Lots of interesting abstracts and cases were submitted for TCTAP 2024. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-152
Nine Decades Challenge : A Case of Very Old Age, Triple Vessel Disease, Diabetes, Chronic Kidney Disease and Acute Coronary Syndrome Status Post Complete Revascularization by IVUS and FFR Guidance.
By Wei-Cheng Chang, Yen-Lien Chou
Presenter
Wei-Cheng Chang
Authors
Wei-Cheng Chang1, Yen-Lien Chou2
Affiliation
Tri-Service General Hospital, Songshan Branch, Taiwan1, Tri-Service General Hospital, Taiwan2,
View Study Report
TCTAP C-152
Coronary - High-Risk Intervention (Diabetes, Heart Failure, Renal Failure, Shock, etc)
Nine Decades Challenge : A Case of Very Old Age, Triple Vessel Disease, Diabetes, Chronic Kidney Disease and Acute Coronary Syndrome Status Post Complete Revascularization by IVUS and FFR Guidance.
Wei-Cheng Chang1, Yen-Lien Chou2
Tri-Service General Hospital, Songshan Branch, Taiwan1, Tri-Service General Hospital, Taiwan2,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
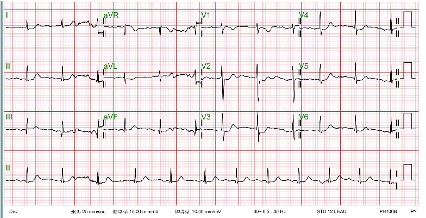
A 94-year-old man with a history of type 2 diabetes, stage III chronic kidney disease, hypertension, and hyperlipidemia presented to the emergency department with worsening chest pain and tightness that had persisted for several minutes. The electrocardiogram (ECG) revealed ST-segment depression in leads V2-V4(no elevated at V7-V9),, and elevated cardiac enzymes were noted. The catheterization (CATH) lab was promptly activated for non-ST-segment elevation myocardial infarction (NSTEMI)


Relevant Test Results Prior to Catheterization
Hemoglobin: 14.5 g/dL
Relevant Catheterization Findings
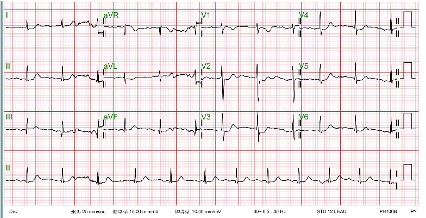
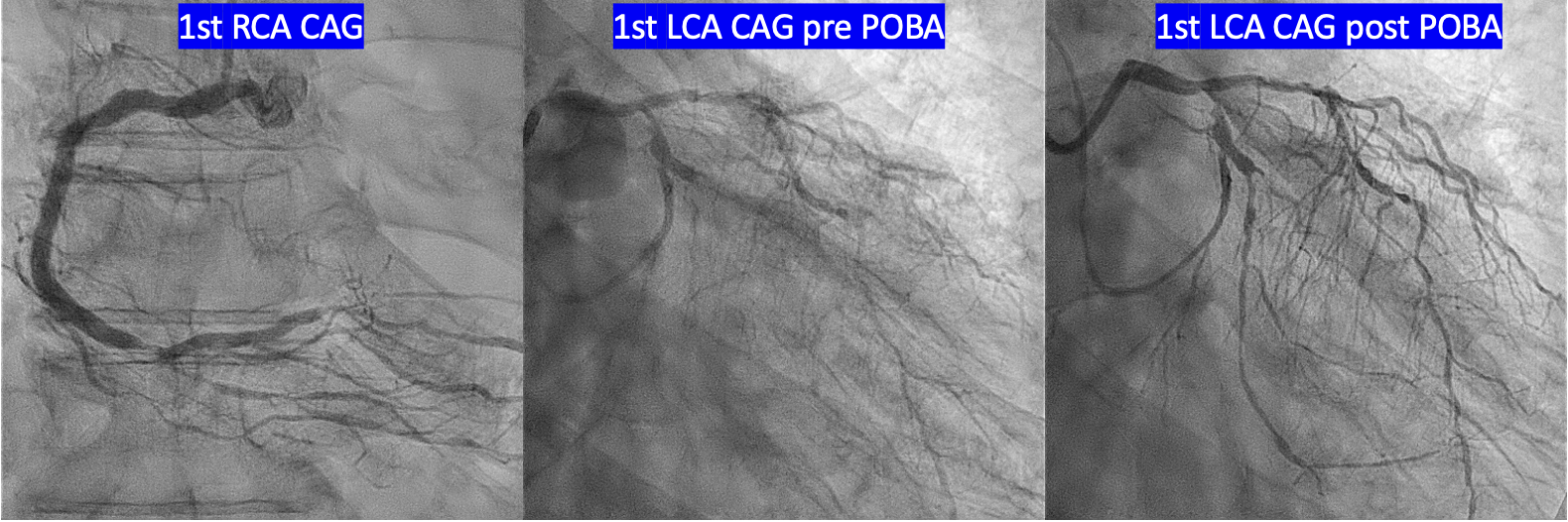
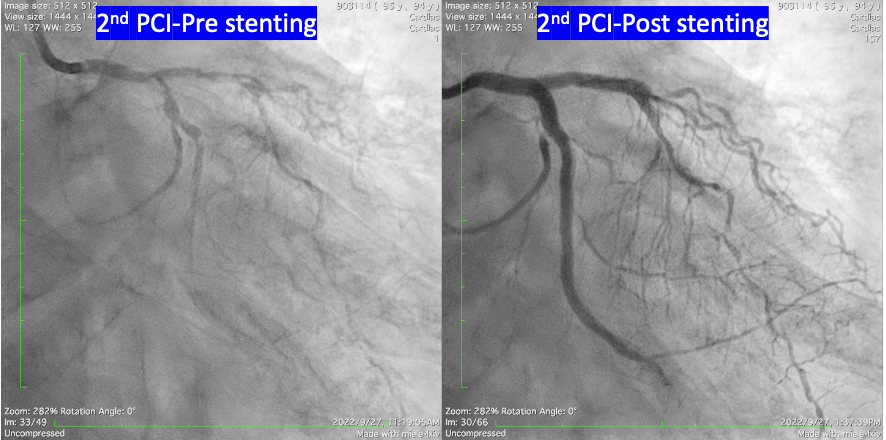
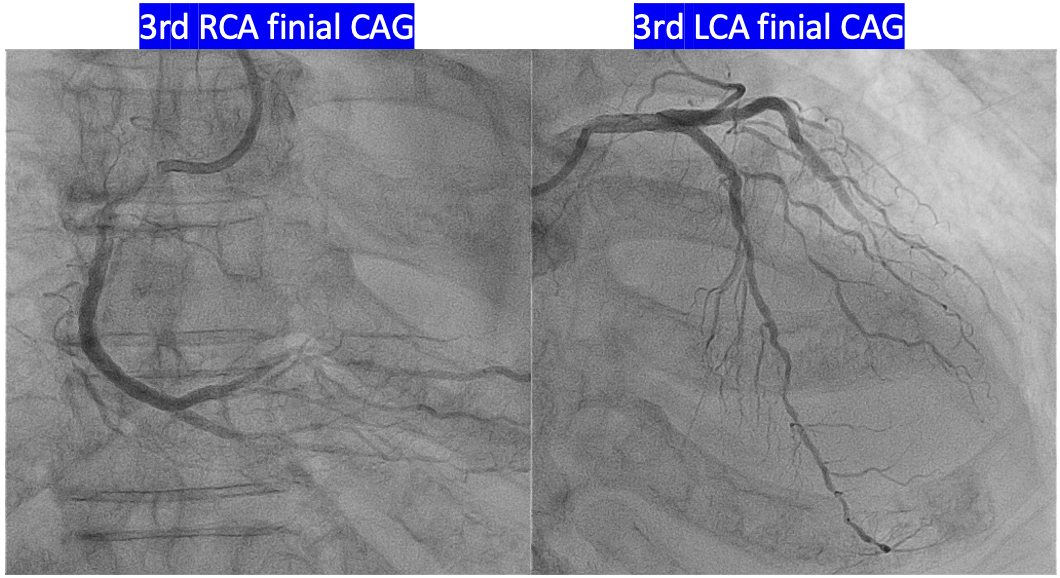
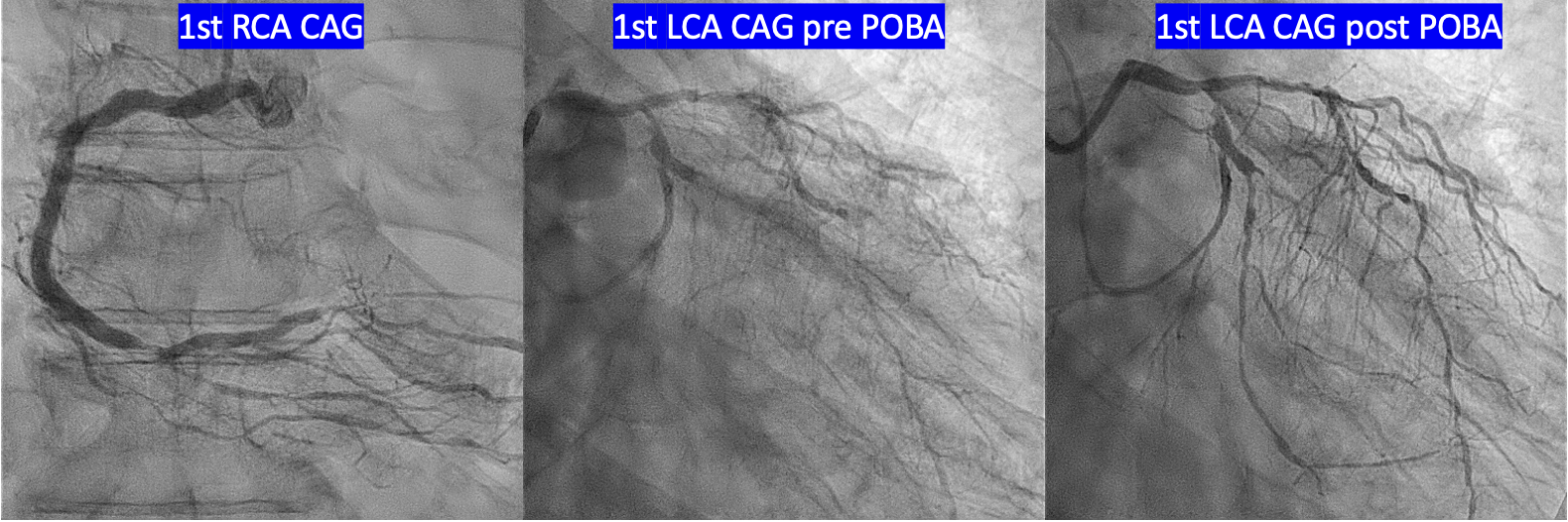
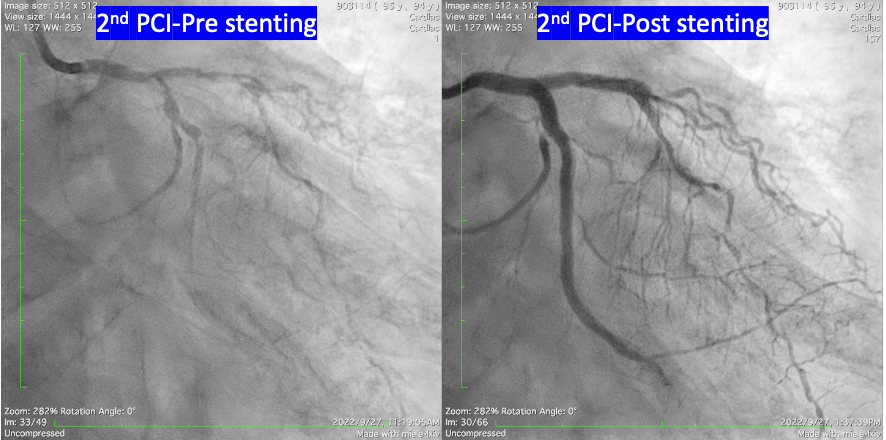
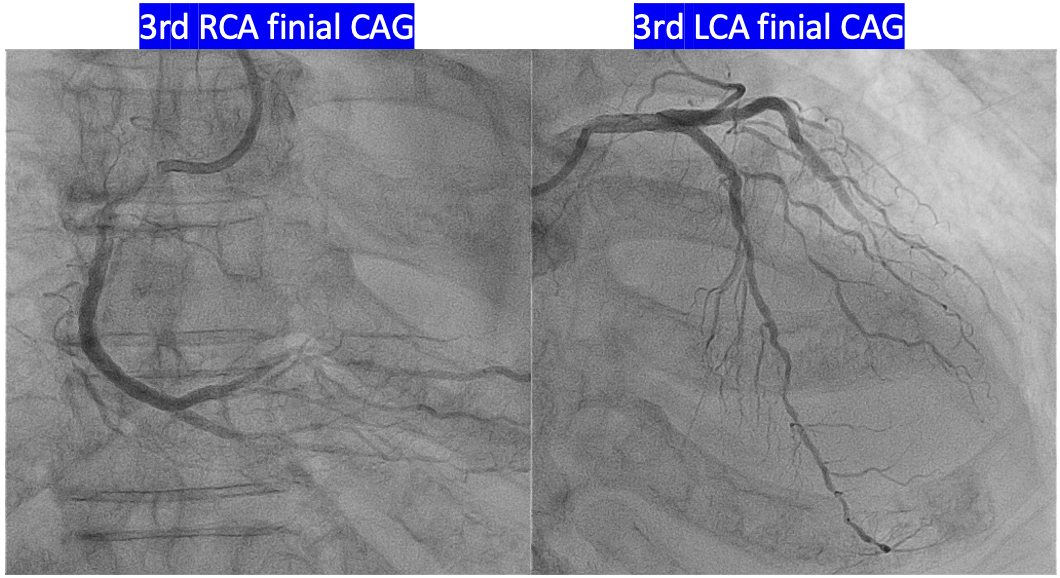
1.LMCA: patent2.LAD: -P/3 to D/3: diffuse lesion, max 80-90% stenosis -DB osmium: discrete lesion, max 70% stenosis DB M/3: diffuse lesion, max 80-90% stenosis3.LCX - Osmium: 80% stenosis - P/3:near total occlusion, receiving collateral flow form LAD4.RCA - D/3: tubular lesion, max 80-90% stenosis before bifurcation - PDA osmium-M/3: diffuse lesion, max 80-90% stenosis - PL: diffuse lesion, max 80% stenosis
Interventional Management
Procedural Step
Staged PCI was performed for complete revascularization.
Case Summary
This patient was of advanced age and had multiple chronic diseases, but he could still take care of himself. Coronary artery bypass grafting (CABG) was not considered due to his old age. Therefore, we performed a complicated complete triple-vessel revascularization with adequate sizing using intravascular ultrasound (IVUS) and checked the final result with fractional flow reserve (FFR). Due to his chronic kidney disease (CKD) and old age, the entire procedure was separated into three stages to reduce the contrast amount and procedure time at each percutaneous coronary intervention (PCI). After the intervention, he remained stable at the age of 95

