Lots of interesting abstracts and cases were submitted for TCTAP 2024. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-079
A Case of Triple Vessel Disease (Distal LMT, Ostial LAD CTO, Proximal RCA and LCX Stenosis) With Poor Left Ventricular Function Deemed Unfit for CABG Underwent Full Revascularization by Complex PCI
By Hou Tee Lu, Azrina Abdul Kadir, Heng Shee Kim, Chu Zhen Quek, Yu Ying Ong, Vicknesan Kulasingham, Mahadevan Gurudevan
Presenter
Hou Tee Lu
Authors
Hou Tee Lu1, Azrina Abdul Kadir2, Heng Shee Kim1, Chu Zhen Quek1, Yu Ying Ong3, Vicknesan Kulasingham4, Mahadevan Gurudevan5
Affiliation
Sultanah Aminah Hospital, Malaysia1, KPJ Bandar Dato Onn Specialist Hospital, Malaysia2, Sultan Idris Shah Serdang Hospital, Malaysia3, Ministry of Health Malaysia, Malaysia4, Sultanah Amina Hospital, Malaysia5,
View Study Report
TCTAP C-079
Coronary - Complex PCI - CTO
A Case of Triple Vessel Disease (Distal LMT, Ostial LAD CTO, Proximal RCA and LCX Stenosis) With Poor Left Ventricular Function Deemed Unfit for CABG Underwent Full Revascularization by Complex PCI
Hou Tee Lu1, Azrina Abdul Kadir2, Heng Shee Kim1, Chu Zhen Quek1, Yu Ying Ong3, Vicknesan Kulasingham4, Mahadevan Gurudevan5
Sultanah Aminah Hospital, Malaysia1, KPJ Bandar Dato Onn Specialist Hospital, Malaysia2, Sultan Idris Shah Serdang Hospital, Malaysia3, Ministry of Health Malaysia, Malaysia4, Sultanah Amina Hospital, Malaysia5,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
A 54-year-old male was admitted to a district hospital for shortness of breath and angina. He was then referred to our hospital for ACS and heart failure. His risk factors were DM and ex- smoker. The HR was 80/min and BP was 120/70 mmHg. He was on SC insulin (Actrapid) 10u tds, metformin 1 g BD, gliclazide 60 mg bd, aspirin 100 mg od, clopidogrel 75 mg od, Vasteral MR 35 mg bd, isorsobide mononitrate 60 mg ½ tab od, perindopril 2 mg od, bisoprolol 2.5 mgod, and atorvastatin 40 mg od.


Relevant Test Results Prior to Catheterization
The ECG showed T inversion at lead I, AVL, V6. The Troponin T was negative. Blood investigations: Hb: 14.4 g/dL, creatinine: 104 µmol/L, total cholesterol: 4.4 mmol/L and LDL: 2.7 mmol/L, and RBS 15.2 mmol/l. CXR showed cardiomegaly with minimal pleural effusion. The echocardiography showed impaired LVEF of 35-40% with dilated left ventricle. Hypokinetic anteroseptal wall. Normal valves.


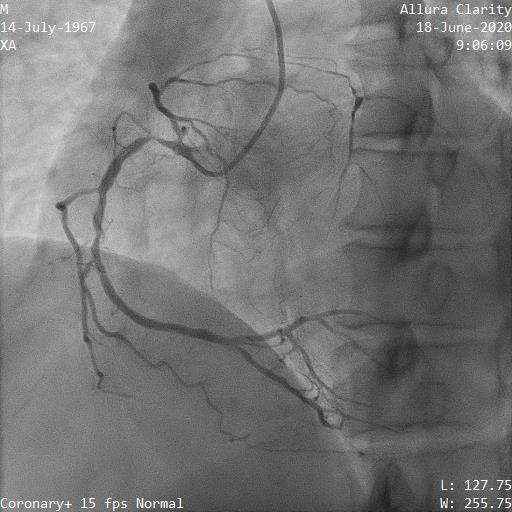
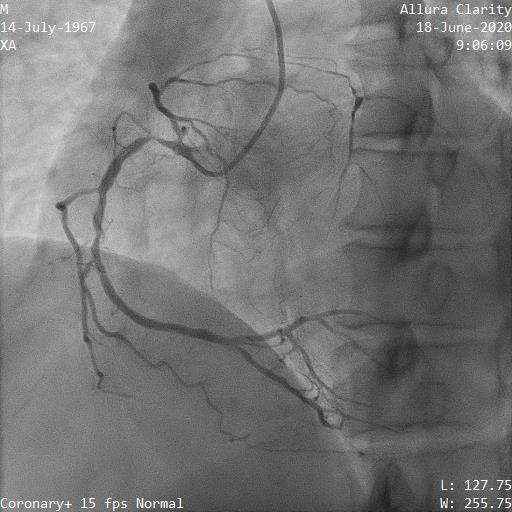
Relevant Catheterization Findings
Diagnostic angiogram1. Distal LMT 80% stenosis2. Ostial LAD CTO with ambiguous proximal cap 3. Proximal LCX artery 70% stenosis 4. Proximal RCA 90% stenosis, small septal collateral (CC) from PDA and epicardial CC from right marginal arterySYNTAX I score: 39 Nuclear scan showed viable myocardium in all territory.Patient was referred for CABG. However, he was deemed unfit for CABG because of poor LV function and angiographically small LAD. He was scheduled for high risk complex PCI.




Interventional Management
Procedural Step
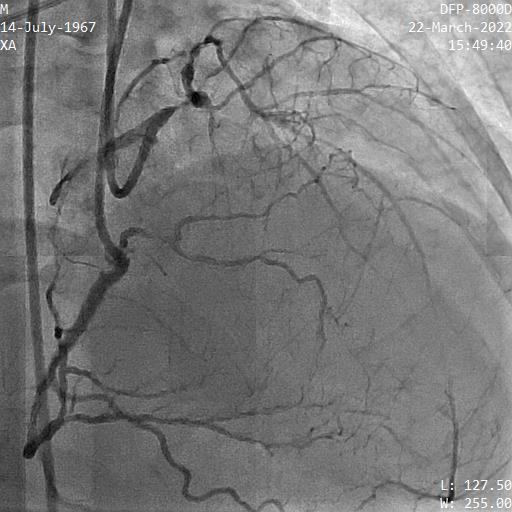
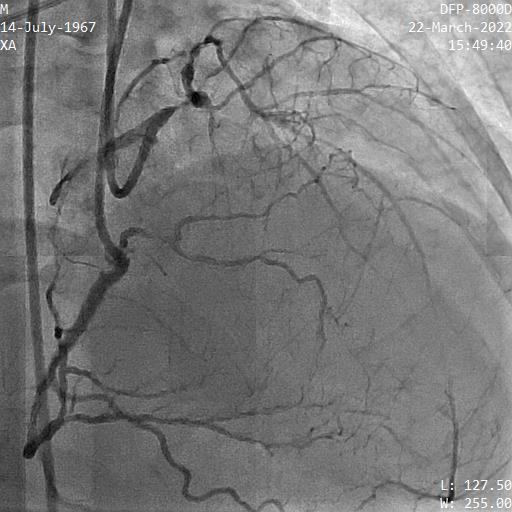
First, the proximal RCA (non-left main) lesion was treated successfully with a 3.5x23mm everolimus eluting stent (EES) . Stage PCI for LMT/LAD/LCX lesion was planned 1 month later. Unfortunately, during the procedure he developed acute pulmonary edema on table and the the procedure was abandoned. He was rescheduled for stage PCI after optimization of heart failure 2 month later. Bi-femoral punctured and IABP was used this time. A 7Fr EBU 3.5 GC was used to engage LMT. JR 4 GC was used for RCA. Initially, the antegrade approach to puncture LAD CTO proximal cap by Fielder XTR and GAIA 2nd via a Finecross microcatheter (MC) was unsuccessful. Then, parallel wire technique was applied with a CRUSADE MC but the second wire (Conquest Pro) went into false lumen. Decision was made for retrograde approach. After failing septal wiring, a SUOH 03 was successfully wired through the right marginal epicardial collateral into distal LAD via a Caravel MC. Wire was exchanged with a UB3 to penetrate distal CTO cap and UB3 was used as wire marker to guide antegrade puncture. The antegrade Conquest Pro was successfully entered LAD true lumen. The LMT/LAD/LCX bifurcation lesion was treated by MINI CRUSH technique guided by IVUS. The mid LAD was treated by a 2.25x24mm EES. The LCX was treated by a 4.0x16mm EES and the LM-LAD was treated by a 4.0x24mm EES. Final kissing balloon was performed. Patient discharged well. 8 month later, surveillance angiogram showed patent stents. The LV function was normalized.




Case Summary
Our case demonstrated that complex PCI could be considered as an alternative treatment for multivessel coronary artery disease with poor LV function deemed unfit for CABG. Stumpless CTO is challenging due to the difficulty of locating a suitable entry point. Retrograde wire marker technique is chosen in our case instead of the classic externalization wire technique to minimize the risk of epicardial collateral injury. In accordance with the clinical studies, the impaired LV function recovered after full revascularization.

