Lots of interesting abstracts and cases were submitted for TCTAP 2024. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-113
The Story of My Unfriendly Catheter
By Donluck Poonkasem, Mann Chandavimol, Pavit Pienvichit
Presenter
Donluck Poonkasem
Authors
Donluck Poonkasem1, Mann Chandavimol2, Pavit Pienvichit2
Affiliation
Vibharam Hospital, Thailand1, Ramathibodi Hospital, Thailand2,
View Study Report
TCTAP C-113
Coronary - Complication Management
The Story of My Unfriendly Catheter
Donluck Poonkasem1, Mann Chandavimol2, Pavit Pienvichit2
Vibharam Hospital, Thailand1, Ramathibodi Hospital, Thailand2,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
A 79 year-old-man with underlying diseases of hypertension, hyperlipidemia and dementia presented with dyspnea on exertion and intermittent chest tightness for 2 monthsAfter thorough physical examination, his lung was clear and his heart had no murmur.
Relevant Test Results Prior to Catheterization
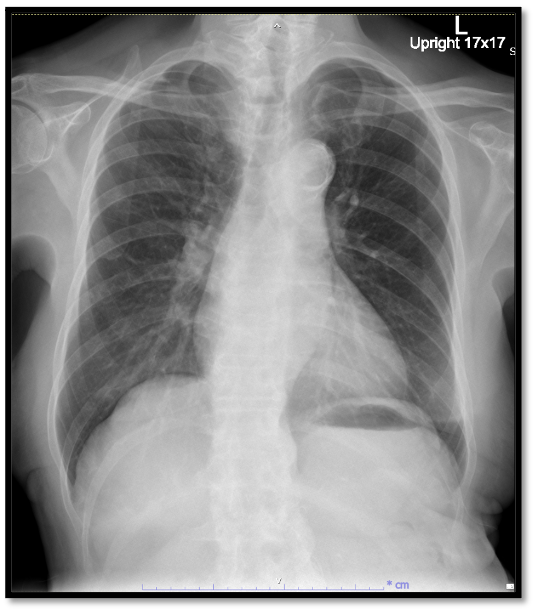
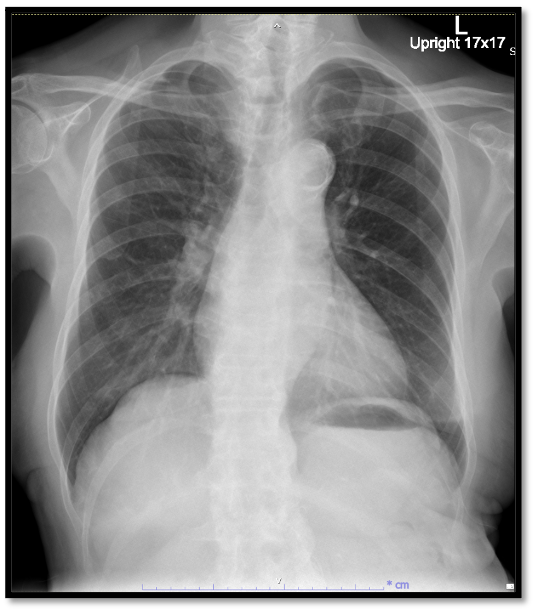
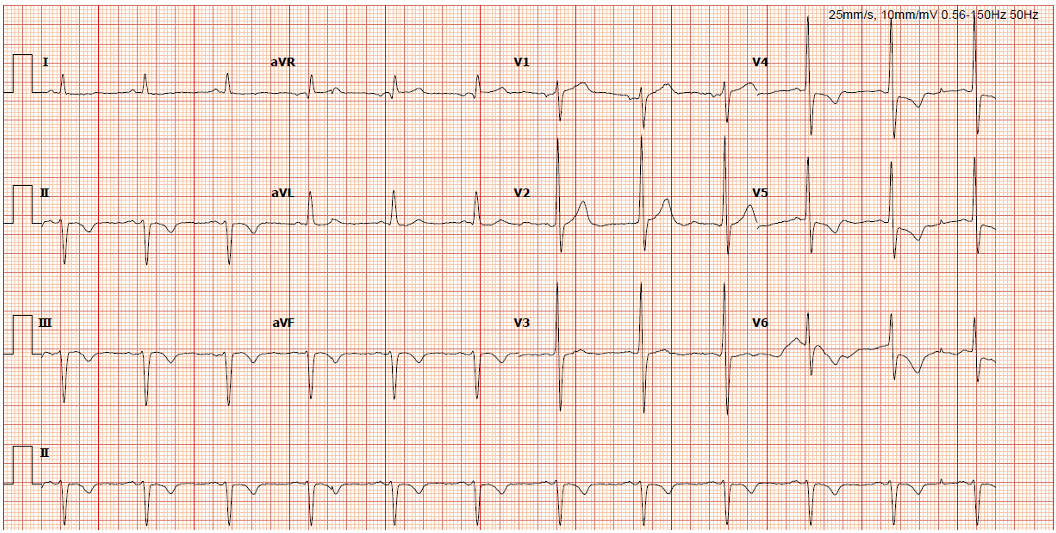
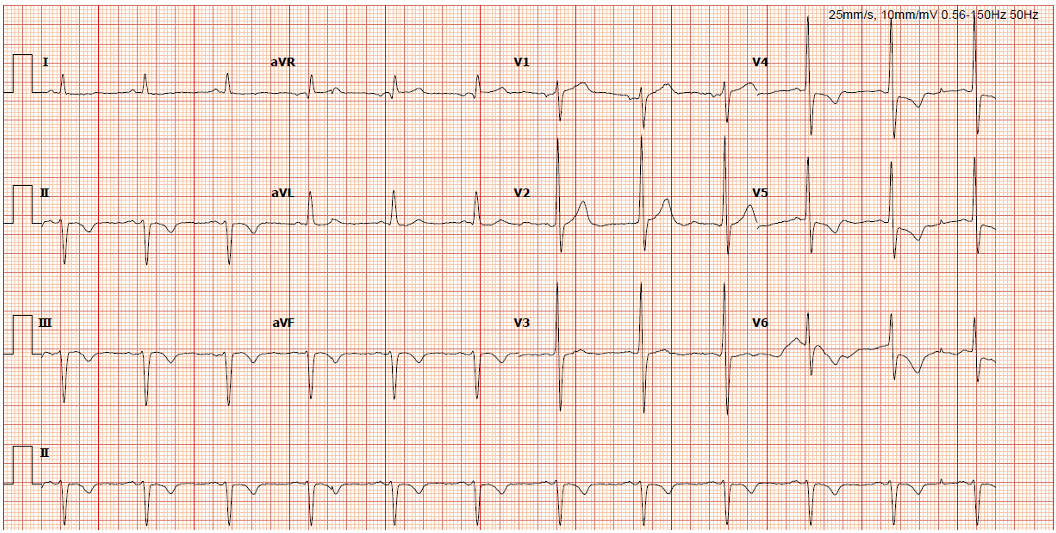
His chest x-rays showed cardiomegaly with normal lung parenchyma. His ECG showed sinus rhythm with T-wave inversion in lead II, III, aVF and ST depression in lead V4-6.Other blood examination tests were in normal range.Cardiac MRI exhibited that LVEF was impaired with 40% and there were severe hypokinesia of anterior, anteroseptal, inferosetal, and inferior wall from apical to basal segment. Besides, there was no late gadolinium enhancement which meant all segments were viable.
Relevant Catheterization Findings
CAG was done and shown as below.LM : No significant stenosis


LAD : 80-90% calcified stenosis at proximal to mid LAD with bifurcation of 70% stenosis ostial DG1
LCx : 90% calcified stenosis at proximal part followed by 90% long stenosis distal part.
RCA : Nodular calcium causing 90% stenosis ostial RCA followed by CTO distal PLB received collateral flow from left coronary system
In conclusion, the patient had tripple vessel disease and desired to be revascularised with PCI rather than CABG.


Interventional Management
Procedural Step
We planed to do PCI to RCA first with JR4 guiding and SION blue as workhorse wire. Pre-dilation was done with SC balloon 2.5 x 15 mm and NC balloon 3.5 x 15 mm respectively at proximal RCA. After that we tried to put the stent (SES 4.0 x 19 mm) into the lesion. Because of lack of support from guiding catheter and tight calcified lesion, the calamity was happened. The guiding catheter was push back and also dragged out the stent and wire to the aorta. We tried to engage again with the same catheter but serious accident occurred. Due to tortuous right femoral and iliac artery, the proximal part of catheter was twisted like a knot. And after we tried to pull it back, the knot was fastened tighter and unable to untangle.We change the strategy to solve this disaster. We accessed via transradial artery in order to use snare to fix the tip of catheter. But the anatomy to the right subclavian artery was quite challenging. We changed many catheters to facilitate the snare to grab tip of guiding catheter. Finally, we can catch it followed by untangled the twisted knot and pulled it out. Lastly, we proceeded to deploy stent by using new guiding catheter. The final angiogram showed satisified result.






Case Summary
A 79 year-old-man presented with chronic coronary syndrome and his angiogram showed TVD with calcified lesion. Firstly, we tried to do PCI at proximal RCA but accidentally, the catheter was twisted and kinked. We used the snare via transradial artery to grab the tip of catheter in order to fix it and be able to untangle the proximal part. Finally, we can finish the PCI of RCA with good results without further complications.

