Lots of interesting abstracts and cases were submitted for TCTAP 2024. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-114
Unforseen Dissection
By Kim Fong Ng, Jian Hao Sim, Wee Pang Ng, Jin Kiang Cheng, Vicknesan Kulasingham, Gurudevan Mahadevan
Presenter
Kim Fong Ng
Authors
Kim Fong Ng1, Jian Hao Sim2, Wee Pang Ng2, Jin Kiang Cheng3, Vicknesan Kulasingham4, Gurudevan Mahadevan2
Affiliation
KPJ KLUANG SPECIALIST HOSPITAL, Malaysia1, Sultanah Aminah Hospital, Malaysia2, Hospital Sultanah Aminah, Malaysia3, Ministry of Health Malaysia, Malaysia4,
View Study Report
TCTAP C-114
Coronary - Complication Management
Unforseen Dissection
Kim Fong Ng1, Jian Hao Sim2, Wee Pang Ng2, Jin Kiang Cheng3, Vicknesan Kulasingham4, Gurudevan Mahadevan2
KPJ KLUANG SPECIALIST HOSPITAL, Malaysia1, Sultanah Aminah Hospital, Malaysia2, Hospital Sultanah Aminah, Malaysia3, Ministry of Health Malaysia, Malaysia4,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
A 65-year-old gentlemen, a former smoker with medical history including diabetes mellitus, hypertension and ischaemic heart disease underwent prior PCI for RCA and LCx in 2015. Recently, he experienced one episode of unstable angina. An angiogram conducted at a private centre revealed 70% stenosis in the LAD and 70% ISR in the RCA. He had been referred to our centre for further PCI intervention.
Relevant Test Results Prior to Catheterization
Echocardiogram showed good LV function , EF 65%, All chamber normal size. All valves normal and functional No RWMA. No diastolic dysfunction.




Relevant Catheterization Findings
PCI to LAD and RCA
IA Heparin 8000 IU given and T. Clopidogrel 300mg were given prior to PCI
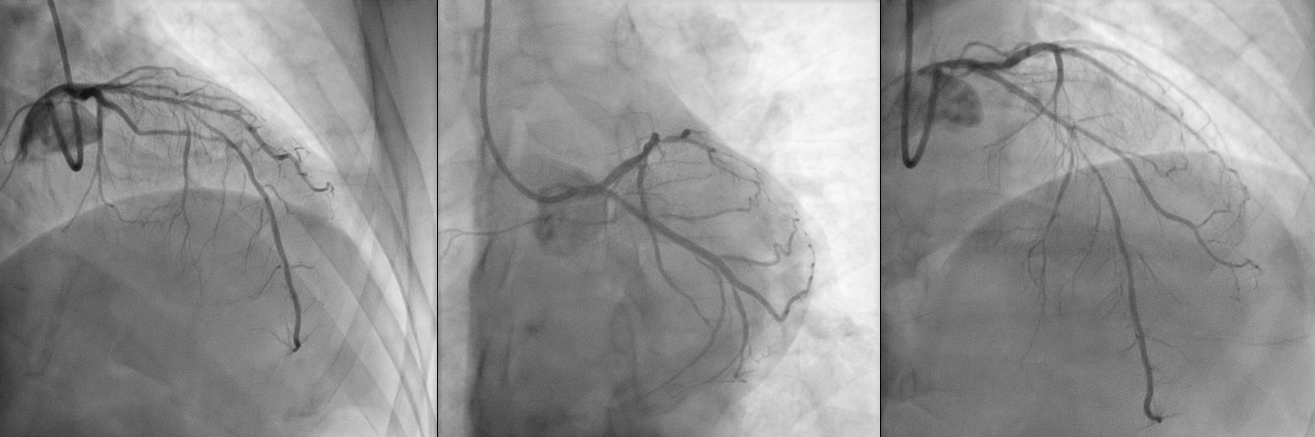
We wired down LAD with PT 2 moderate support. We then predilated MLAD with Emerge Monorail 2.5 x 15mm, up to 12 atm. We deployed DCB to MLAD with Agent 2.5 x 30mm, up to 6 atm, followed by DES to PLAD with Promus Elite 2.75 x 38mm. Post-dilatation of stent was done with NC Emerge 3.0 x 15mm, up to 16 atm. TIMI flow was III post-procedure.
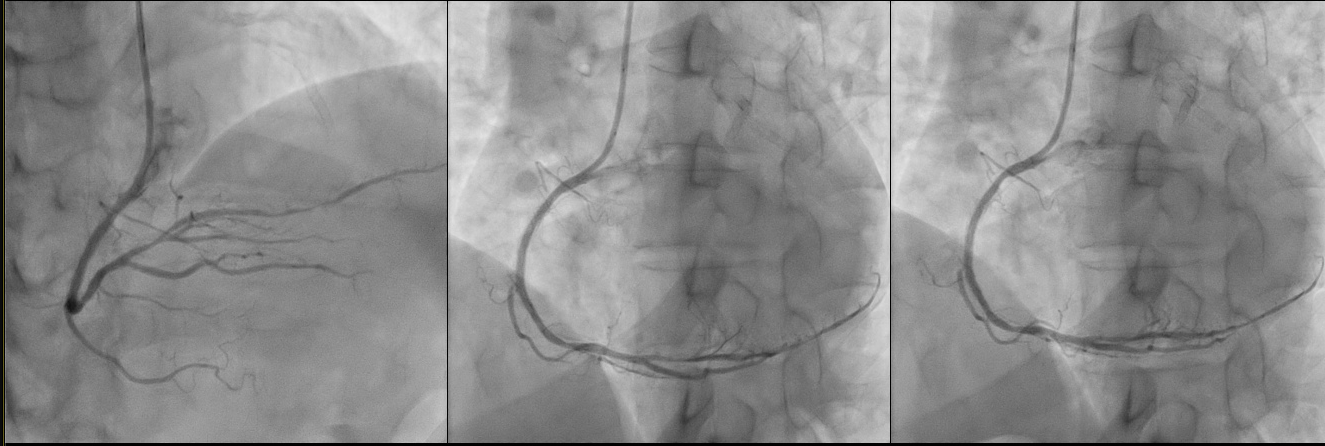
We proceed to engaged RCA with JR 4 6 F. Then we wired down RCA with PT 2 moderate support. We predilated PRCA to MRCA with NC Emerge 2.5 x 15mm, up to 20 atm. Further pre-dilatation of the PRCA to MRCA was performed with NC Emerge 3.0 x 15mm, up to 22 atm. We then deployed DCB to MRCA with Agent 3.0 x 30mm, up to 12 atm, and Agent 3.5 x 30mm, up to 8 atm. Another DCB was placed at the ostial RCA to PRCA with 3.5 x 20mm, up to 12 atm. Noted Type A dissection at the end of the procedure. However, it was non-flow limiting and post-procedural TIMI Flow was III. Patient was asymptomatic. The case was ended.



IA Heparin 8000 IU given and T. Clopidogrel 300mg were given prior to PCI
We wired down LAD with PT 2 moderate support. We then predilated MLAD with Emerge Monorail 2.5 x 15mm, up to 12 atm. We deployed DCB to MLAD with Agent 2.5 x 30mm, up to 6 atm, followed by DES to PLAD with Promus Elite 2.75 x 38mm. Post-dilatation of stent was done with NC Emerge 3.0 x 15mm, up to 16 atm. TIMI flow was III post-procedure.
We proceed to engaged RCA with JR 4 6 F. Then we wired down RCA with PT 2 moderate support. We predilated PRCA to MRCA with NC Emerge 2.5 x 15mm, up to 20 atm. Further pre-dilatation of the PRCA to MRCA was performed with NC Emerge 3.0 x 15mm, up to 22 atm. We then deployed DCB to MRCA with Agent 3.0 x 30mm, up to 12 atm, and Agent 3.5 x 30mm, up to 8 atm. Another DCB was placed at the ostial RCA to PRCA with 3.5 x 20mm, up to 12 atm. Noted Type A dissection at the end of the procedure. However, it was non-flow limiting and post-procedural TIMI Flow was III. Patient was asymptomatic. The case was ended.



Interventional Management
Procedural Step
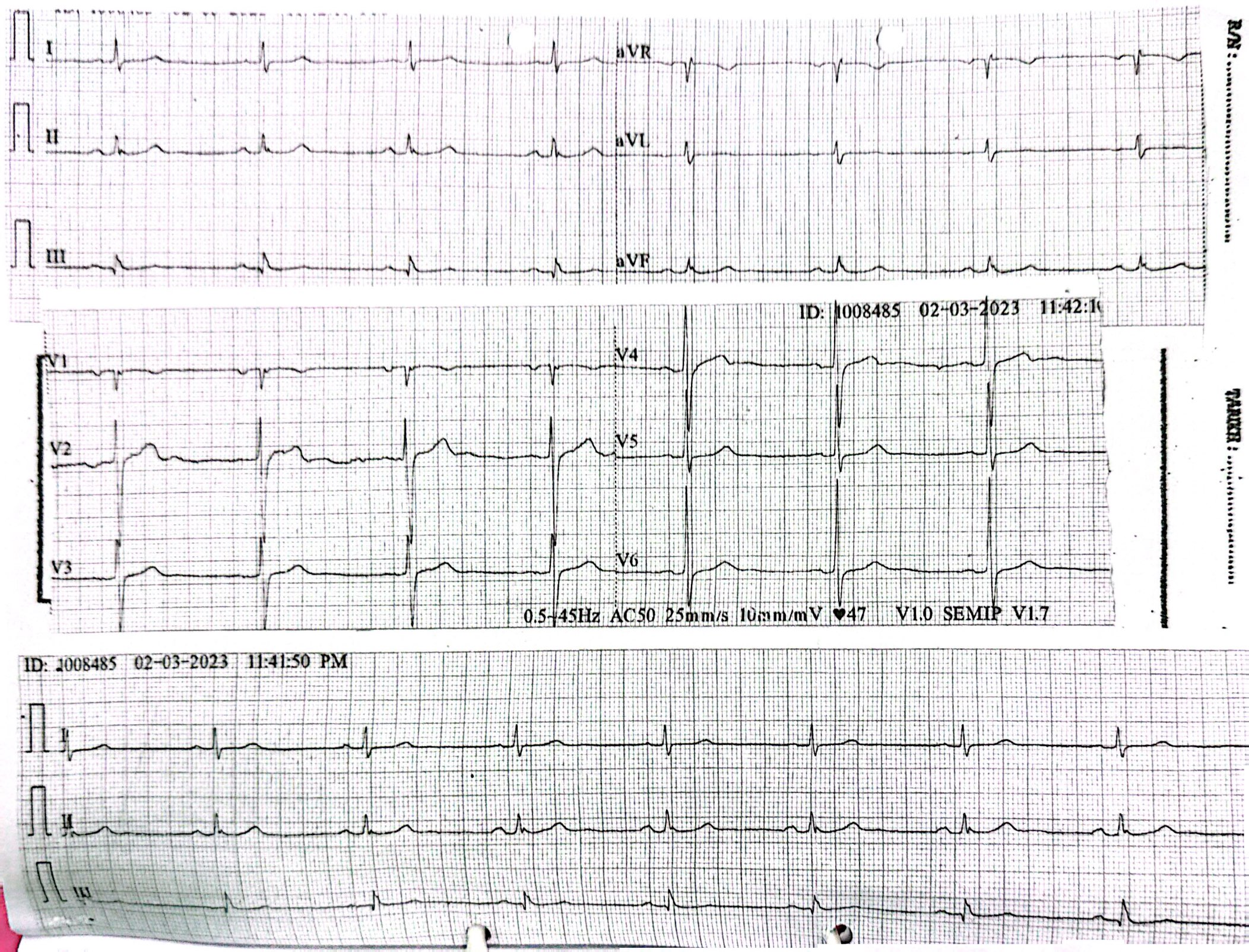
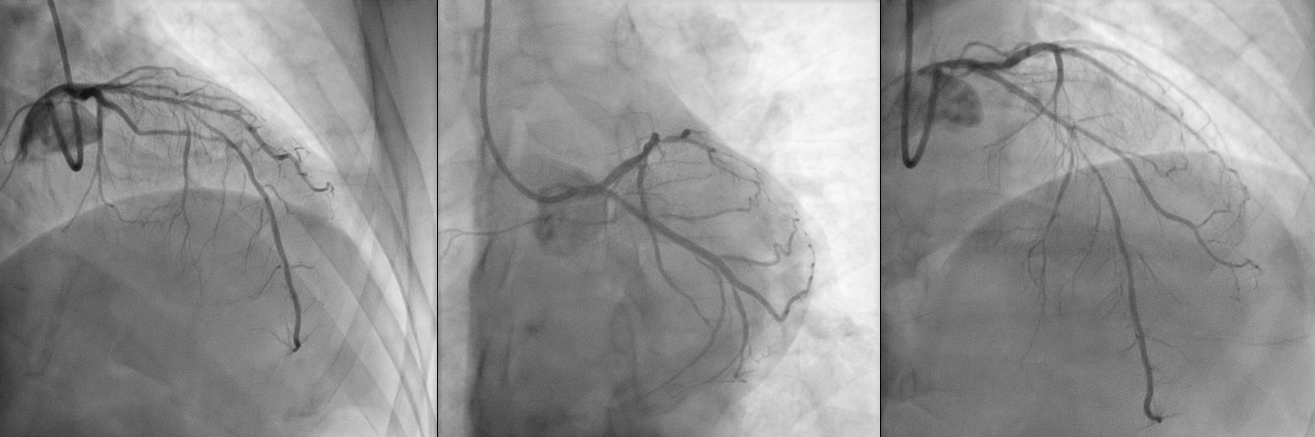
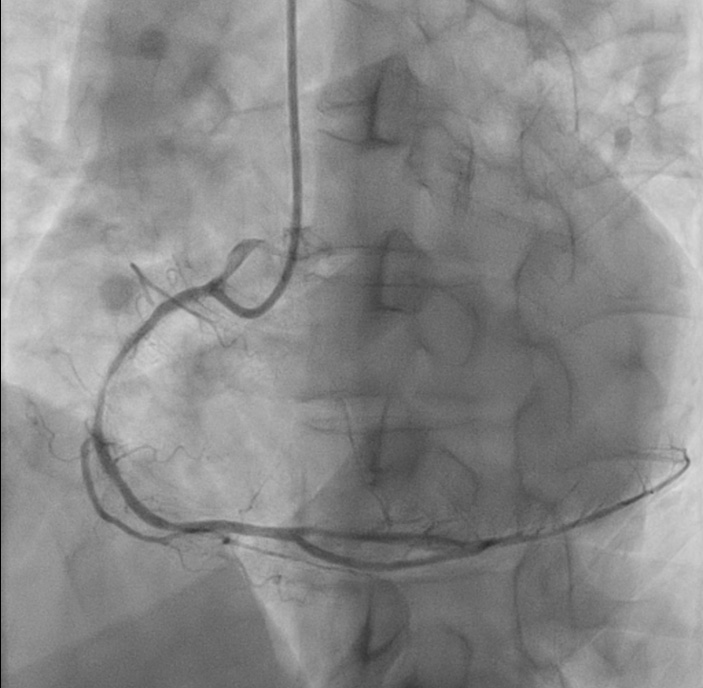
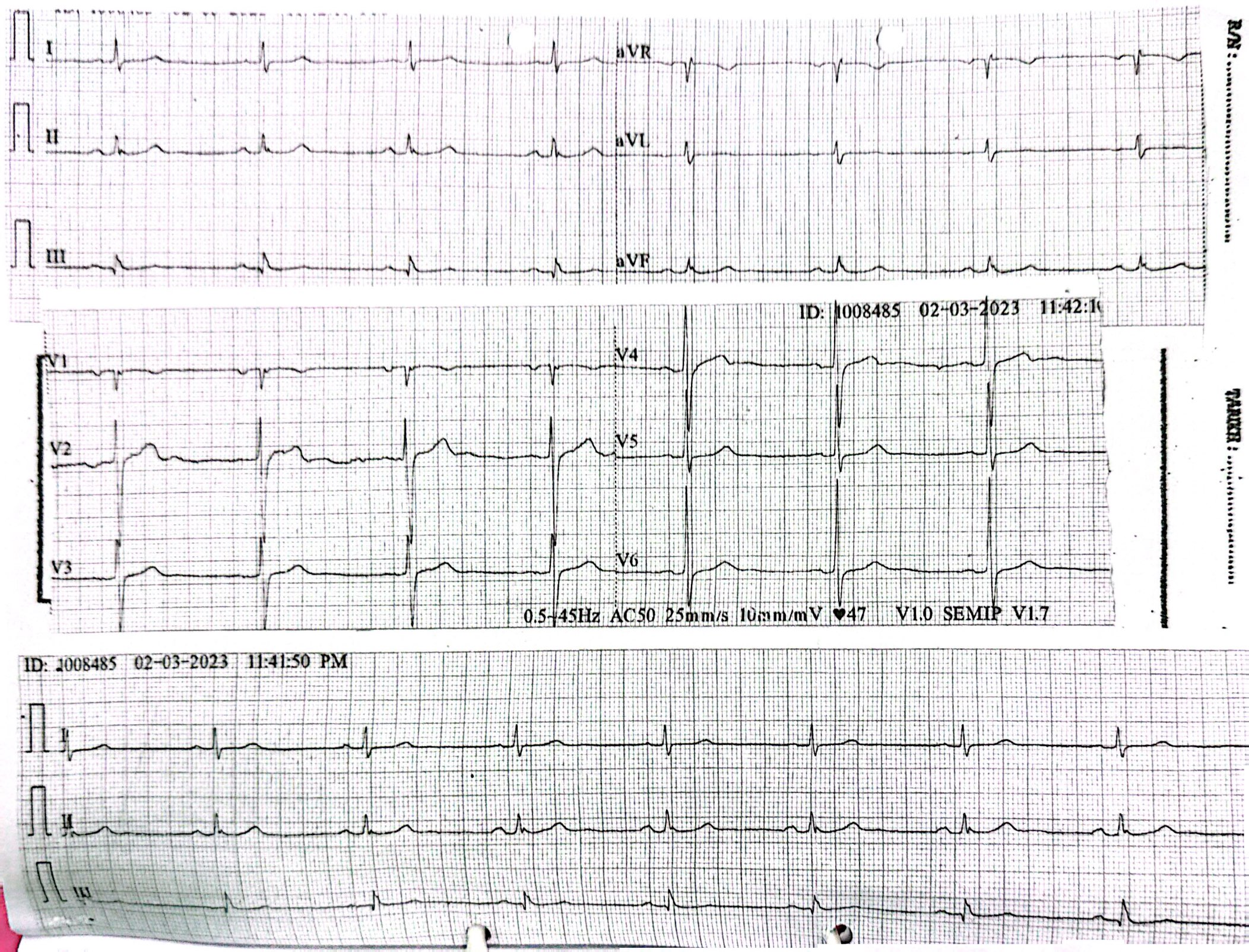
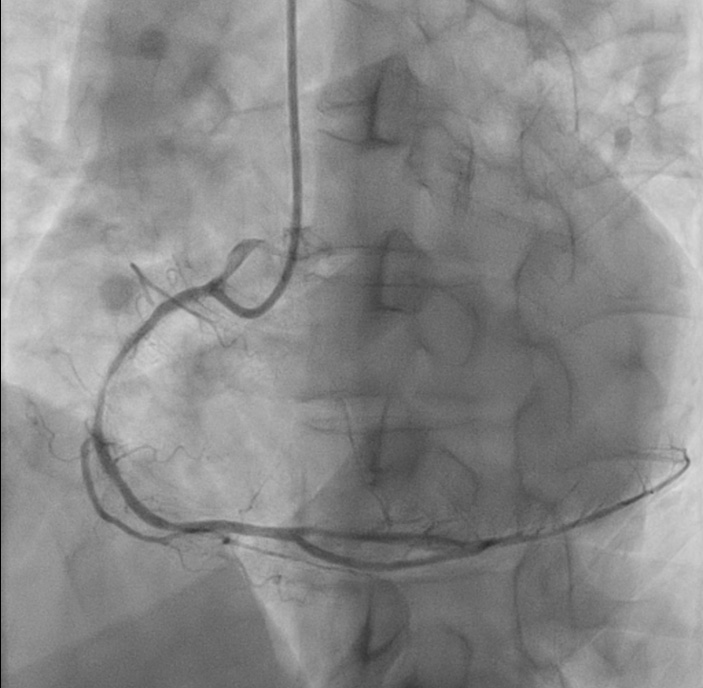
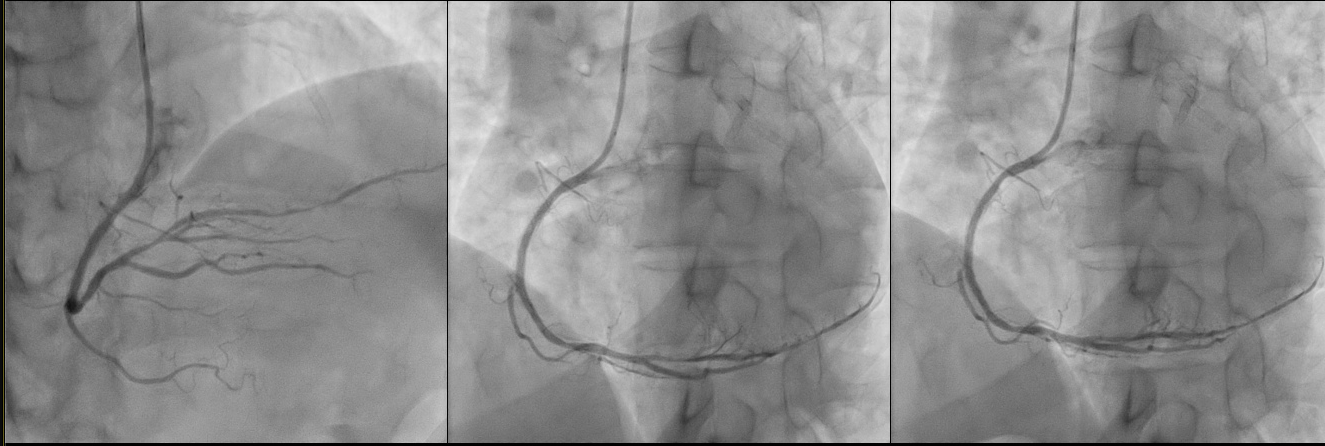
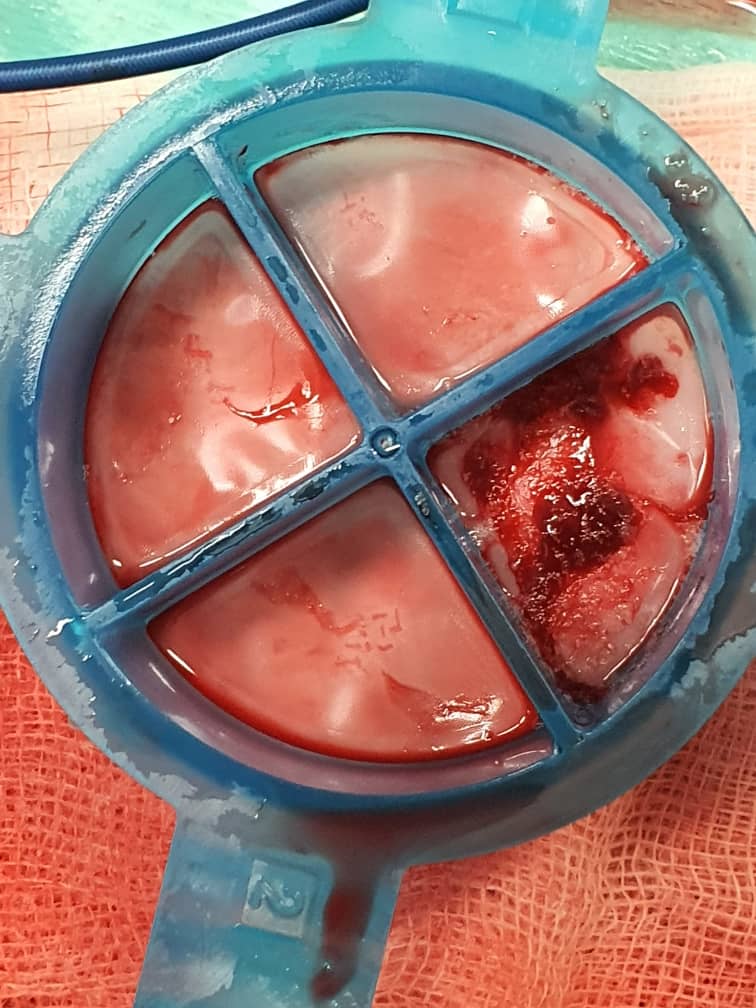
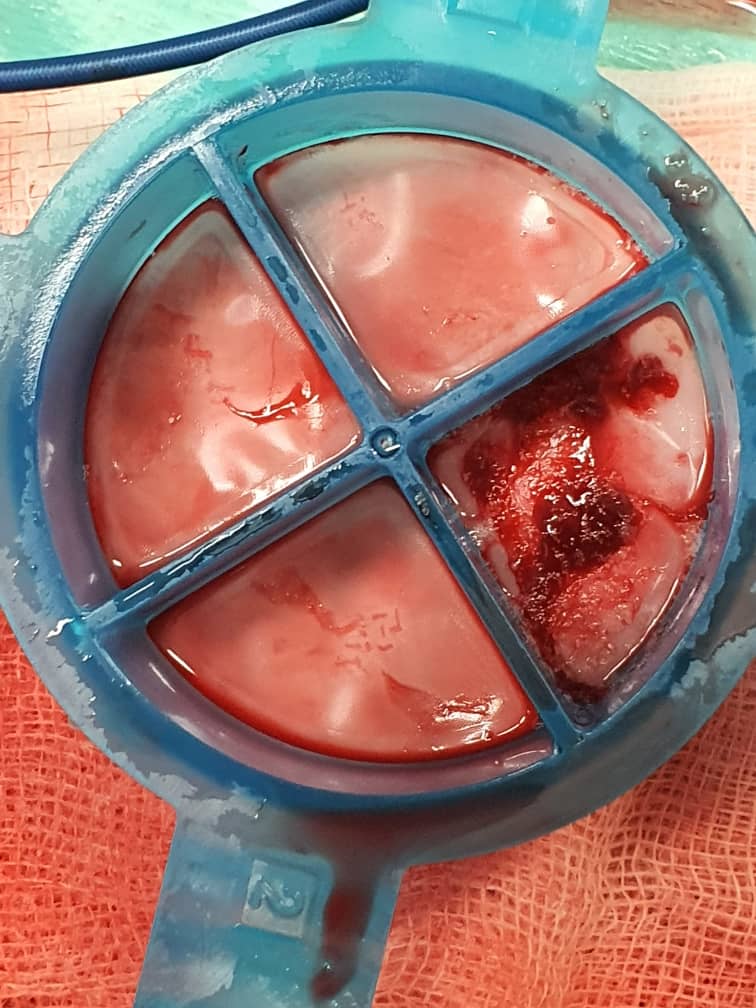
12 minutes after the procedure, while at the recovery bay, patient had syncopal attack. ECG at that time showed sinus rhythm. Patient complained of central chest pain, heavy in nature, 2 hours after the PCI. His chest pain was not relieved with Subligual GTN spray x 3. ECG showed ST elevation II, III, aVF, V7 – V9; ST depression V1 – V3. We immediately brought the patient back to the catheterization lab and performed coronary angiogram for him. Diagnostic coronary angiogram of the RCA showed dissection at ostial RCA at aortic cusp, 30% stenosis at PRCA, 40% stenosis at MRCA, acute total occlusion with multiple large thrombus. We proceed to engaged RCA with JR 4 6 F and wired down RCA with Asahi Sion Blue. Multiple large thrombi aspirated with thrombuster III SL. Patient was restless during the procedure. Direct stenting to the DRCA was done with Biomatrix Alpha 2.5 x 36mm. Post-dilatation of the stent was done with Accuforce 2.5 x 8mm, up to 20 atm. We then proceed with direct stenting of the ostial RCA to pRCA with Biomatrix Alpha 3.5 x 29mm and post-dilated it with NC Euphora 3.5 x 15mm, up to 22 atm. TIMI flow III achieved post-procedure. Final fluoroscopic image showed good result. Patient’s symptoms resolved. ECG post-procedure revealed sinus rhythm, with no acute ischemic changes.Patient subsequently underwent CT Coronary Artery & CT Thoracic Aorta the next day. The CT findings showed acute Stanford Type A thoracic aorta dissection. No haematoma or leakage; moderate RCA ISR. Underlying triple vessels disease with LAD and LCX stent in-situ. No demonstrable resting myocardial infarct. Upper abdomen cystic lesion with predominantly benign features, differential diagnosis of GIST with no evidence of distal metastasis.




Case Summary
IVUS should be use at the start to assess the PCI of RCA and dissection. For coronary ostial lesions, particularly those situated at either the aorto-ostial or major coronary ostial segments, the prevailing management strategy involves stent implantation to seal the flap in the ostial right coronary artery (RCA). This approach boasts the highest success rates. In cases where instability or confirmatory progression of dissection to the ascending aorta and beyond is observed through computed tomography aortography, coronary artery bypass grafting (CABG) and aortic repair are reserved for such high-risk patients.

