Lots of interesting abstracts and cases were submitted for TCTAP 2024. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-202
Percutaneous Pulmonary Thrombectomy on ECMO - Principles and Pitfalls
By Ting Wei Teo, Peter Chang, Pipin Kojodjojo, Ivandito Kuntjoro, Ting Ting Low, Yinghao Lim
Presenter
Ting Wei Teo
Authors
Ting Wei Teo1, Peter Chang1, Pipin Kojodjojo2, Ivandito Kuntjoro1, Ting Ting Low1, Yinghao Lim1
Affiliation
National University Heart Centre, Singapore1, Asian Heart and Vascular Centre, Singapore2,
View Study Report
TCTAP C-202
Endovascular - Thrombus Removal Devices and Techniques
Percutaneous Pulmonary Thrombectomy on ECMO - Principles and Pitfalls
Ting Wei Teo1, Peter Chang1, Pipin Kojodjojo2, Ivandito Kuntjoro1, Ting Ting Low1, Yinghao Lim1
National University Heart Centre, Singapore1, Asian Heart and Vascular Centre, Singapore2,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
A 38-year-old man presented with acute dyspnoea and near-syncope after toileting. He was morbidly obese with hypertension, non-ischaemic cardiomyopathy, and successfully-ablated atrial fibrillation (CHA2DS2-VASc score 2) no longer on anticoagulation. His pulse rate was irregular at 118 beats per minute with a blood pressure of 79/63 mmHg. Oxygen saturation on room air was 85%. He was tachypneic with a respiratory rate of 35 breaths per minute but physical examination was otherwise unremarkable.
Relevant Test Results Prior to Catheterization
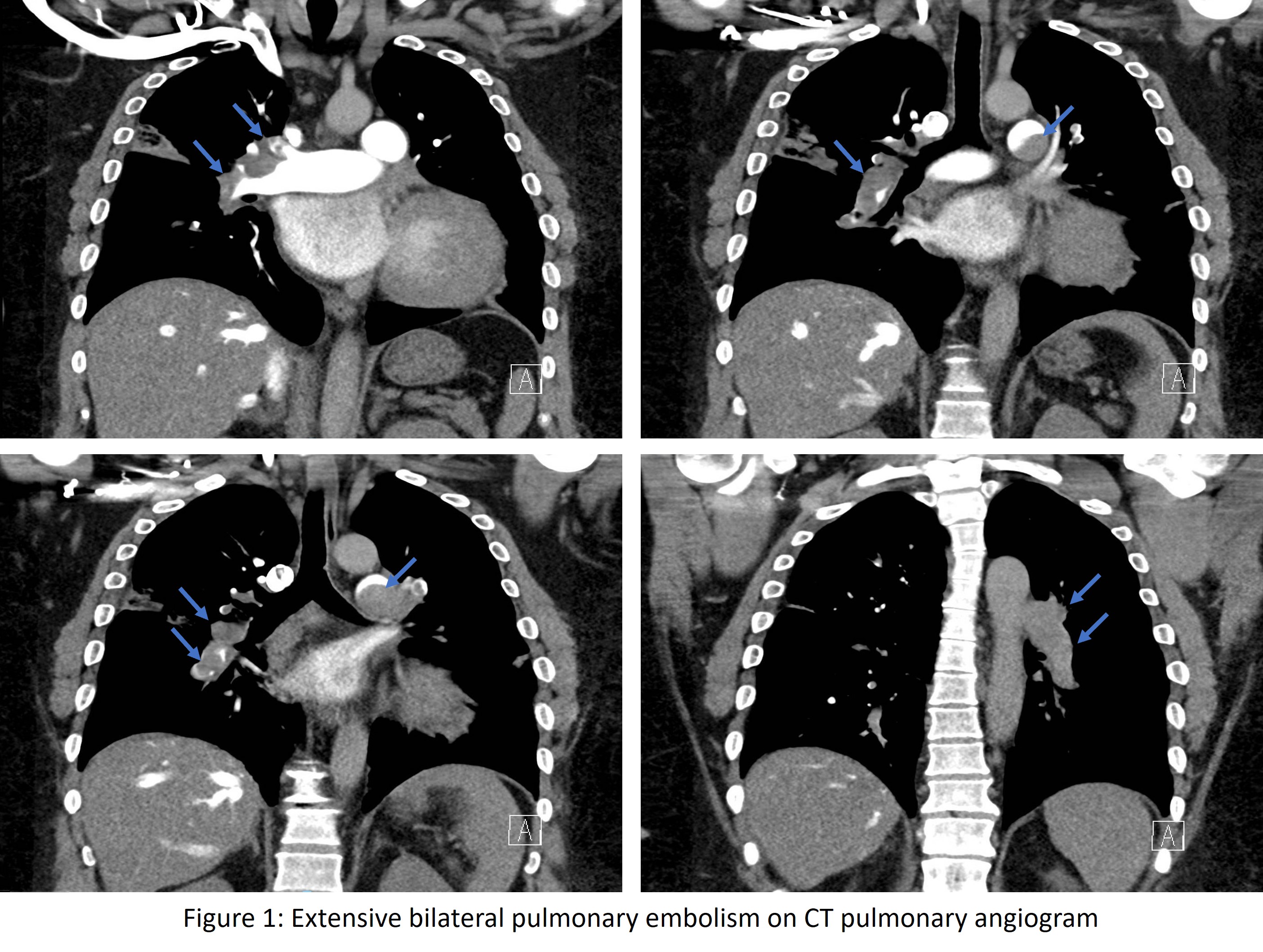
CT pulmonary angiogram (CTPA) showed extensive acute pulmonary embolism, multifocal pulmonary infarcts and right heart strain (Fig 1). 100 mg alteplase was given due to persistent hypoxia and hypotension. He was intubated and initiated on peripheral veno-arterial extracorporeal membrane oxygenation (VA-ECMO) via 25 Fr venous and 19 Fr arterial cannulas in the right common femoral vein and artery respectively. Decision was made for percutaneous pulmonary thrombectomy due to high surgical risks.
Relevant Catheterization Findings
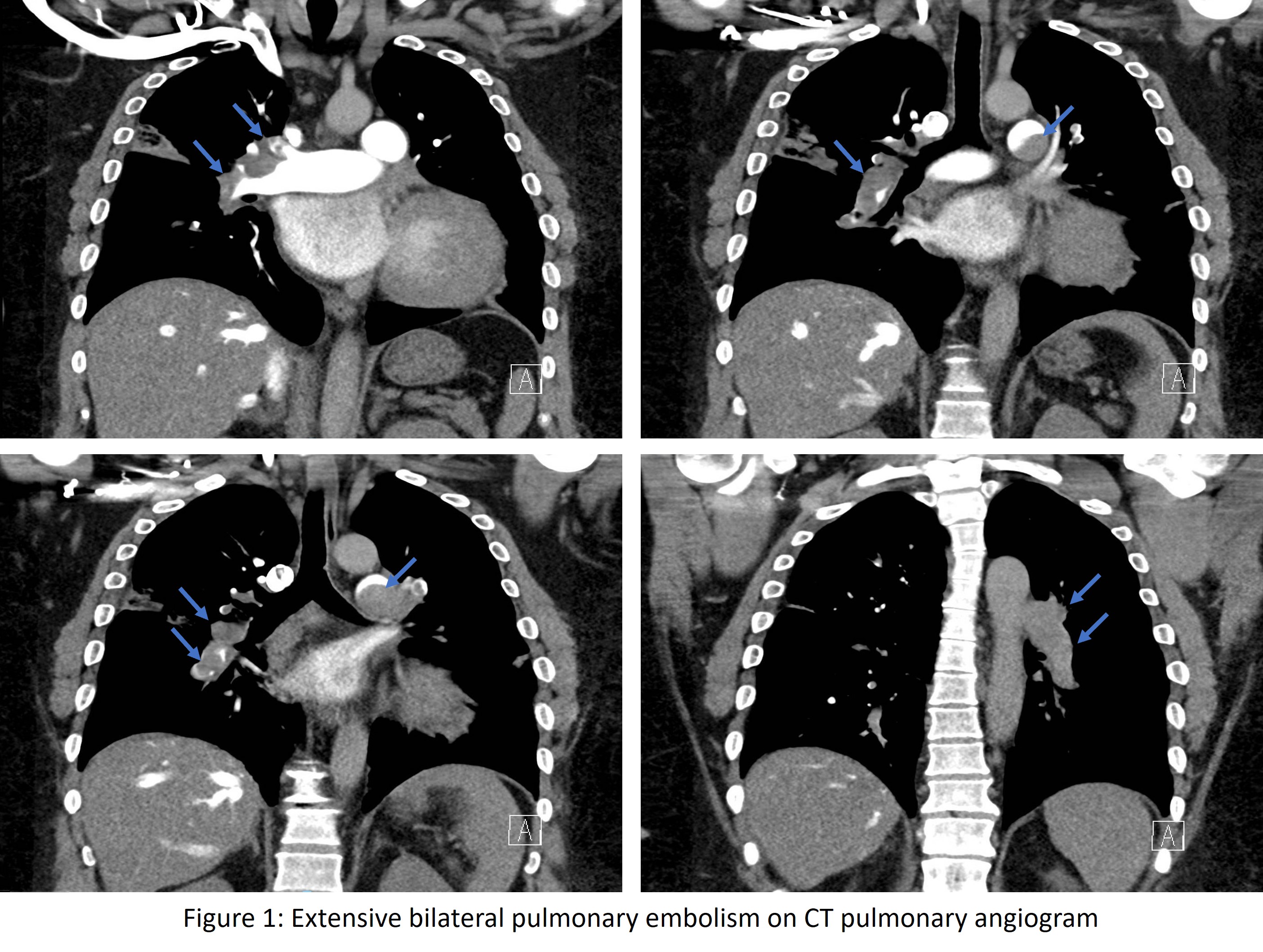
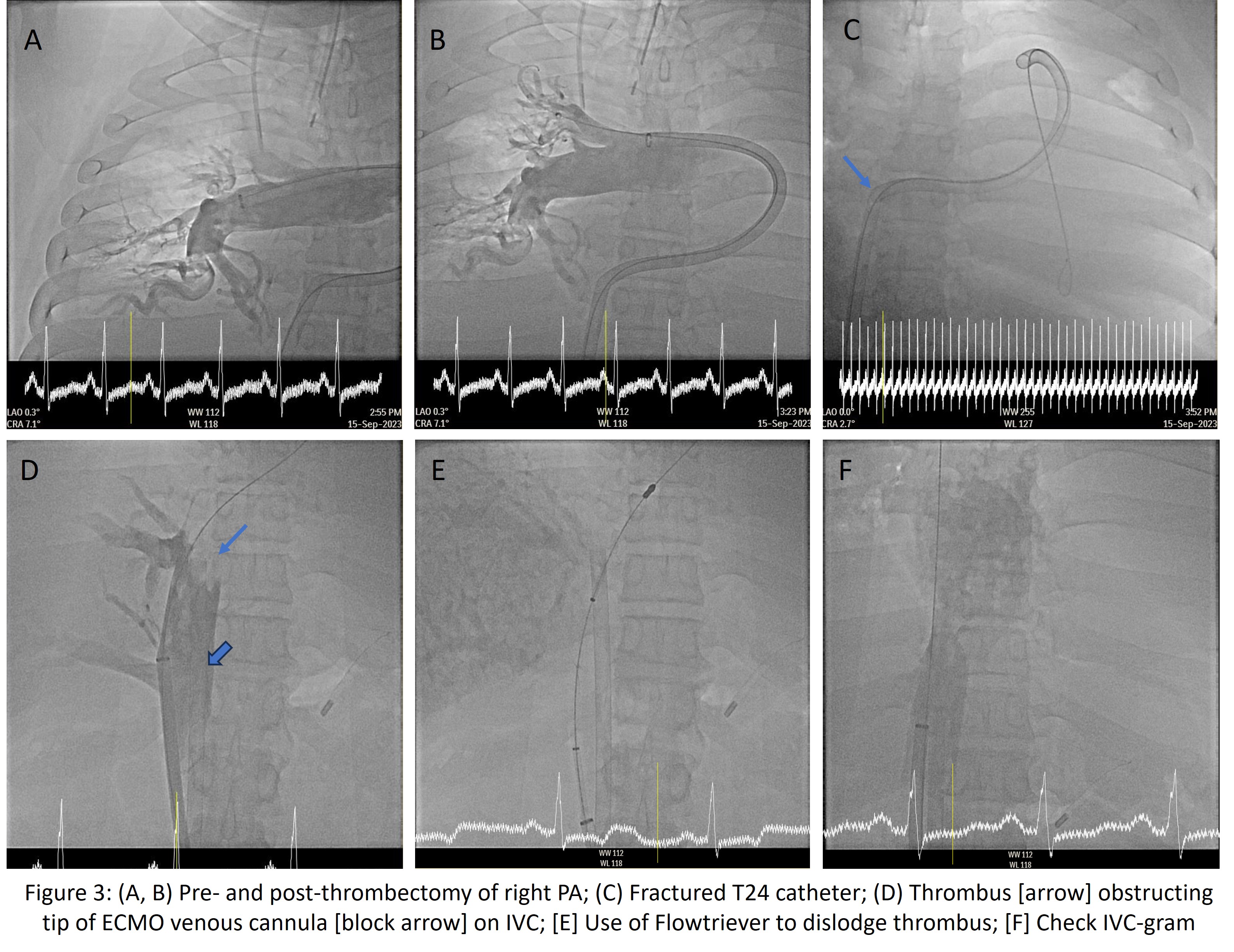
Venogram via left femoral vein access did not reveal any thrombus in iliac veins or inferior vena cava (IVC). IVC dimensions were adequate to allow passage of both 25 Fr ECMO venous cannula and 24 Fr Inari sheath. Bilateral pulmonary arteries (PA) angiography confirmed CTPA findings of extensive bilateral acute pulmonary emboli with complete occlusion of the left PA (Fig 2A, 2B).


Interventional Management
Procedural Step
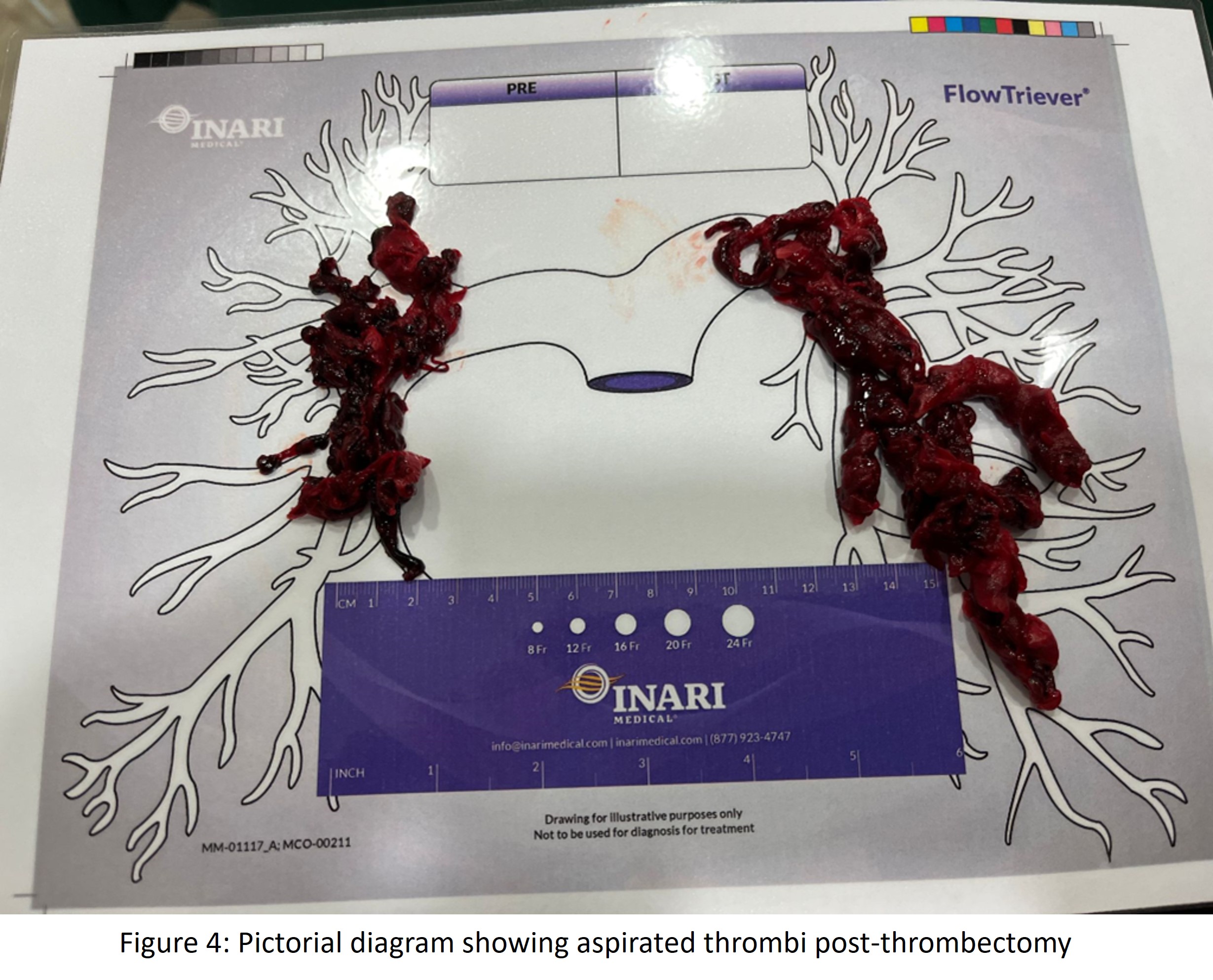
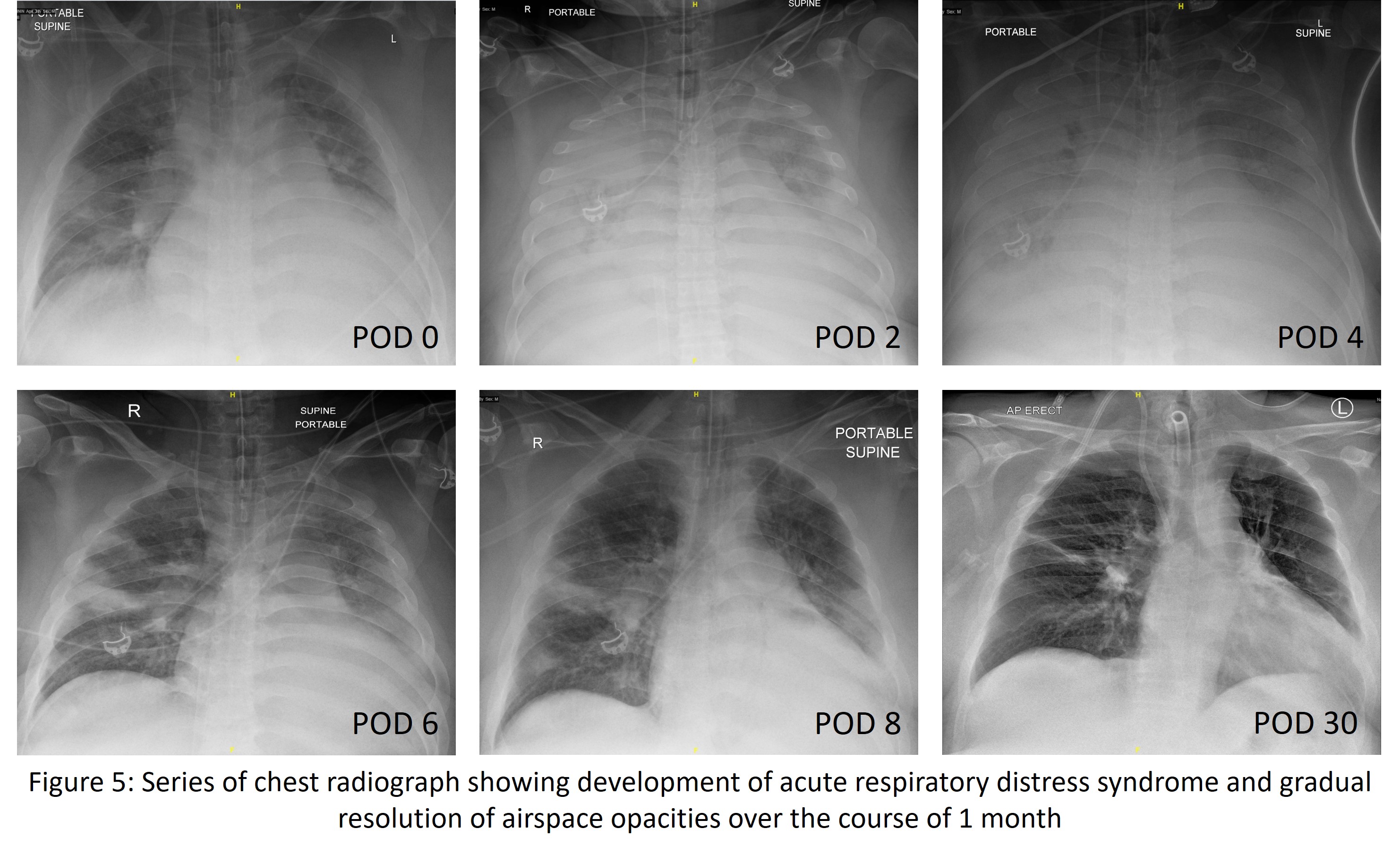
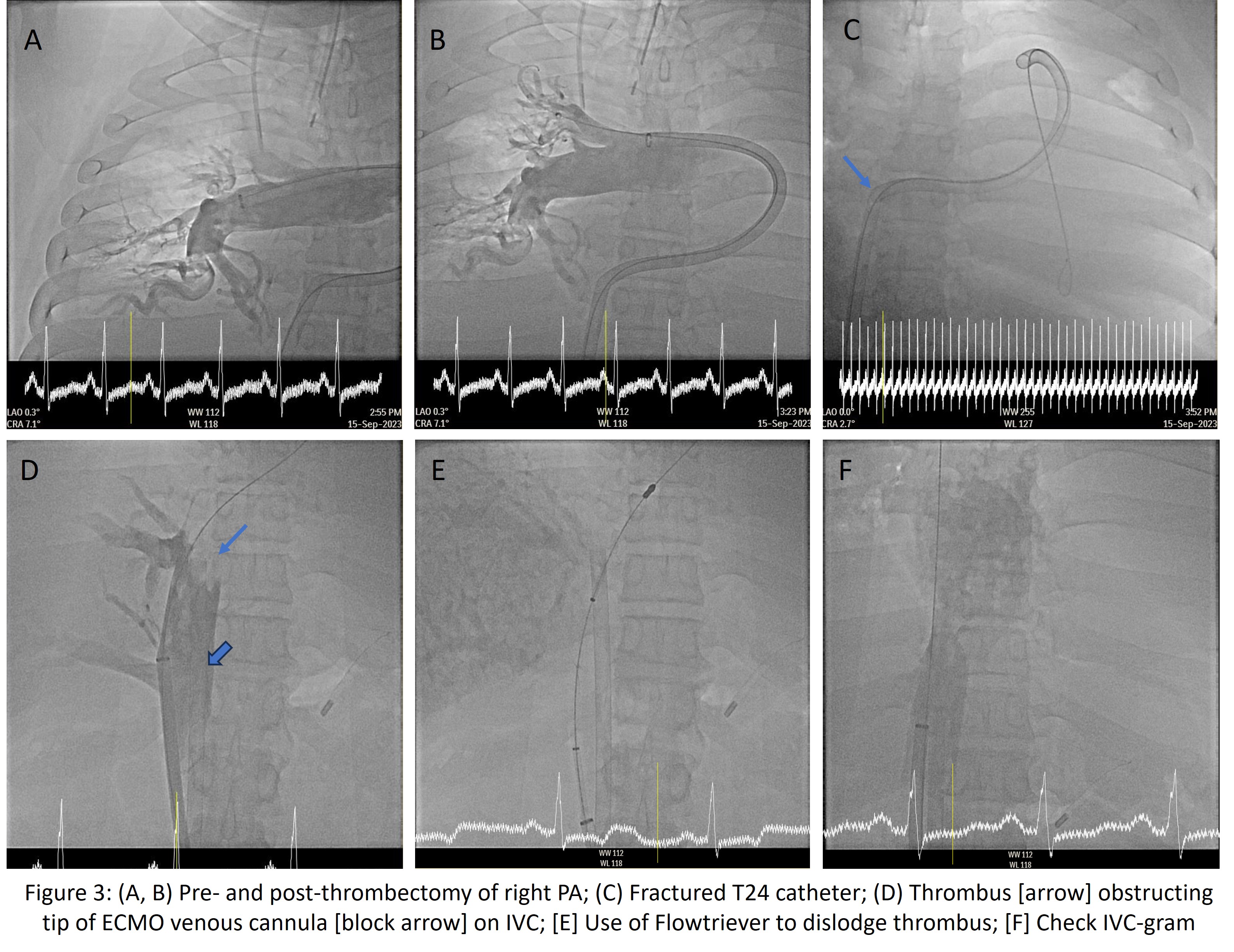
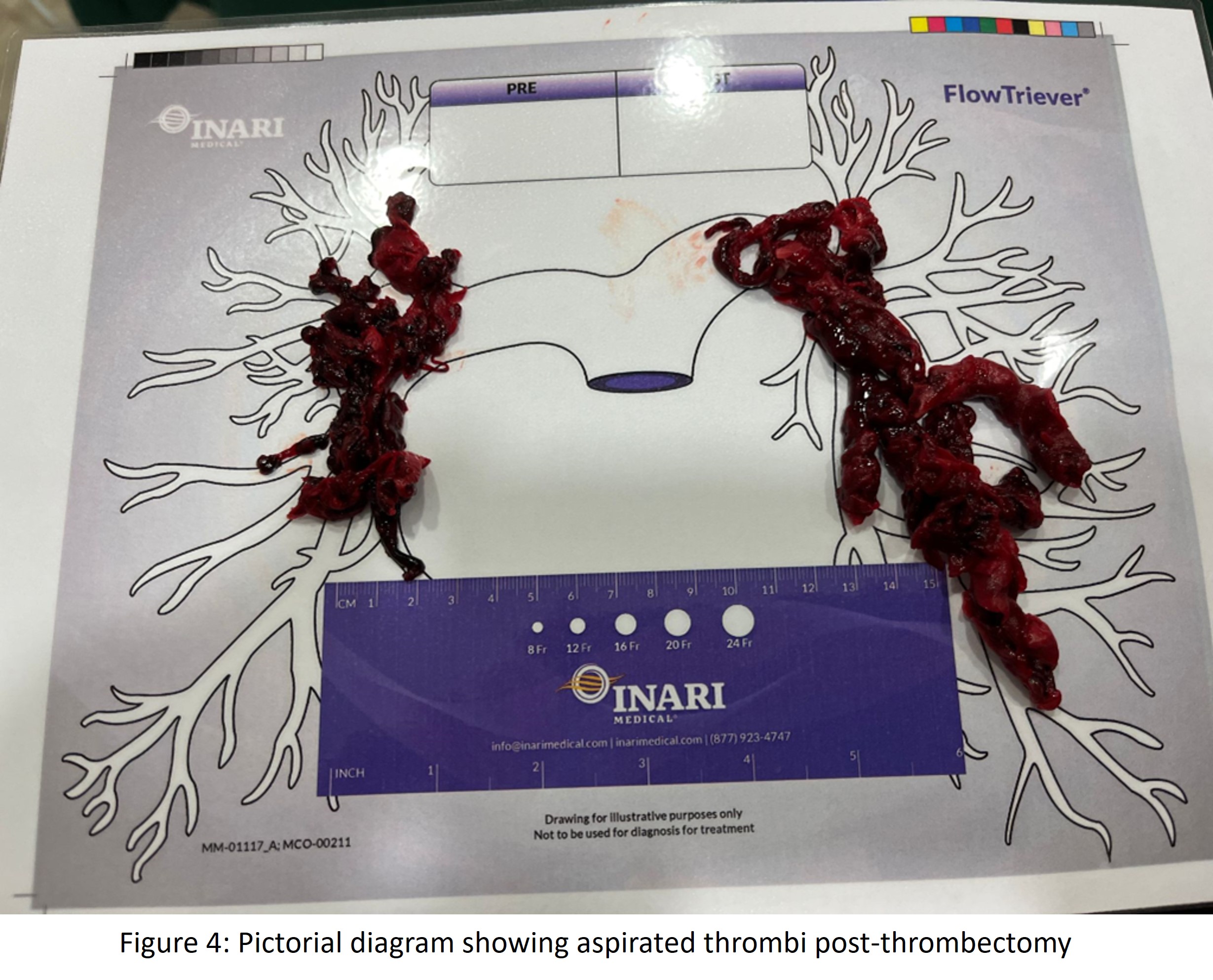
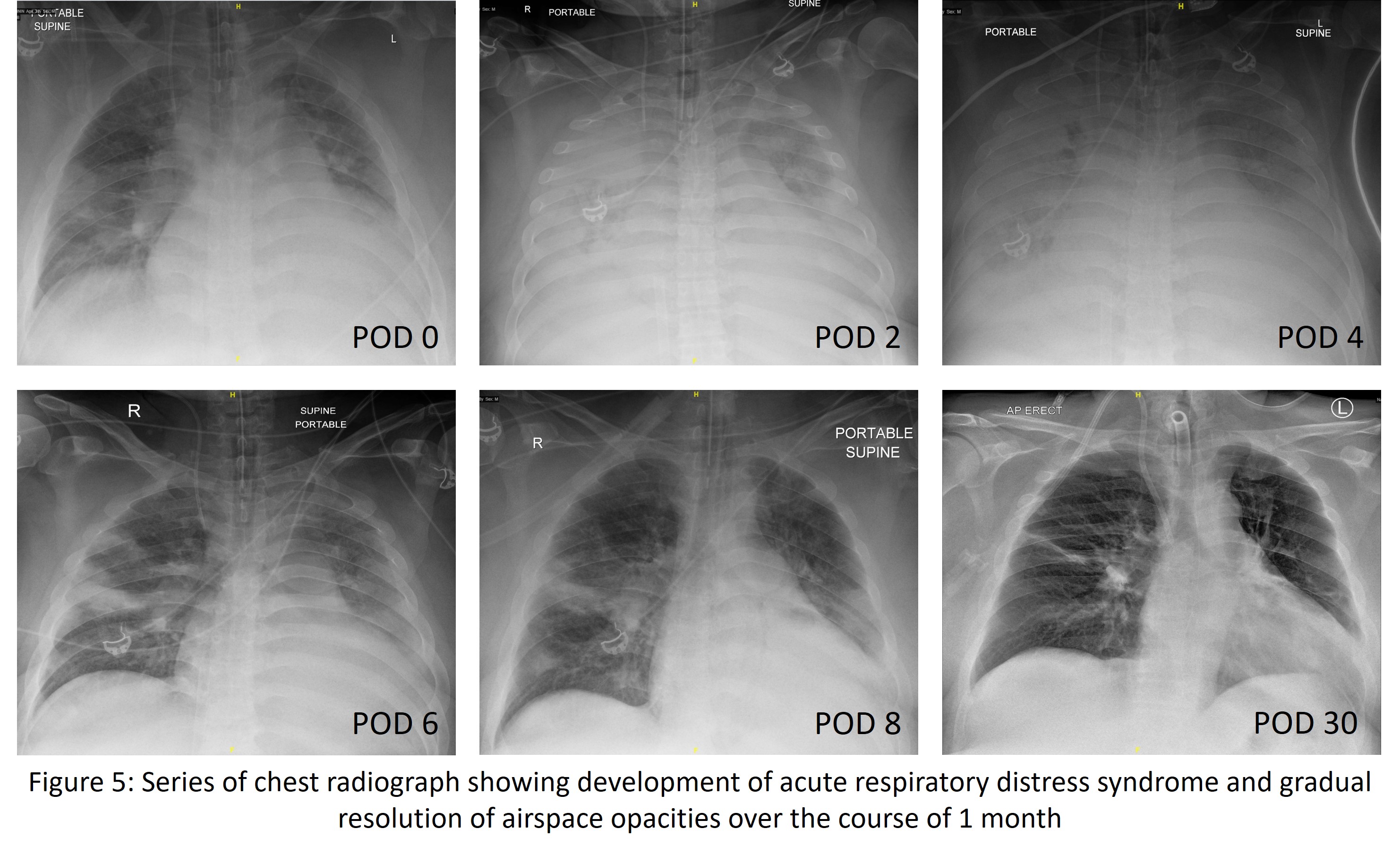
Intri24 Introducer Sheath (Inari Medical, Irvine, CA) was advanced over Amplatz Extra Stiff Guidewire (Boston Scientific Corporation, Boston, MA) into IVC. Triever24 (T24) and Triever16 catheters were advanced over stiff wire to aspirate thrombi in the right lower branches and truncus anterior with good clearance of lobar to segmental arteries. (Fig 3A, 3B). ECMO circuit was clamped transiently before aspirations to allow PA flow.Aspiration with T24 in left PA ostium was unsuccessful as it was occluded. 5 Fr Pigtail was used for maceration as FlowTriever Disc XL (Inari Medical, Irvine, CA) failed to extract thrombi. Due to large right atrium (RA) and recurrent T24 buckling, the catheter was fractured, requiring extraction (Fig 3C). New T24 was inserted deeper into the left PA and aspiration led to ‘lollipopping’ due to large thrombus size. With T24 pull-back, the thrombus dislodged onto ECMO venous cannula tip, causing high venous pressures and low cardiac output (Fig 3D). Flowtriever Discs dislodged the thrombus (Fig 3E) while ECMO venous cannula was retracted. Circuit flow was restored after flushing.After thrombi removal, there was no overt IVC thrombus (Fig 3F) with residual thrombi in left segmental arteries albeit with good perfusion. Mean PA pressure reduced by 12mmHg.Post-procedure, inotropic support was increased due to acute respiratory distress syndrome from reperfusion injury (Fig 5), requiring lung protective measures and VA-ECMO for oxygenation until POD6.
Case Summary
There is growing interest in catheter-directed therapy for venous thromboembolism. We illustrate principles of managing pulmonary thrombectomy on ECMO: (a) multiple large bore access, (b) ECMO circuit clamp to allow PA flow for aspiration, and (c) venous cannula and aspiration catheter interactions. Complications and bailout strategies include (a) catheter fracture due to large RA size and recurrent catheter buckling, (b) ECMO venous cannula occlusion from large thrombus migration, and (c) reperfusion injury due to extensive thrombus removal and pre-existing pulmonary infarcts. Operators should be aware of ECMO management and potential complications for better peri- and post-procedural care.

