Lots of interesting abstracts and cases were submitted for TCTAP 2024. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-123
Transient Collateral Augmentation: A Saviour During the Storm
By Devan Jothiprahasam, Prem Arumuganathan, Muhamad Ali SK Abdul Kader, Kamaraj Selvaraj, Mohd Ruslan Mustapa, Abd Kahar Abd Ghapar
Presenter
Mohd Ruslan Mustapa
Authors
Devan Jothiprahasam1, Prem Arumuganathan1, Muhamad Ali SK Abdul Kader1, Kamaraj Selvaraj1, Mohd Ruslan Mustapa1, Abd Kahar Abd Ghapar1
Affiliation
Sultan Idris Shah Serdang Hospital, Malaysia1,
View Study Report
TCTAP C-123
Coronary - Complication Management
Transient Collateral Augmentation: A Saviour During the Storm
Devan Jothiprahasam1, Prem Arumuganathan1, Muhamad Ali SK Abdul Kader1, Kamaraj Selvaraj1, Mohd Ruslan Mustapa1, Abd Kahar Abd Ghapar1
Sultan Idris Shah Serdang Hospital, Malaysia1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
A 47 year old gentleman who is a smoker with comorbidities of dyslipidemia and hypertension, presented with a history of crescendo chest pain and shortness of breath for a duration of five days. Physical examination was unremarkable. A diagnosis of NSTEMI was established from the ECG and cardiac biomarkers. Vital signs were stable on presentation. Since he presented in a non-PCI capable centre, he was subsequently referred to us for an urgent coronary intervention.
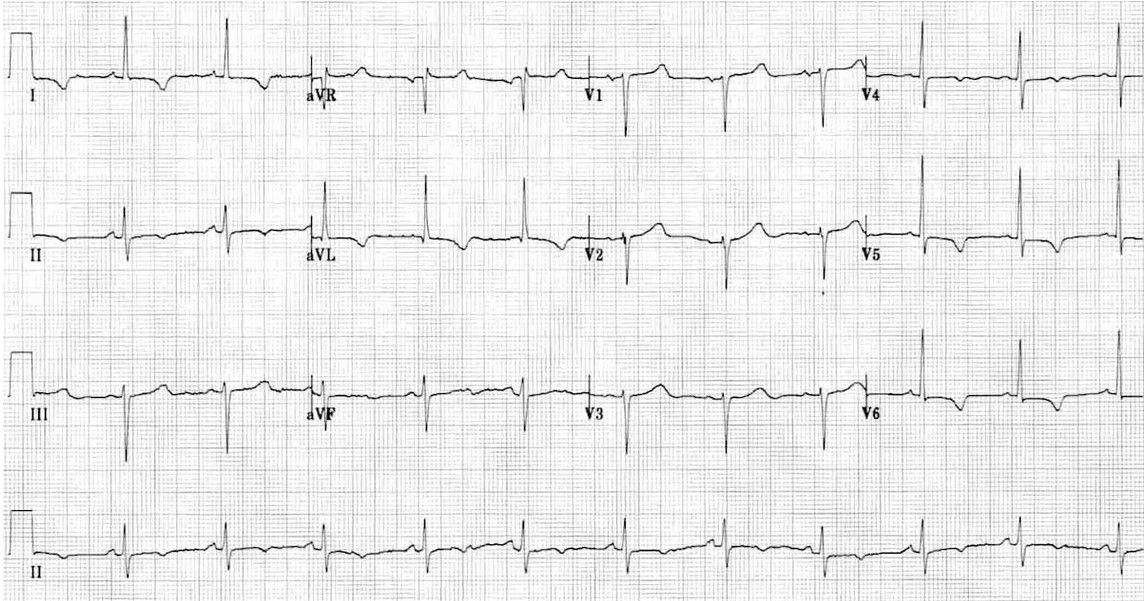
Relevant Test Results Prior to Catheterization
Troponin was raised and electrocardiogram showed T inversion and ST depression over the lateral leads. Echocardiogram showed a mildly reduced LVEF of 50% with hypokinesia over the anterolateral and inferolateral walls.
Relevant Catheterization Findings
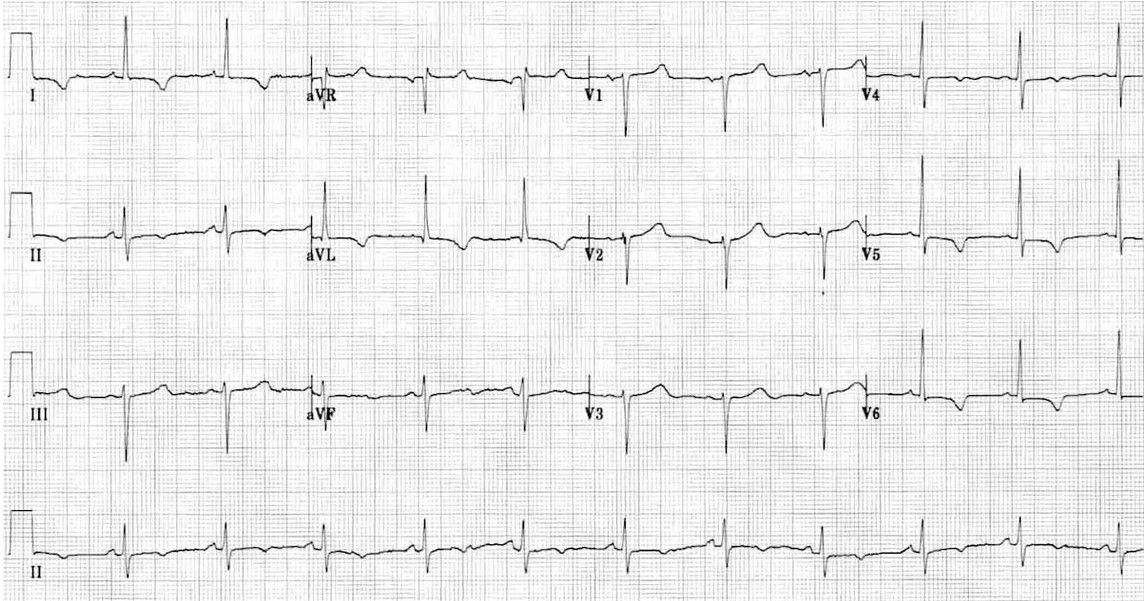
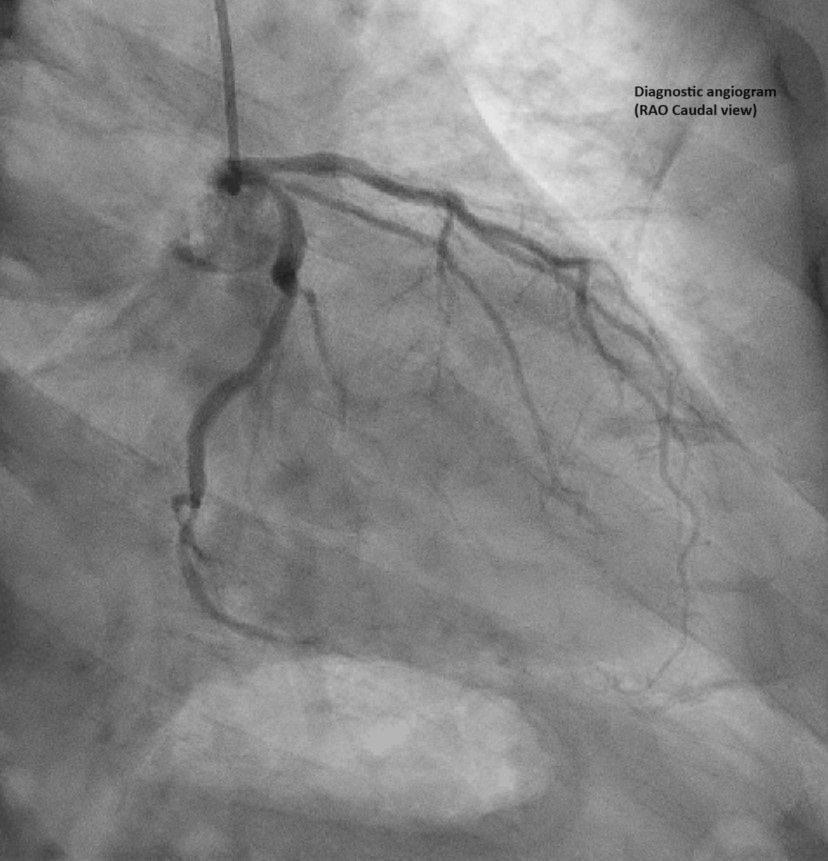
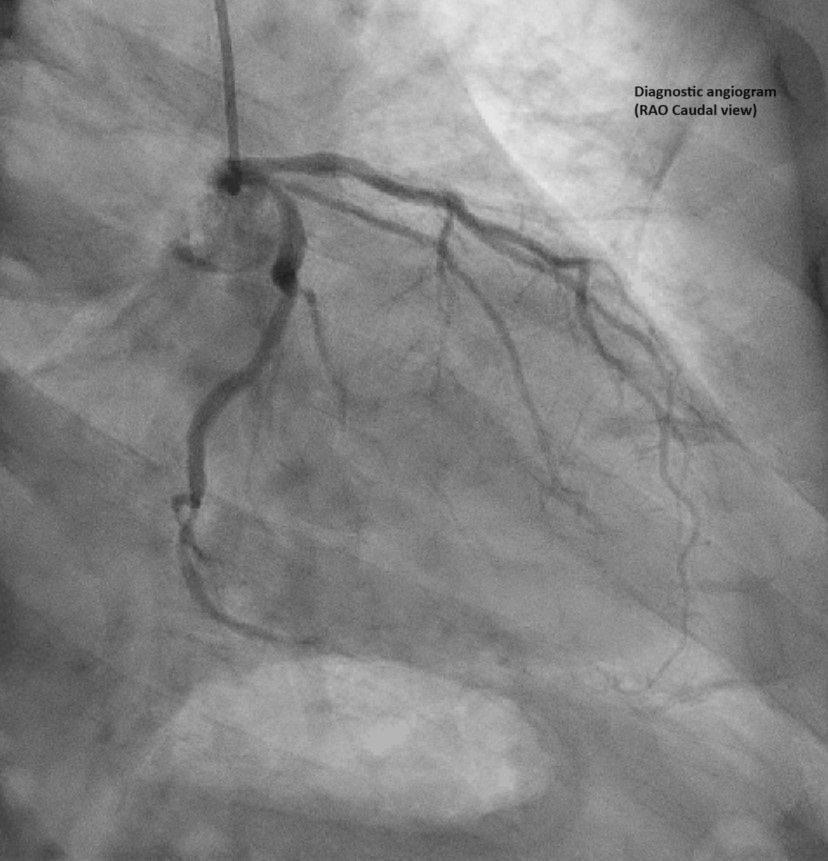
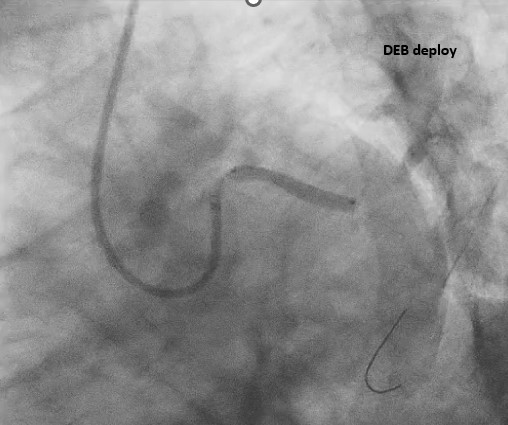
Coronary angiogram done showed single vessel disease with ostial left circumflex 70-80% stenosis. Both the left anterior descending (LAD) and right coronary arteries were smooth. PCI was done to the left circumflex lesion with a 6Fr EBU 3.0 guiding catheter and Sion Blue workhorse wire. The lesion was predilated sequentially from proximal to ostial with a 3.0 x 15 mm scoring and a 3.5 x 15 mm non compliance balloons. A 4.0 x 30 mm drug eluting balloon(DEB) was deployed at the ostial circumflex.


Interventional Management
Procedural Step
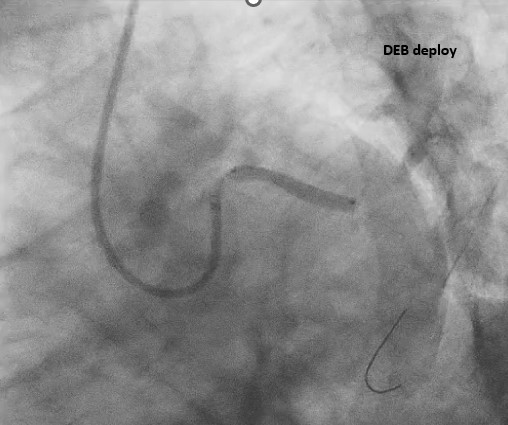
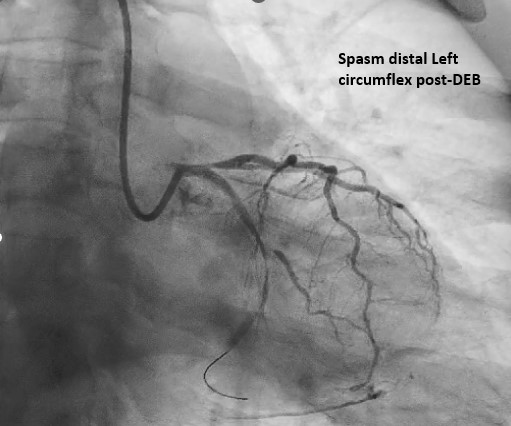
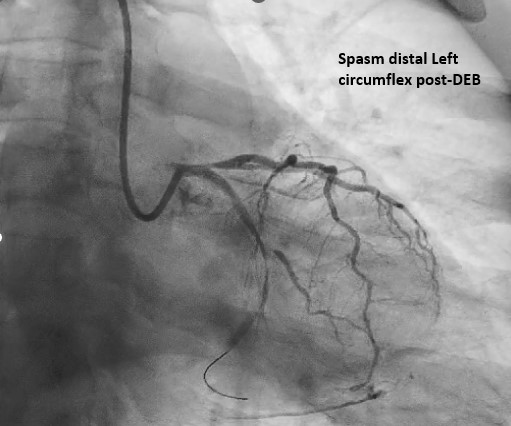
Post DEB deployment, patient developed immense chest pain and repeated angiogram showed severe coronary spasm in distal left circumflex with TIMI 0 flow .ECG showed dynamic ST depression over the lateral leads with stable haemodynamics. Multiple intracoronary vasodilators (Isosorbide Dinitrate, Adenosine and Verapamil ) were given. Chest pain improved, however coronary spasm was persistent. There was presence of collaterals from distal LAD with retrograde filling into distal circumflex (transient collateral augmentation).This collateral augmentation helped in relieving the chest pain. During the course of this spasm, a 2.5 mm semi-compliant balloon was advanced into the distal circumflex and multiple inflations were performed but were unsuccessful. Intracoronary Tirofiban was then administered over 3 minutes in view of long-standing spasm. A thrombus aspiration catheter was used to aspirate any possible thrombus formed over the site of spasm. Fortunately, no thrombus was aspirated. After almost 45 minutes (post PCI) of observing and administering the above treatment, a repeated angiogram showed refractory spasm with no flow distally. However, chest pain resolved and collaterals were still present (with retrograde flow). A decision to bail out and stent the spastic vessel was not taken as the patient was haemodynamically stable and pain free. A relook angiogram done two days later showed absence of spasm as well as dissection and the initial collaterals were no longer present.

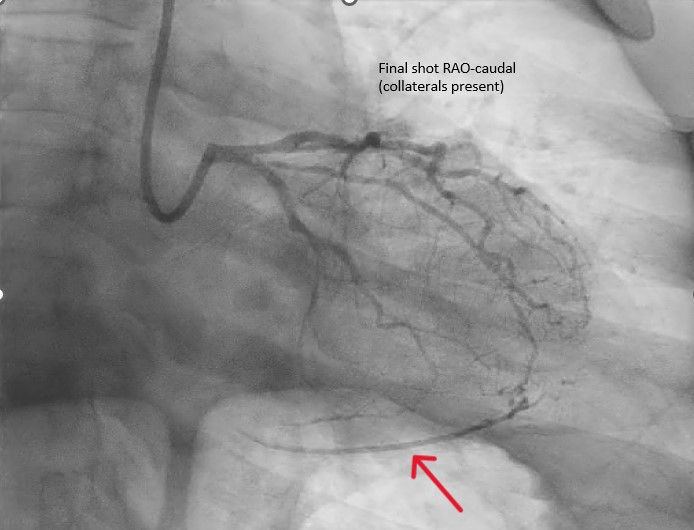

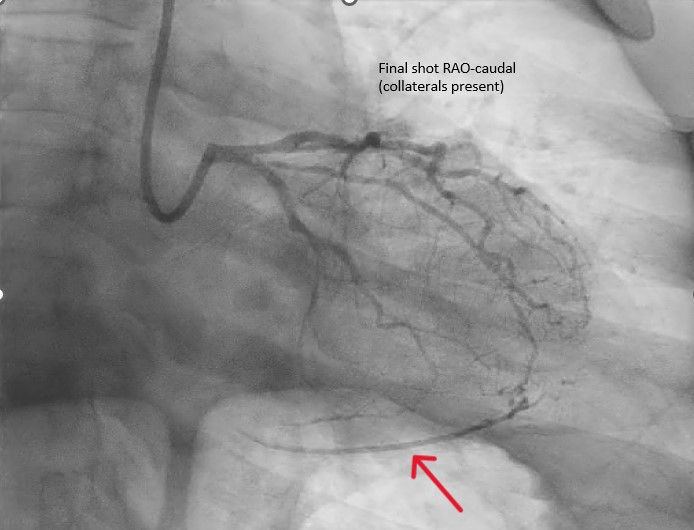
Case Summary
The interesting feature of this case is the refractoriness of the spasm to medical therapy with vasodilators. The second interesting feature is the rare hallmark of transient collateral augmentation that served to salvage otherwise jeopardized ischaemic areas (hence the unexpected saviour in this case). Decision to bail out and stent the spastic vessel, especially in patients who are refractory to medical management and who remain unstable is not an uncommon practice. In this case despite the spasm being refractory, a step back was taken (which was indeed a difficult decision to make). This was mainly because chest pain resolved, hemodynamics were stable, and collaterals were seen.

