Lots of interesting abstracts and cases were submitted for TCTAP 2024. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-143
A Culprit From the Past
By Steven Wong Poh Hock, Aslannif Roslan, Shaiful Azmi Yahaya
Presenter
Steven Wong Poh Hock
Authors
Steven Wong Poh Hock1, Aslannif Roslan1, Shaiful Azmi Yahaya1
Affiliation
National Heart Institute, Malaysia1,
View Study Report
TCTAP C-143
Coronary - DES/BRS/DCB
A Culprit From the Past
Steven Wong Poh Hock1, Aslannif Roslan1, Shaiful Azmi Yahaya1
National Heart Institute, Malaysia1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
65 years old lady with premorbid of hypertension, diabetes mellitus presented with shortness of breath, orthopnea and reduced effort tolerance progressively worsening over 3 days. On arrival her blood pressure was 93/63mmHg, heart rate 79bpm, SPO2 91% under room air. Lung auscultation revealed crepitations bilaterally up to midzones. Two weeks prior to this, she had DCB done to LAD at another hospital for late presentation of anterior myocardial infarction, and was discharged well.




Relevant Test Results Prior to Catheterization
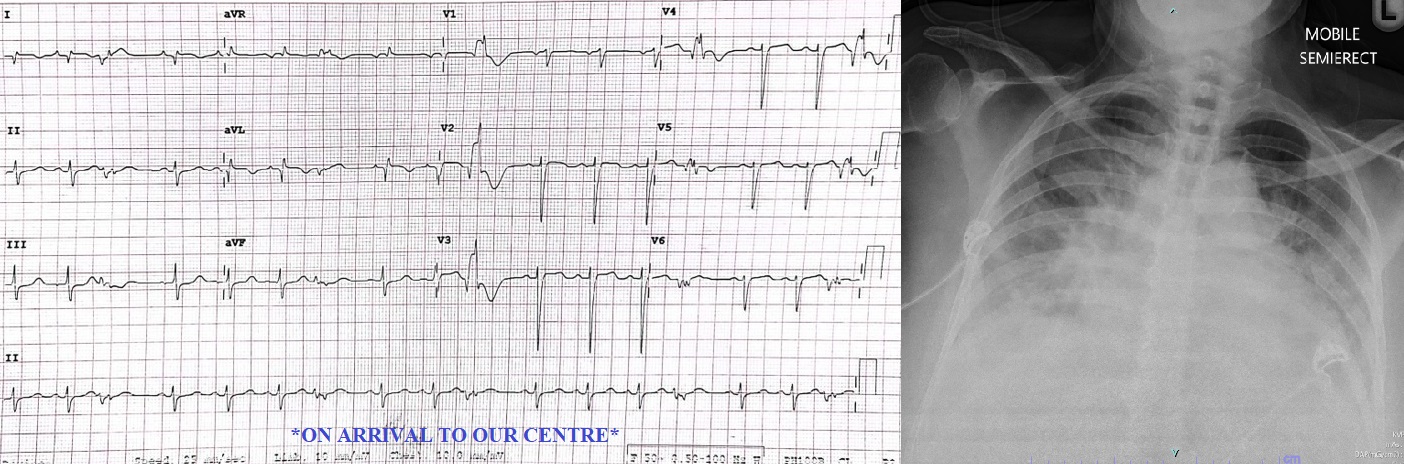
ECG revealed poor R wave progression, and multiple PVCs (isolated, couplet, NSVT). Chest X-ray is consistent with acute pulmonary edema.
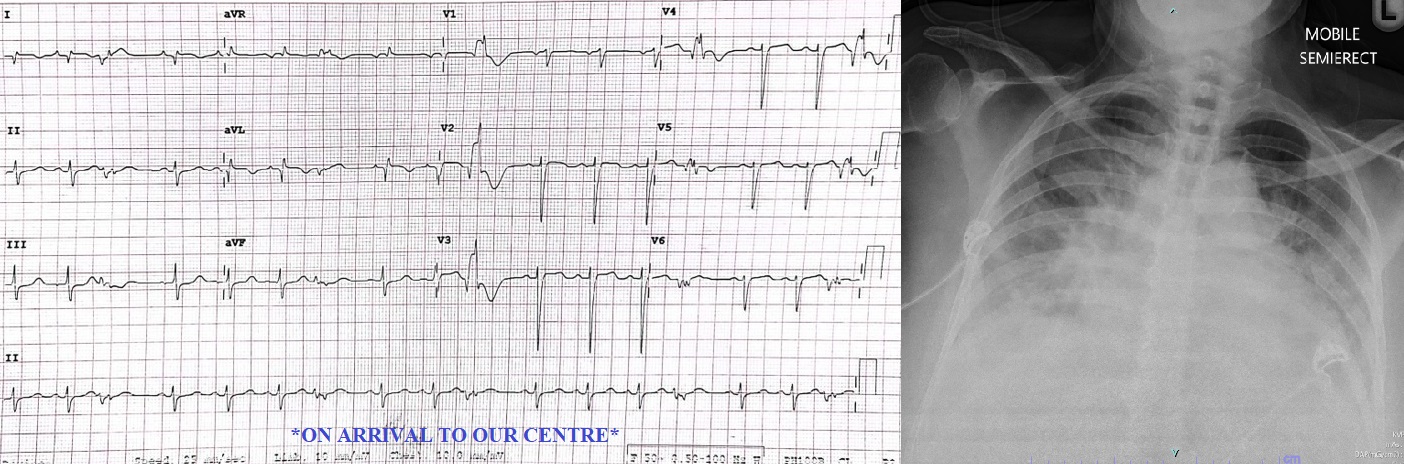
Echocardiogram: EF 20%, moderate MR, global hypokinesia. Pericardial effusion largest 1cm at lateral wall, no tamponade. No VSR.She was ventilated in CCU and we brought her into the cath lab the next day due to episodes of Ventricular tachycardia and fibrillation which required multiple shocks.

Relevant Catheterization Findings
Left main stem : Normal




Interventional Management
Procedural Step
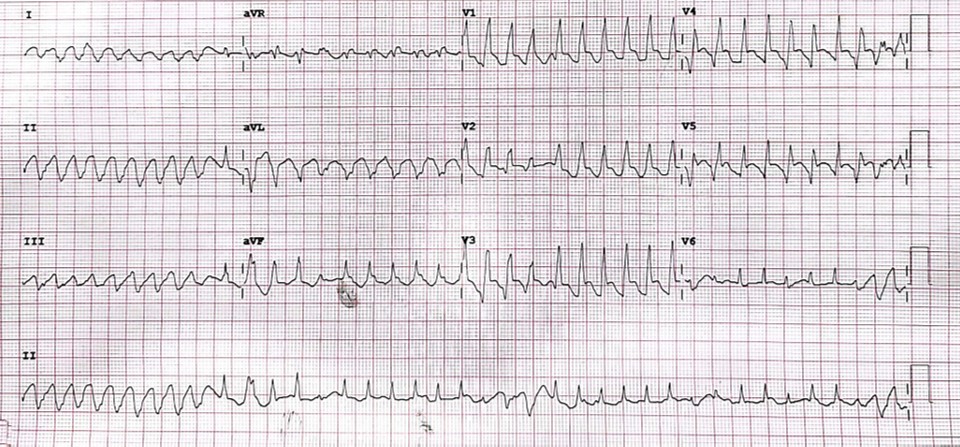
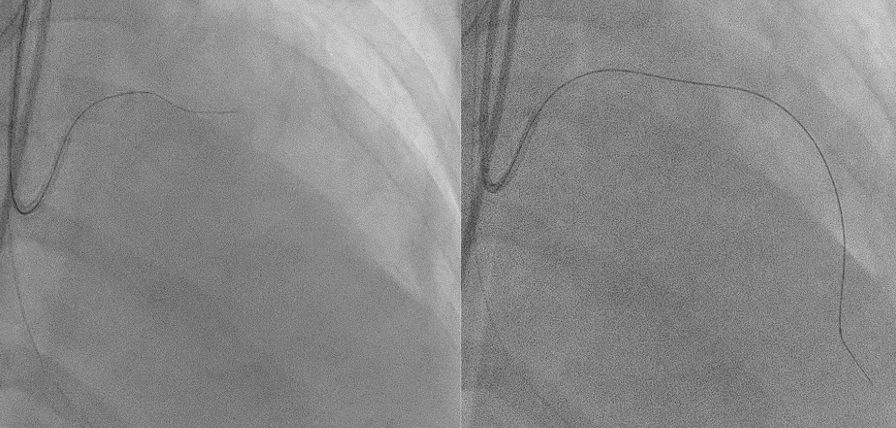
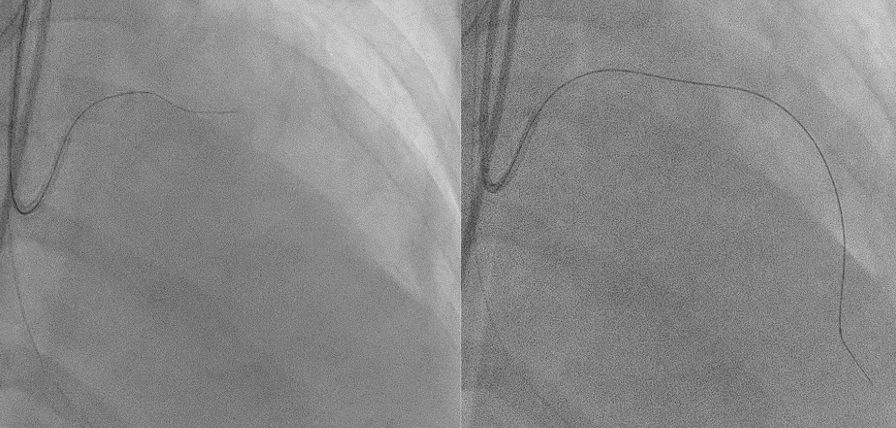
IABP insertion was done via left femoral approach. The right femoral artery was punctured, and left coronary artery was engaged with EBU 3.5 6FR catheter.
We had difficulty wiring through LAD, and we eventually able to wire across the occlusion with Fielder XT wire supported by Finecross microcatheter.
It was exchanged to Runthrough floppy, and SION blue was placed in LCX.
Predilation was done with RYUREI 2.0x15mm and 2.5x15mm from mid to ostio-proximal LAD. Stented Ostial-proximal LAD with SYNERGY 2.75x38mm and postdilated with SAPPHIRE NC 2.75x15mm.
Noted distal stent edge dissection which was stented. TIMI III flow achieved and no recurrence of ventricular arrhythmia noted.

We had difficulty wiring through LAD, and we eventually able to wire across the occlusion with Fielder XT wire supported by Finecross microcatheter.
It was exchanged to Runthrough floppy, and SION blue was placed in LCX.
Predilation was done with RYUREI 2.0x15mm and 2.5x15mm from mid to ostio-proximal LAD. Stented Ostial-proximal LAD with SYNERGY 2.75x38mm and postdilated with SAPPHIRE NC 2.75x15mm.
Noted distal stent edge dissection which was stented. TIMI III flow achieved and no recurrence of ventricular arrhythmia noted.

Case Summary
Restenosis rates in ostial LAD lesions treated with DCB/DEB have been a subject of interest in interventional cardiology. Ostial lesions, due to technical challenges in stent positioning and vessel scaffolding, have been associated with a higher risk of restenosis. A study comparing ostial LAD stenting with a cross-over technique showed the feasibility of ostial stenting; however, a high restenosis rate was observed in this group. Therefore, further research and larger studies are warranted to explore strategies to effectively reduce restenosis in ostial LAD lesions.

