Lots of interesting abstracts and cases were submitted for TCTAP 2024. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-163
To Test Is to Believe: A Reverse Visual-Functional Mismatch Between IVUS and FFR
By Hsuan-Ling Tseng, Hsien-Li Kao
Presenter
Hsuan-Ling Tseng
Authors
Hsuan-Ling Tseng1, Hsien-Li Kao2
Affiliation
Chi-Mei Hospital, Taiwan1, National Taiwan University Hospital, Taiwan2,
View Study Report
TCTAP C-163
Coronary - Imaging & Physiology - FFR
To Test Is to Believe: A Reverse Visual-Functional Mismatch Between IVUS and FFR
Hsuan-Ling Tseng1, Hsien-Li Kao2
Chi-Mei Hospital, Taiwan1, National Taiwan University Hospital, Taiwan2,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
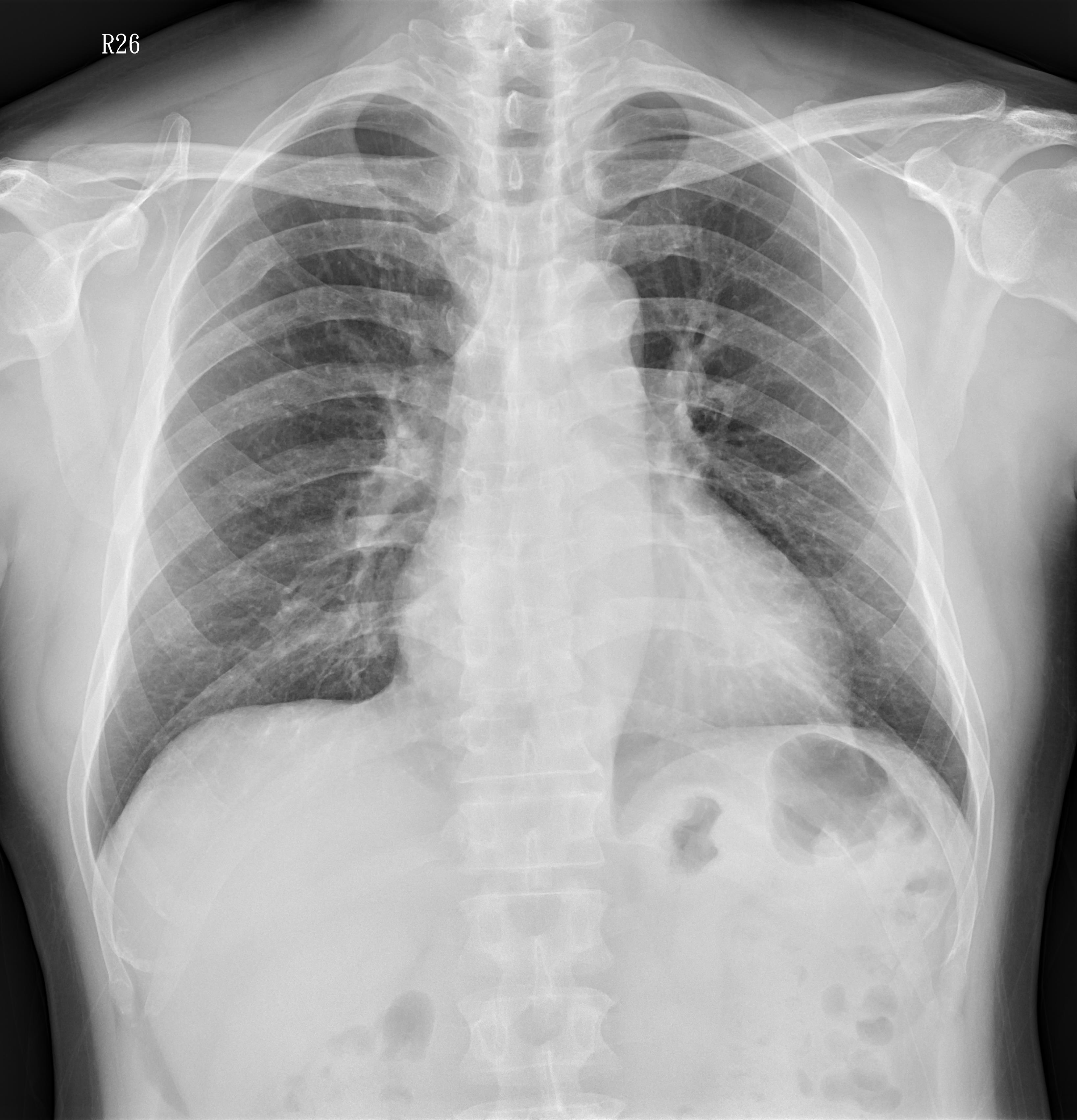
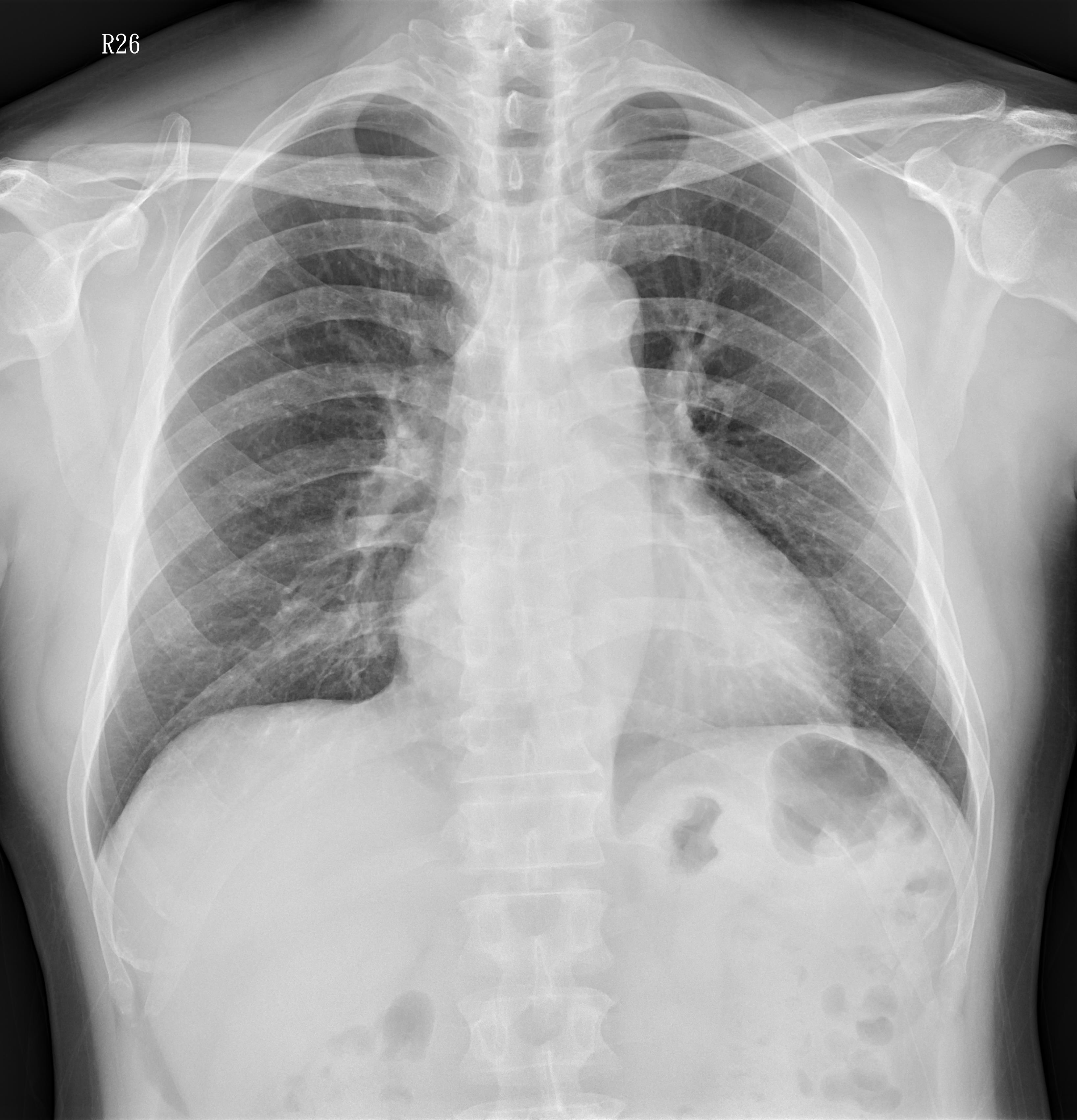
This 54 y/o man was a case of LICAS, HTN, T2DM, and dyslipidemia. He was an ex-smoker. He also had a family history of CAD. The patient complained of intermittent chest tightness since 6 months ago. He denied exertional dyspnea, exertional chest pain, palpitation, syncope, and productive cough recently. He received a thallium scan at the local medical department, and suspected ischemia was told. Previous CXR showed borderline cardiomegaly. The physical exam showed clear BS, RHB with no murmur.
Relevant Test Results Prior to Catheterization
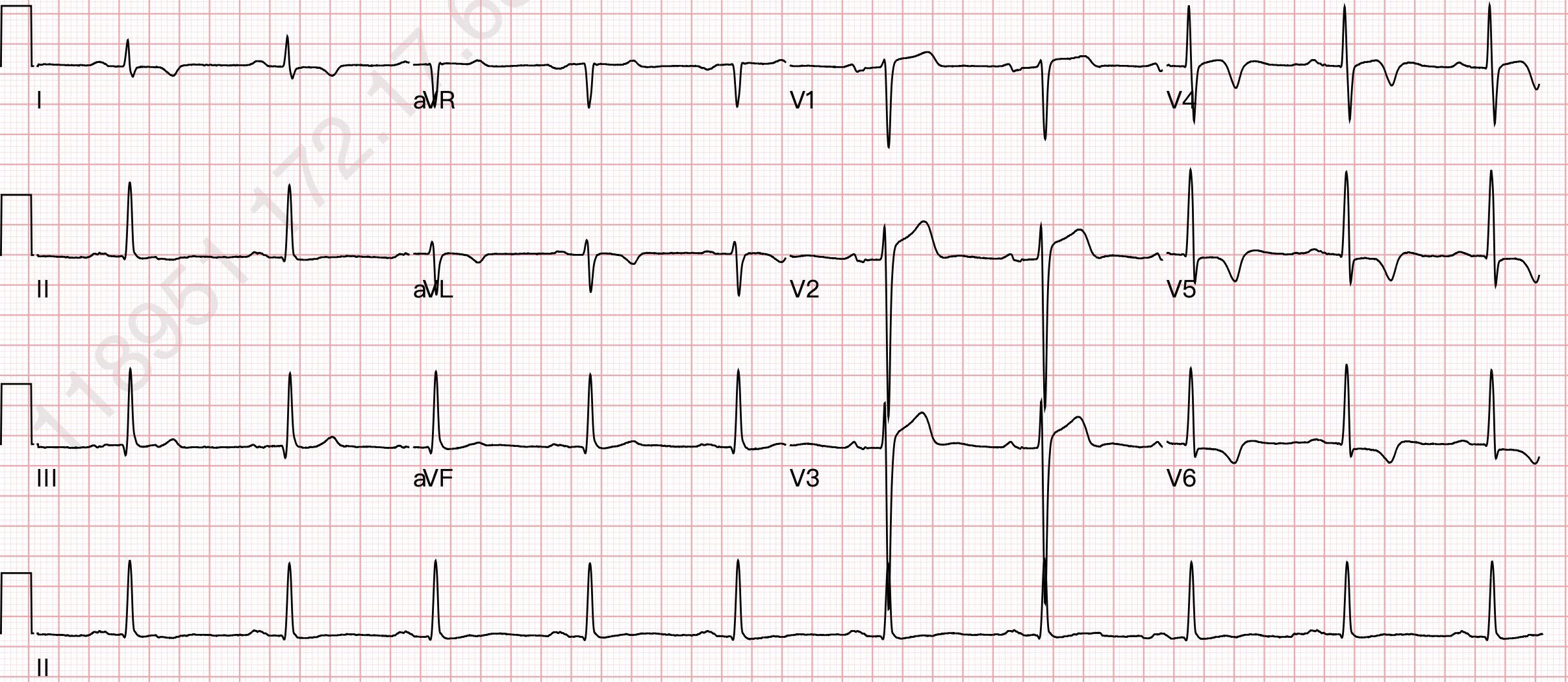
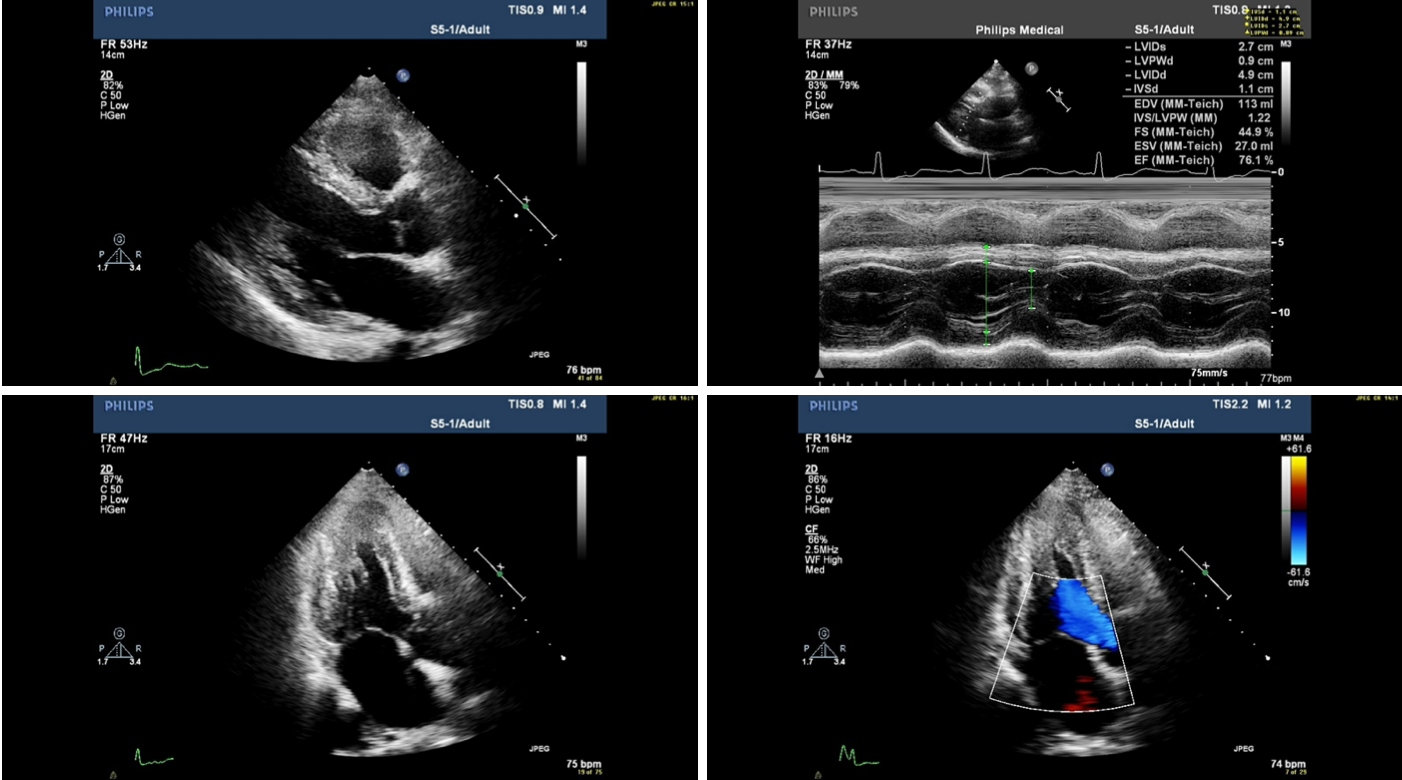
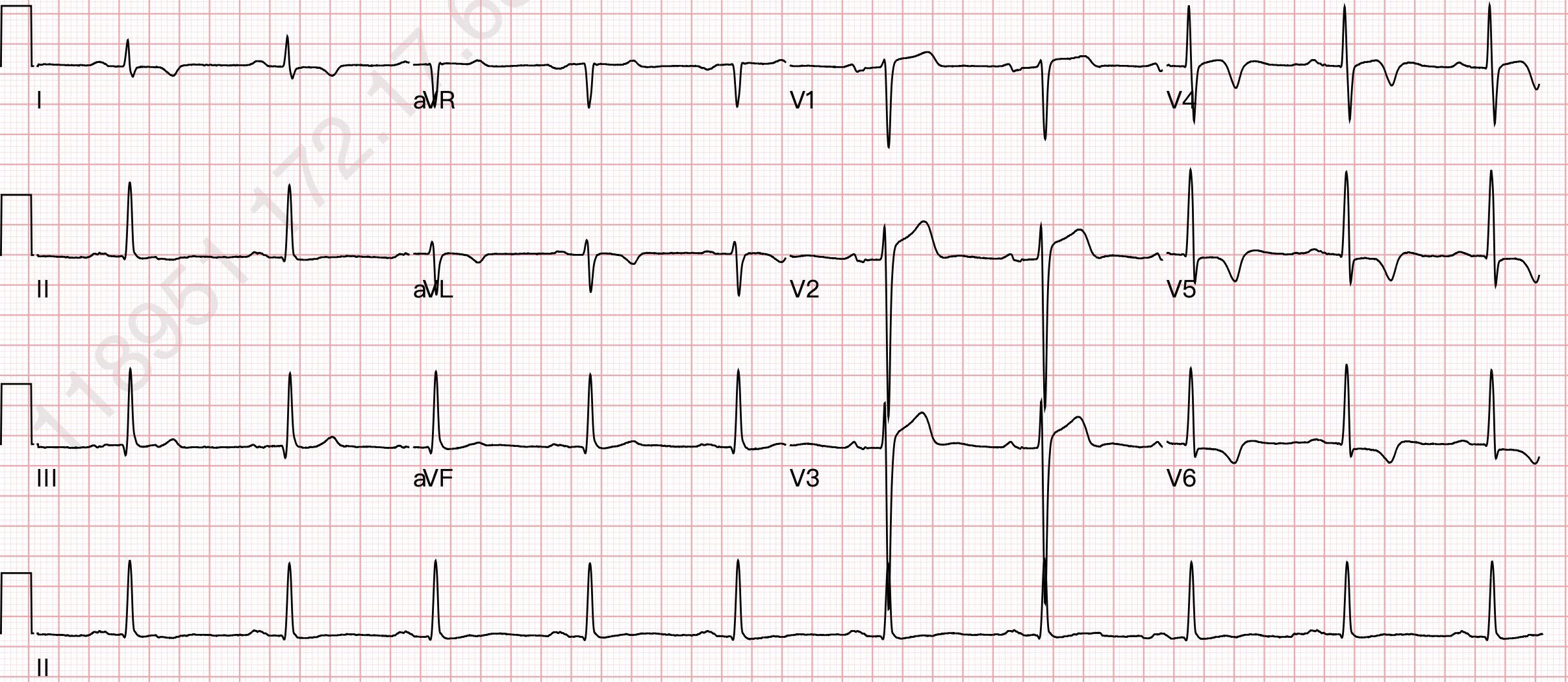
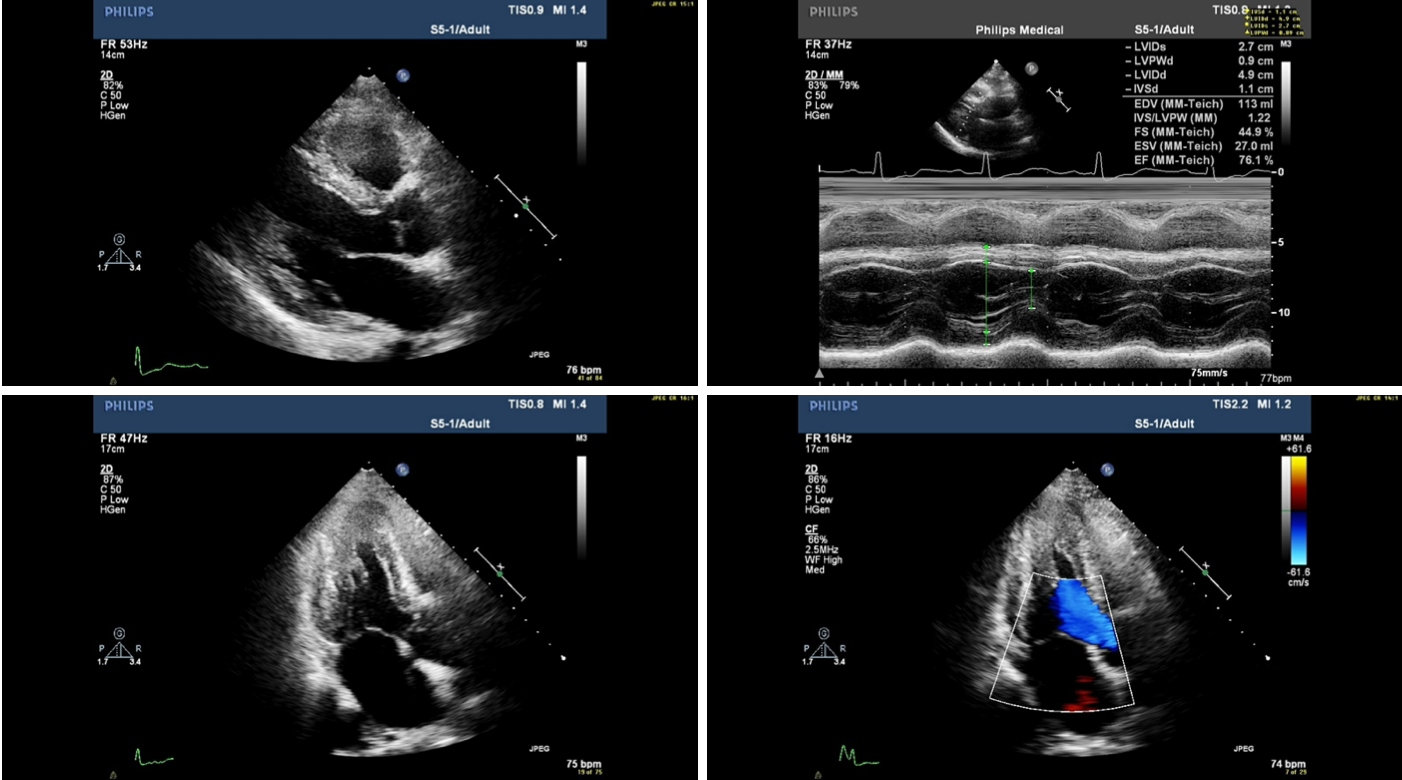
The baseline 12-lead ECG showed SR with LVH and suspected old inferior MI. The treadmill exercise reported ST-changes reaching criteria for positive results. Echocardiography showed normal LV systolic function with no regional wall motion abnormalities.


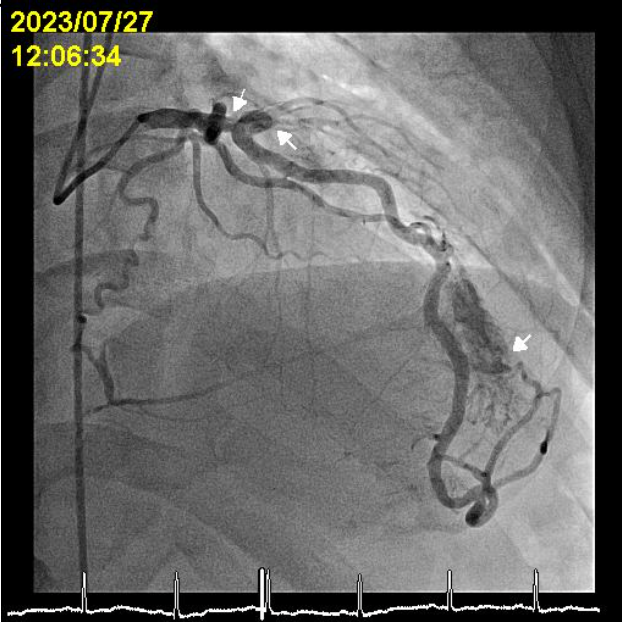
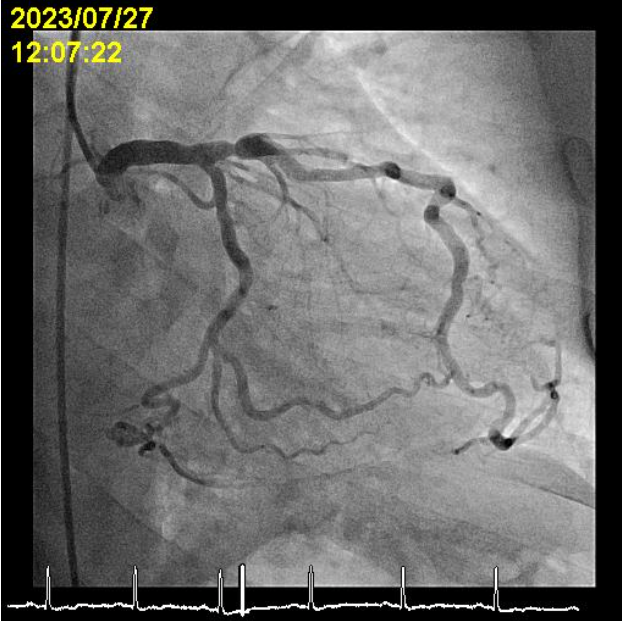
Relevant Catheterization Findings
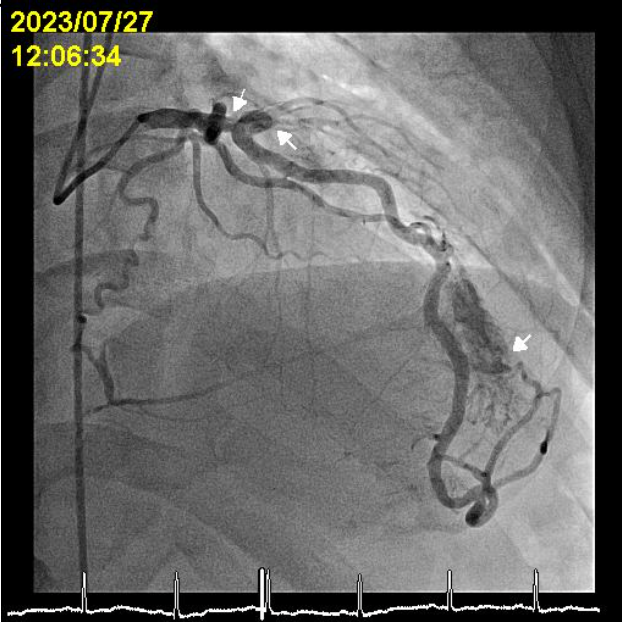
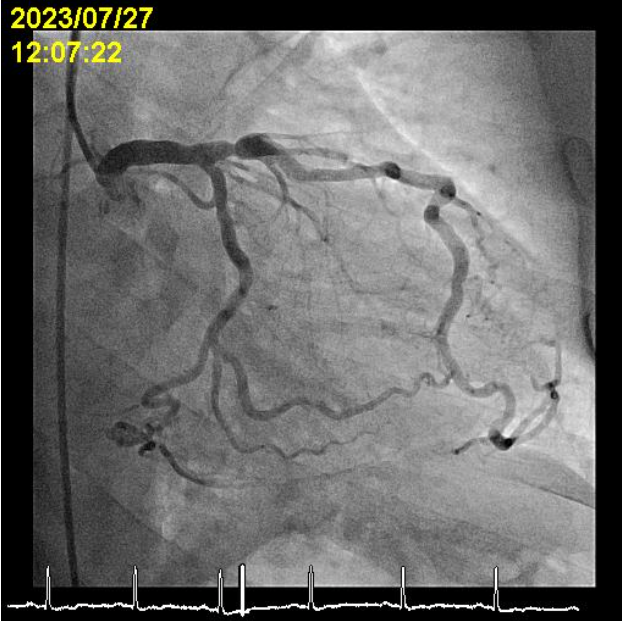
LM: patent


Interventional Management
Procedural Step
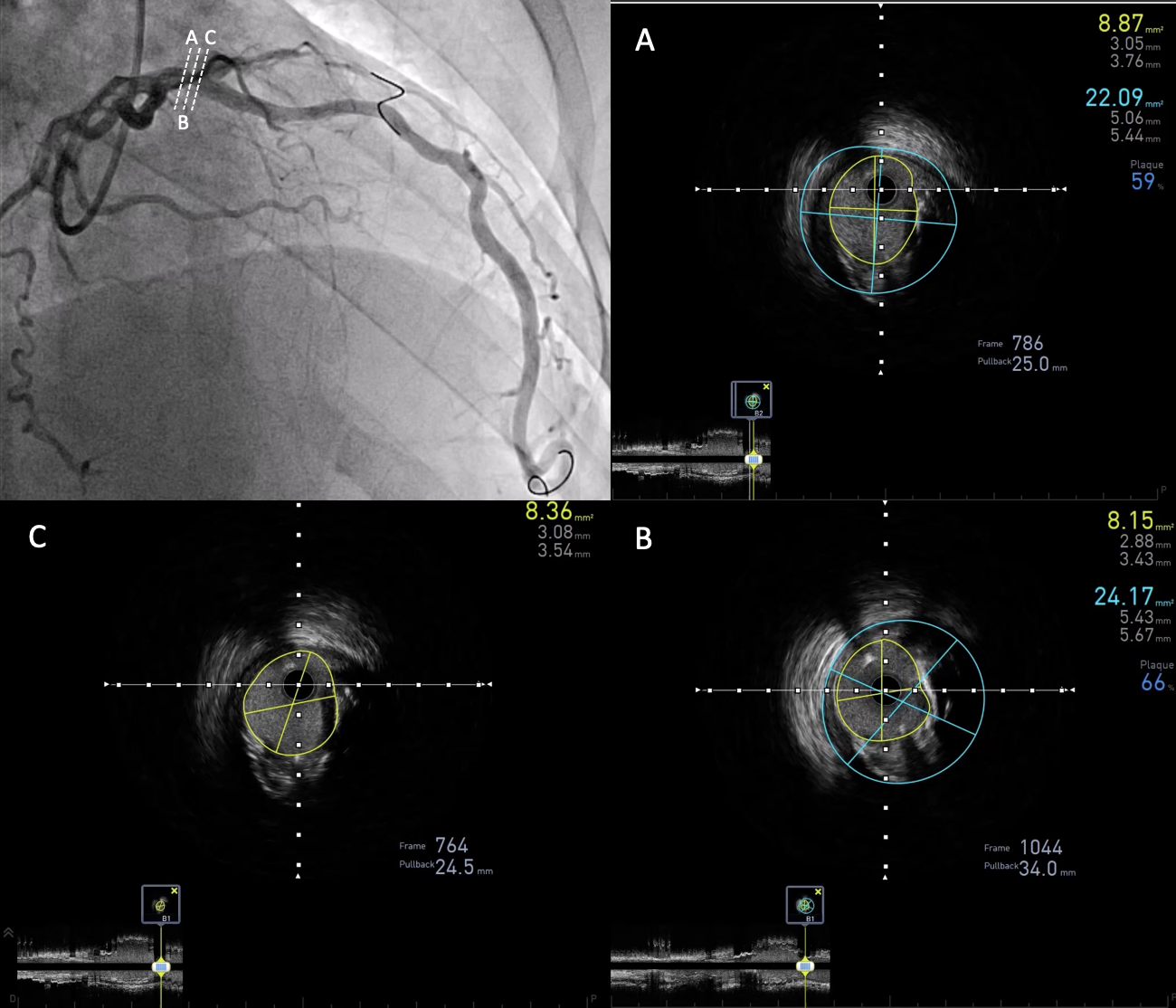
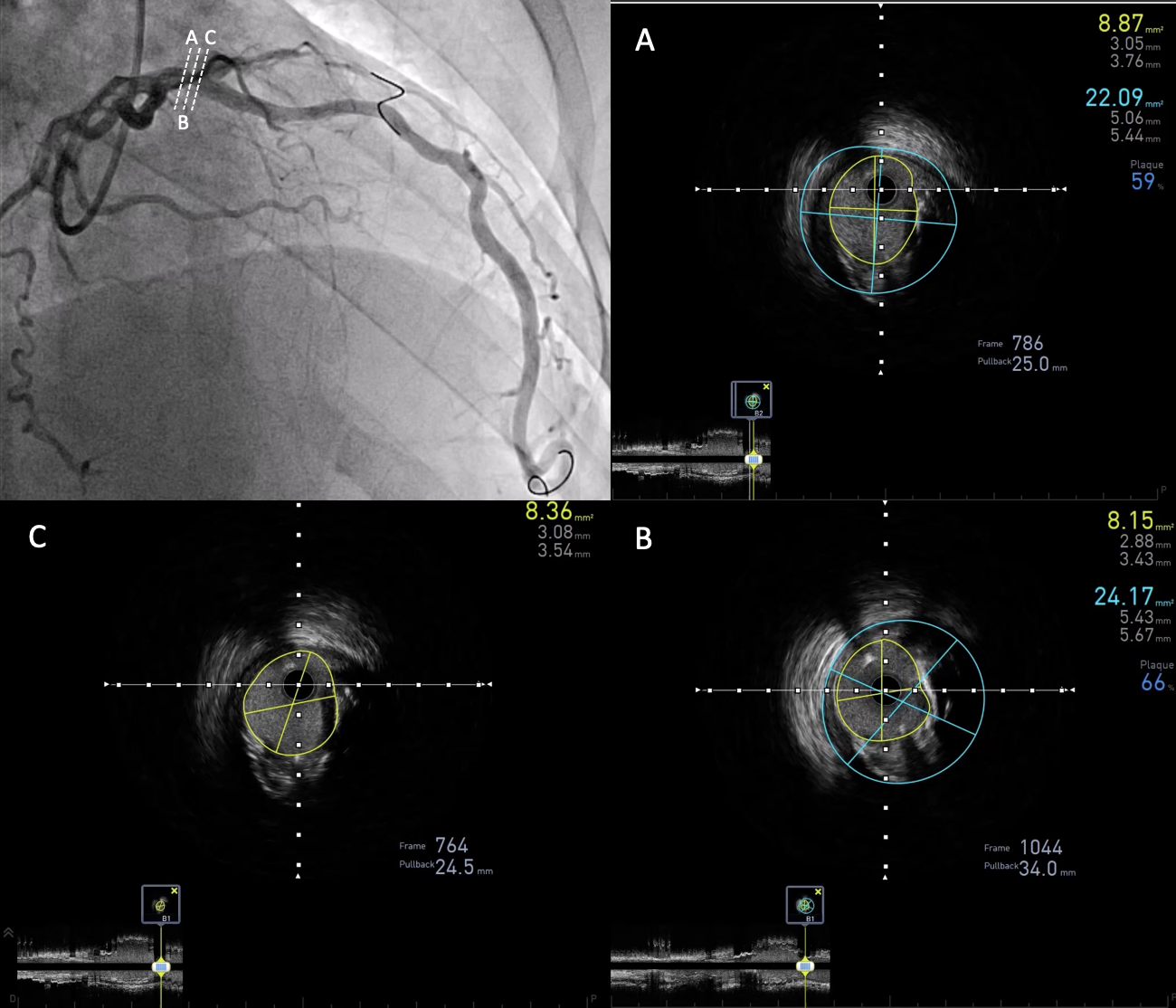
1. Tried to wire D1 CTO with RT Floppy under the support of Mizuki micro-catheter and wired RT Hypercoat to dLAD.




Case Summary
1. The MLA (8.15 mm2) of p-LAD in this patient far exceeds the determined cut-off value of IVUS-derived MLA (> 5~6mm2).

