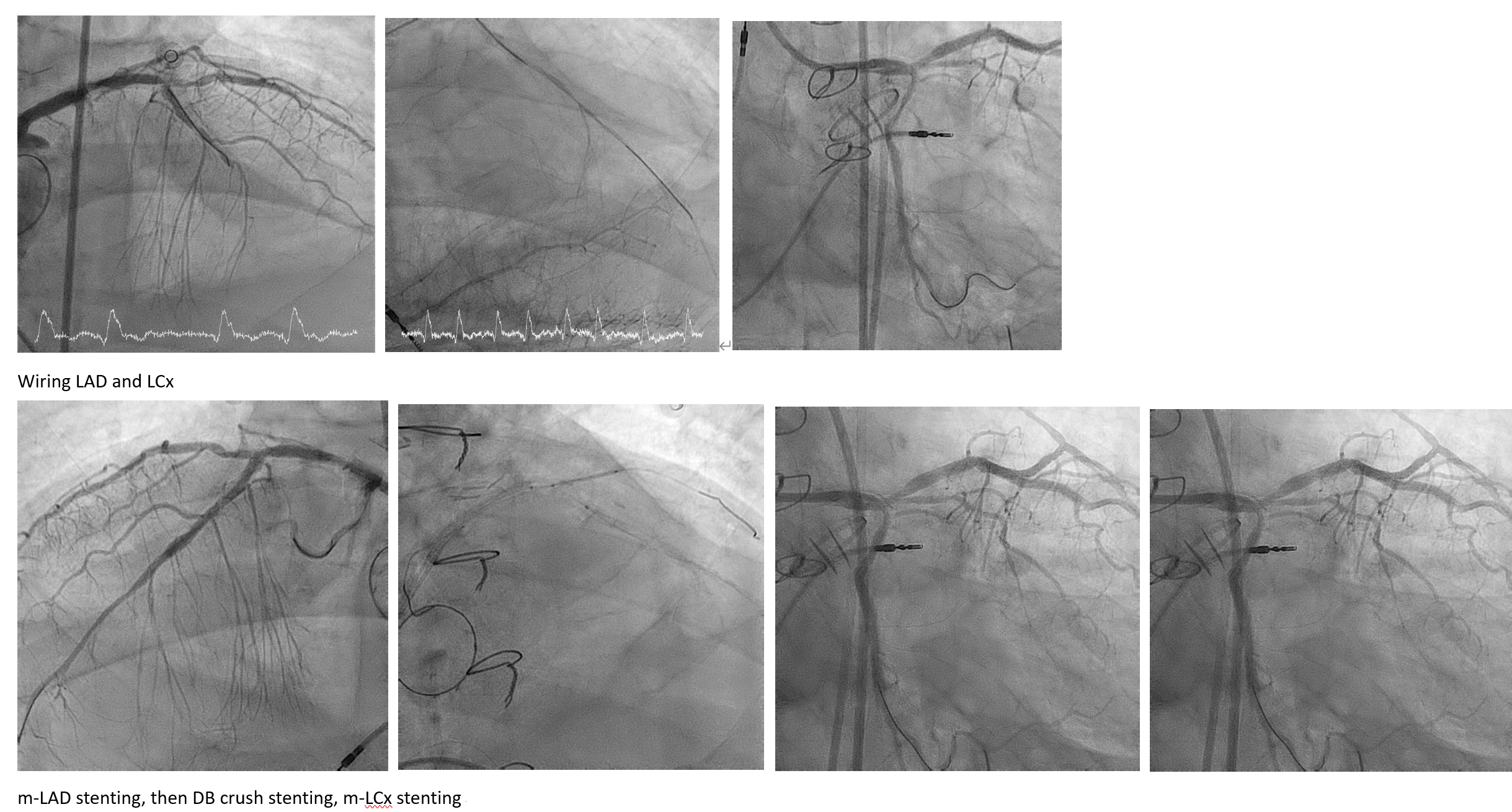
Bilateral contrast injection facilitated the management of LAD CTO. SION in Cosair easily wired into the d-LAD. Gaia1 in Cosair was used to wire the LCX successfully. Lesion opening in the LAD and LCX was achieved, followed by IVUS. Preparatory steps involved series balloon dilation and cutting balloon techniques. Stent placement ensued, including a 2.25X39mm DES in the m-d~LAD, crush stenting in DB, and stenting in the p~m-LAD and m-LCX with varying DES sizes. Culotte LM stenting was considered. A 3.0X15mm DES was advanced to p-LCX but faced challenges in advancement. During deployment, the stent didn’t fully expand, leading to retention of the stent balloon (Shaft fractured just before the balloon). To resolve this, wires were used to rewire the LCX, and a wiggle wire was inserted into the LCX. Series of balloon dilation was employed to crush the stent. Distal balloon retrieval was tried but failed. Snail to grab the stent balloon, also failed. IVUS imaging indicated successful preparation of the LCX and the stent balloon not protruding into the aorta. Consequently, the decision was made to 'externalize' the stent balloon by covering it with a new DES. A nono-T stent, sized at 3.0X15mm, was deployed to LAD. The LM~ pLCx lesion was stented with a 3.5X26mm DES. Post-dilation in the LM, followed by rewiring to the LAD and LCx and a KBT were performed. IVUS evaluation indicated an adequate result for the LAD and LCX MSA. The final angiography showed good result.
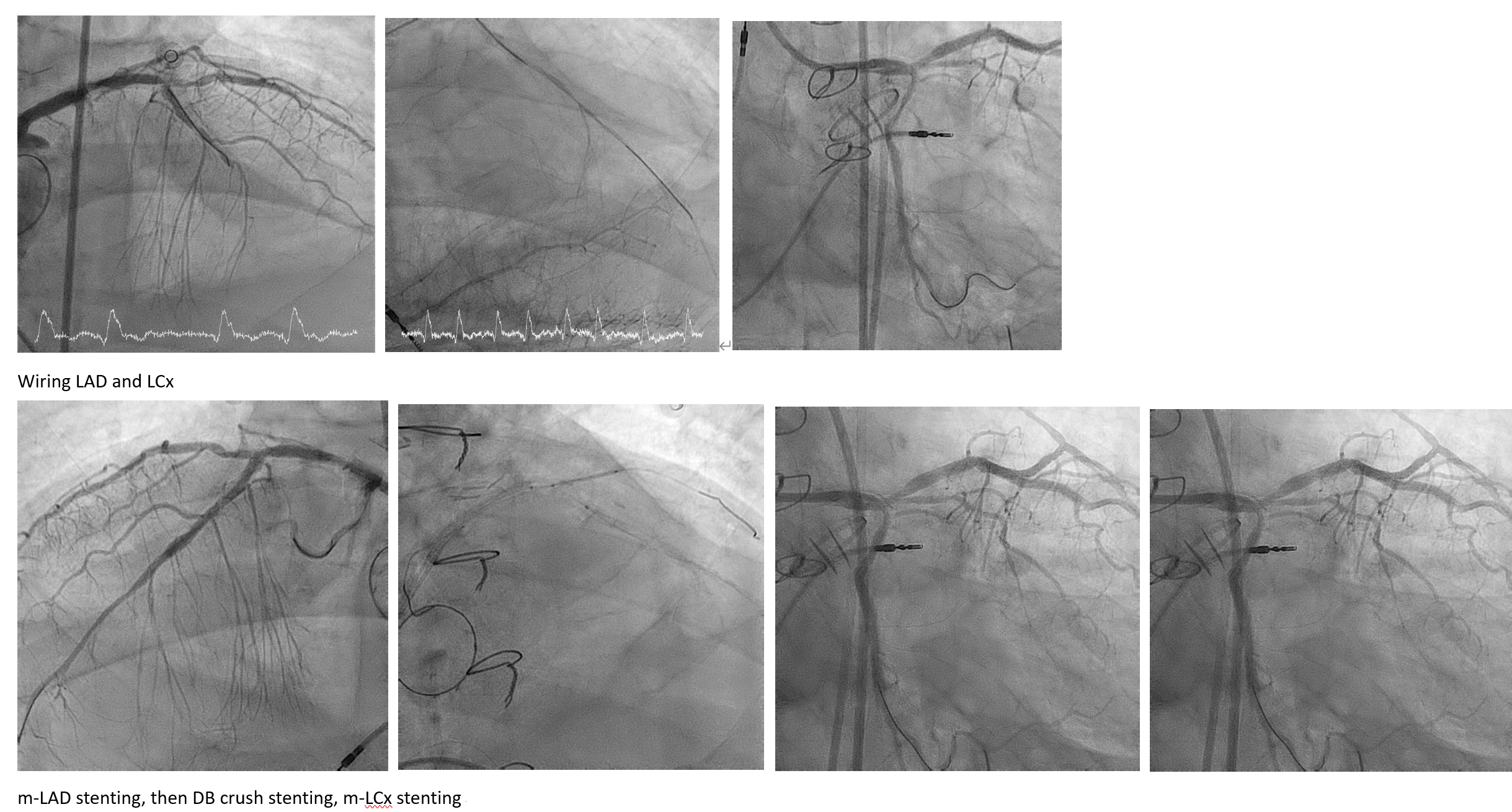


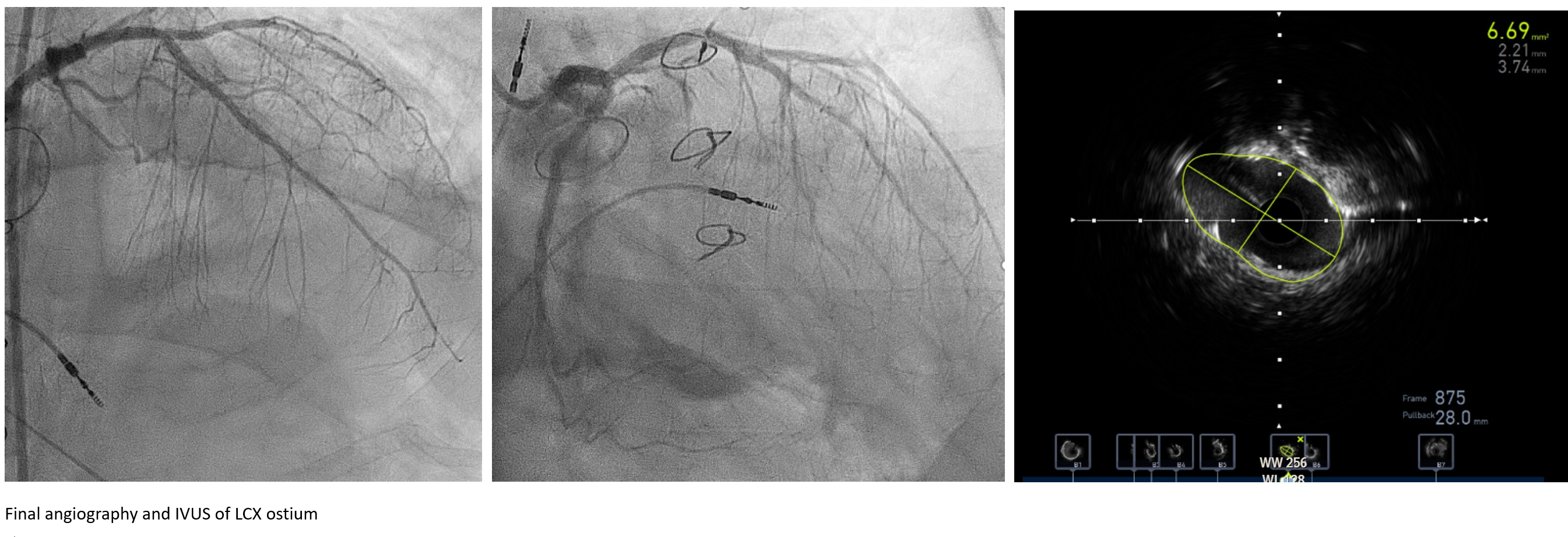
Case Summary
Encountering a heavily calcified lesion at an acute angle posed challenges during stent dilation, complicating stent removal. The coronary wire's positioning was pivotal, but the presence of a stent balloon impeded device advancement. Repositioning the wire, we used balloon dilations to crush the stent. Distal balloon retrieval and snaring attempts failed. Ultimately, we opted to stent the vessel, covering the stent balloon. IVUS confirmed success with effective coverage. Post-treatment, the patient was extubated promptly. This case emphasizes the importance of thorough lesion preparation and the use of supportive tools when dealing with calcified or tortuous vessels.

