Lots of interesting abstracts and cases were submitted for TCTAP 2024. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-186
Magic Touch: Intervention for Stenosis, Plaque, and Ischemia Without Devices
By Haechan Cho, Bon-Kwon Koo
Presenter
Haechan Cho
Authors
Haechan Cho1, Bon-Kwon Koo1
Affiliation
Seoul National University Hospital, Korea (Republic of)1,
View Study Report
TCTAP C-186
Coronary - Imaging & Physiology - Non-Invasive Imaging (CTA, MRI, Echo, etc)
Magic Touch: Intervention for Stenosis, Plaque, and Ischemia Without Devices
Haechan Cho1, Bon-Kwon Koo1
Seoul National University Hospital, Korea (Republic of)1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
A 51-year-old Korean male with a history of chronic alcoholism and untreated dyslipidemia presented to the hospital with exertional chest pain and dyspnea. Physical examination and an electrocardiogram were unremarkable, but initial blood tests showed triglyceride (TG) at 247 mg/dL, low-density lipoprotein (LDL) cholesterol at 92 mg/dL, and high-density lipoprotein (HDL) cholesterol at 38 mg/dL (Figure 1).


Relevant Test Results Prior to Catheterization
To evaluate the coronary artery, a coronary computed tomographic angiography (CCTA) was conducted. The CCTA revealed a 90% stenosis at the proximal left anterior descending (LAD) artery-diagonal branch bifurcation (Figure 2). Although he was advised to undergo invasive coronary angiography for further evaluation and treatment, he refused. Consequently, he was prescribed 10 mg of Rosuvastatin, 100 mg of Aspirin, and 5 mg of Nebivolol per day.


Relevant Catheterization Findings
Five years later, the patient reported improvement but still complained of residual chest discomfort. Blood tests and a CCTA were performed again. Triglyceride (TG) levels (239 mg/dL) and HDL-cholesterol (39 mg/dL) showed no significant changes, but LDL-cholesterol decreased by half to 49 mg/dL (Figure 1). On the follow-up CCTA, the stenosis at the proximal LAD-diagonal branch bifurcation had improved to 30%, compared to 90% five years ago (Figure 3).


Interventional Management
Procedural Step
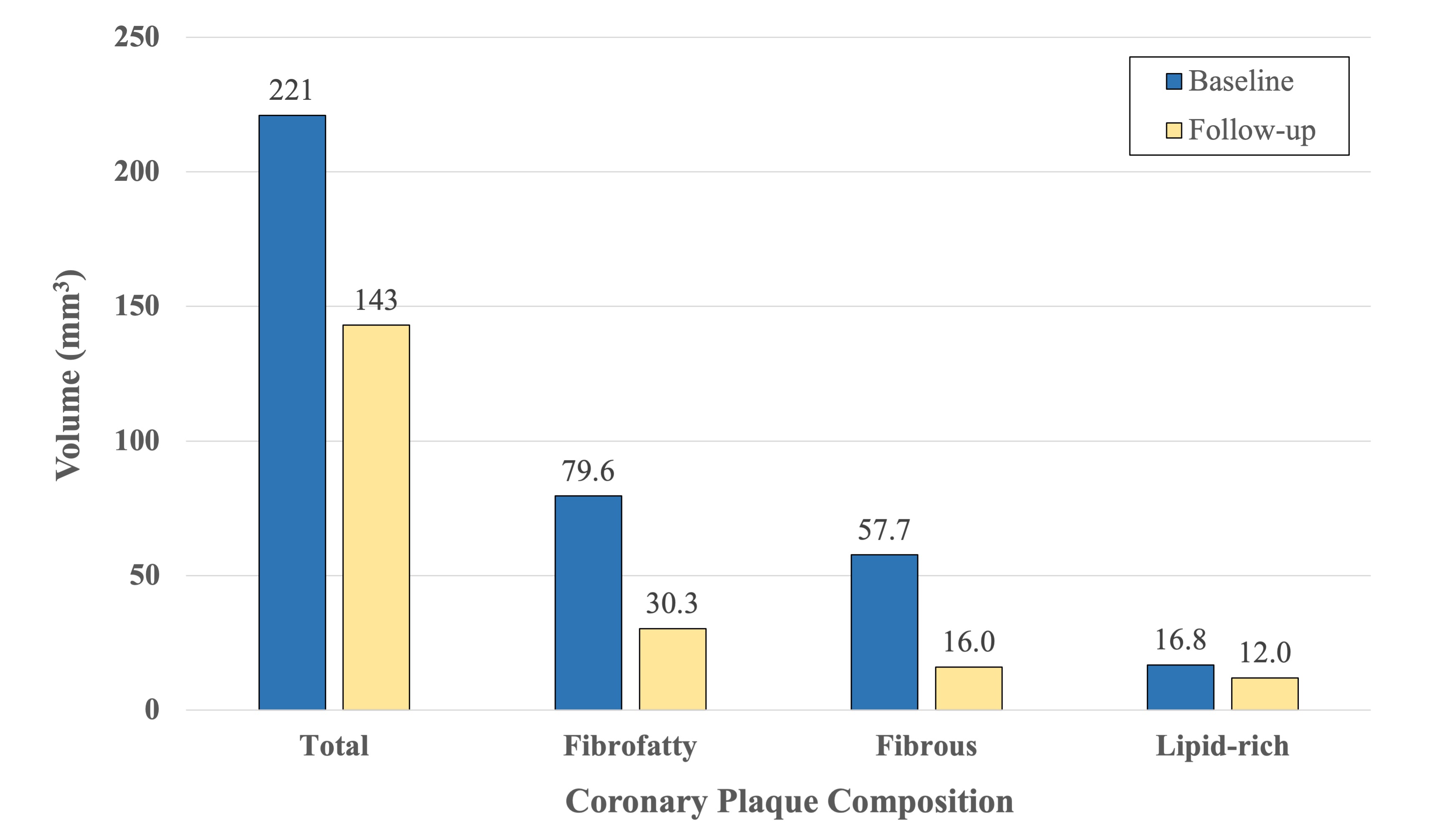
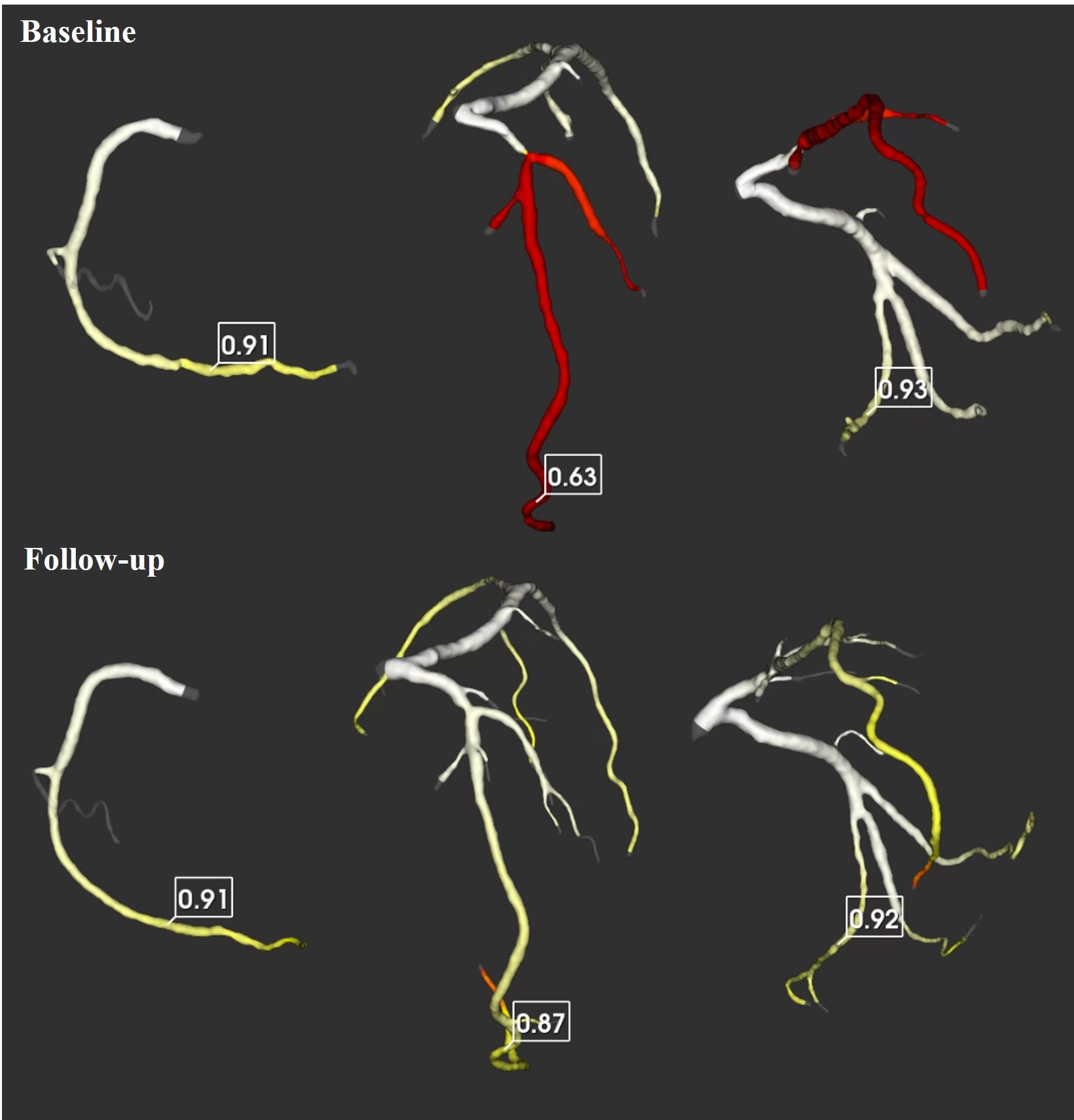
To assess coronary plaque and stenosis more precisely and quantitatively, coronary plaque analysis and fractional flow reserve-computed tomography (FFRCT) were applied to the CCTA scans of the patient. In coronary plaque analysis, the total plaque volume, measured from the midpoint of the proximal LAD to the first septal branch (Figure 4), decreased from 221 mm3 to 143 mm3 over five years. Regarding the tissue composition of the coronary plaque, there was a significant reduction in fibrotic and fibrofatty tissue (57.7 to 16.0 mm3 and 79.6 to 30.3 mm3, respectively, Figure 5). The FFRCT of the right coronary artery (RCA) and the left circumflex artery (LCX) did not change significantly ([RCA] 0.91 to 0.91, [LCX] 0.93 to 0.92). However, the FFRCT of the LAD improved from 0.63 to 0.87 without invasive treatment (Figure 6).

Case Summary
Drastic regression of coronary atherosclerosis plaque is uncommon. The findings in this case demonstrate that, in certain patients with coronary artery disease, lipid-lowering therapy without invasive treatment can be effective not only in reducing plaque volume but also in improving blood flow. The evaluation of coronary plaques and stenoses can be enhanced through more sophisticated and precise methods such as coronary plaque analysis and FFRCT.

