Lots of interesting abstracts and cases were submitted for TCTAP 2024. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-222
A Case of Transcatheter Ventricular Septal Defect Closure in a Challenging Pectus Excavatum Patient
By Kantasit Wisanuvej, Krissada Meemook, Tawai Ngernsritrakul
Presenter
Kantasit Wisanuvej
Authors
Kantasit Wisanuvej1, Krissada Meemook2, Tawai Ngernsritrakul1
Affiliation
Ramathibodi Hospital, Thailand1, Ramathibodi Hospital Mahidol University, Thailand2,
View Study Report
TCTAP C-222
Structural - Other Structural Interventions
A Case of Transcatheter Ventricular Septal Defect Closure in a Challenging Pectus Excavatum Patient
Kantasit Wisanuvej1, Krissada Meemook2, Tawai Ngernsritrakul1
Ramathibodi Hospital, Thailand1, Ramathibodi Hospital Mahidol University, Thailand2,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
Patient has been diagnosed with perimembranous VSD since childhood, recently experienced progressive dyspnea for a year with NYHA Class II, and paroxysmal nocturnal dyspnea, indicative of heart failure. Improvement with diuretics was observed. Surgical VSD correction was turned-down due to severe pectus excavatum. As a result, the patient was referred to our facility for transcatheter VSD closure, given concerns about surgical risks related to the pectus excavatum.

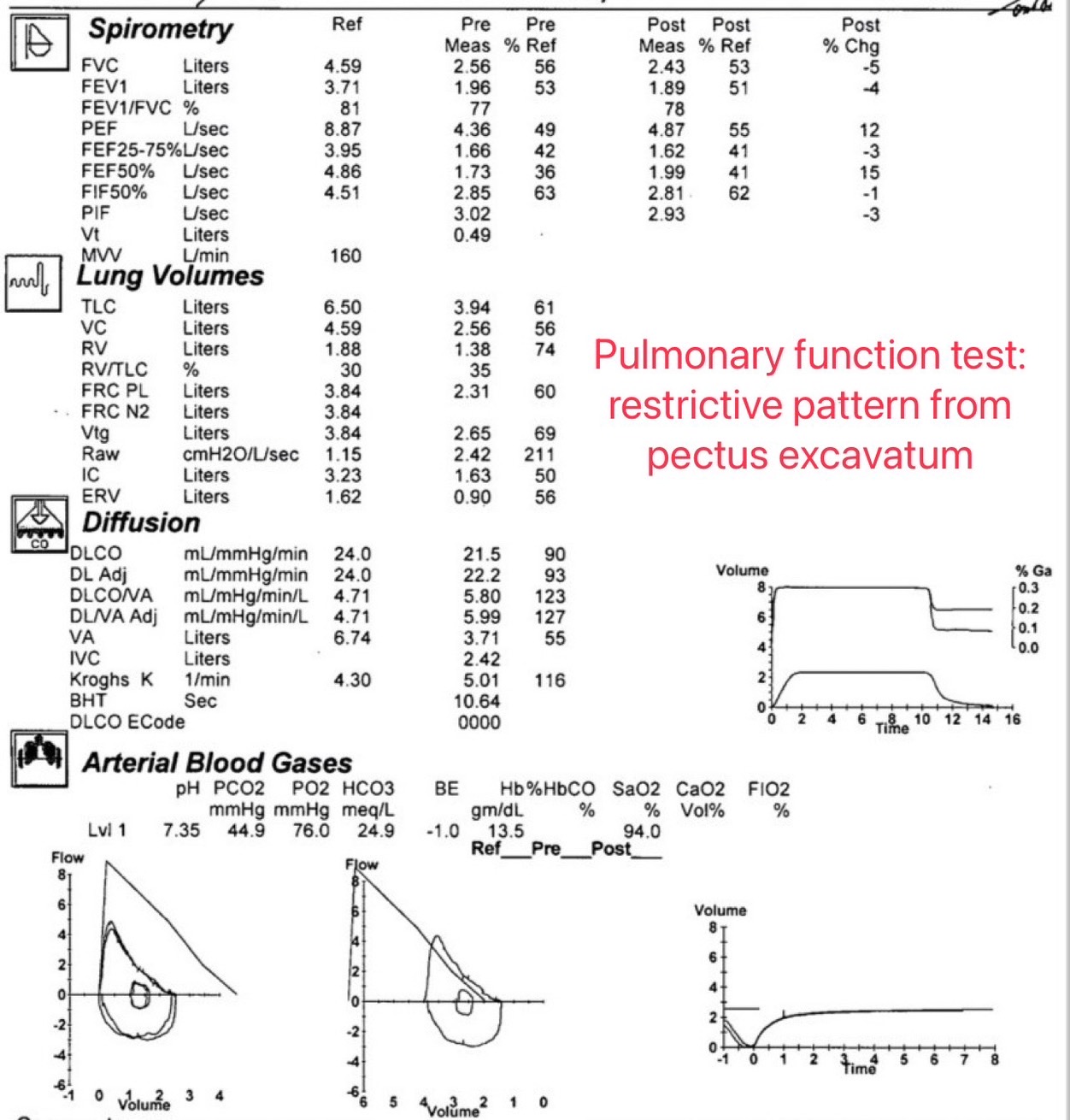

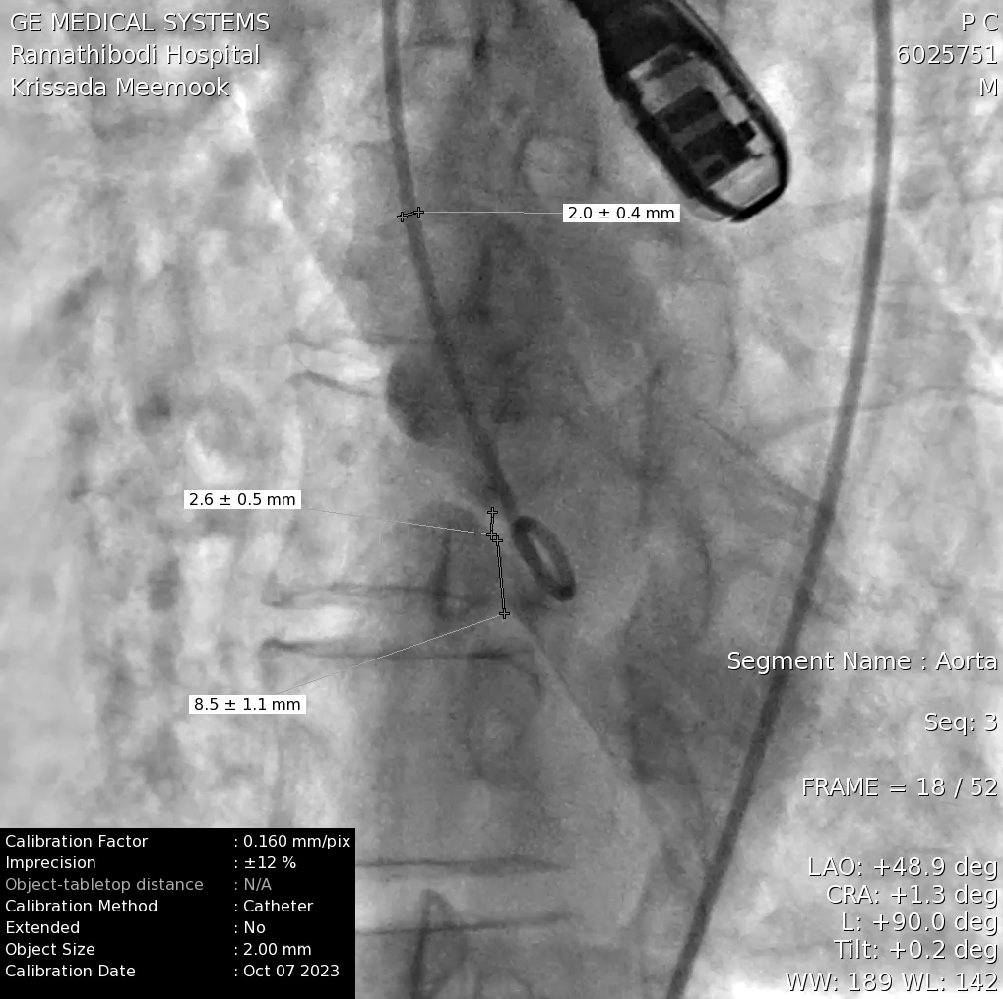
Relevant Test Results Prior to Catheterization
Laboratory tests were unremarkable. ECG showed no abnormalities. Chest X-ray revealed cardiomegaly and pectus excavatum. TTE and TEE demonstrated normal ventricular function (LVEF 66%), a dilated left ventricle (LVIDd 5.4 cm), an 11x5 mm perimembranous VSD causing a left-to-right shunt, and an intact interatrial septum. No endocarditis was detected, and all four pulmonary veins drained into the left atrium, with no significant valvular stenosis or regurgitation.






Relevant Catheterization Findings
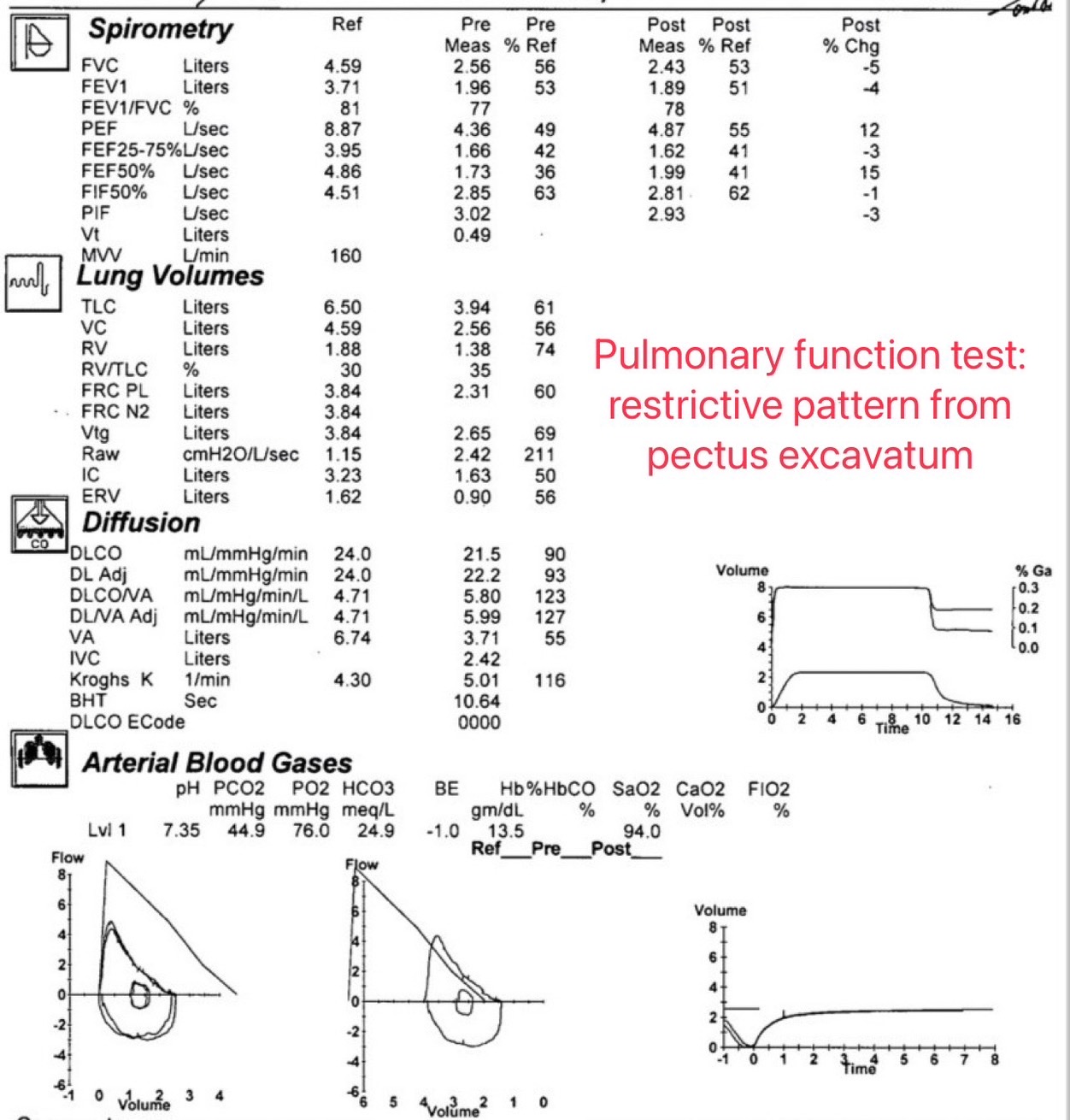
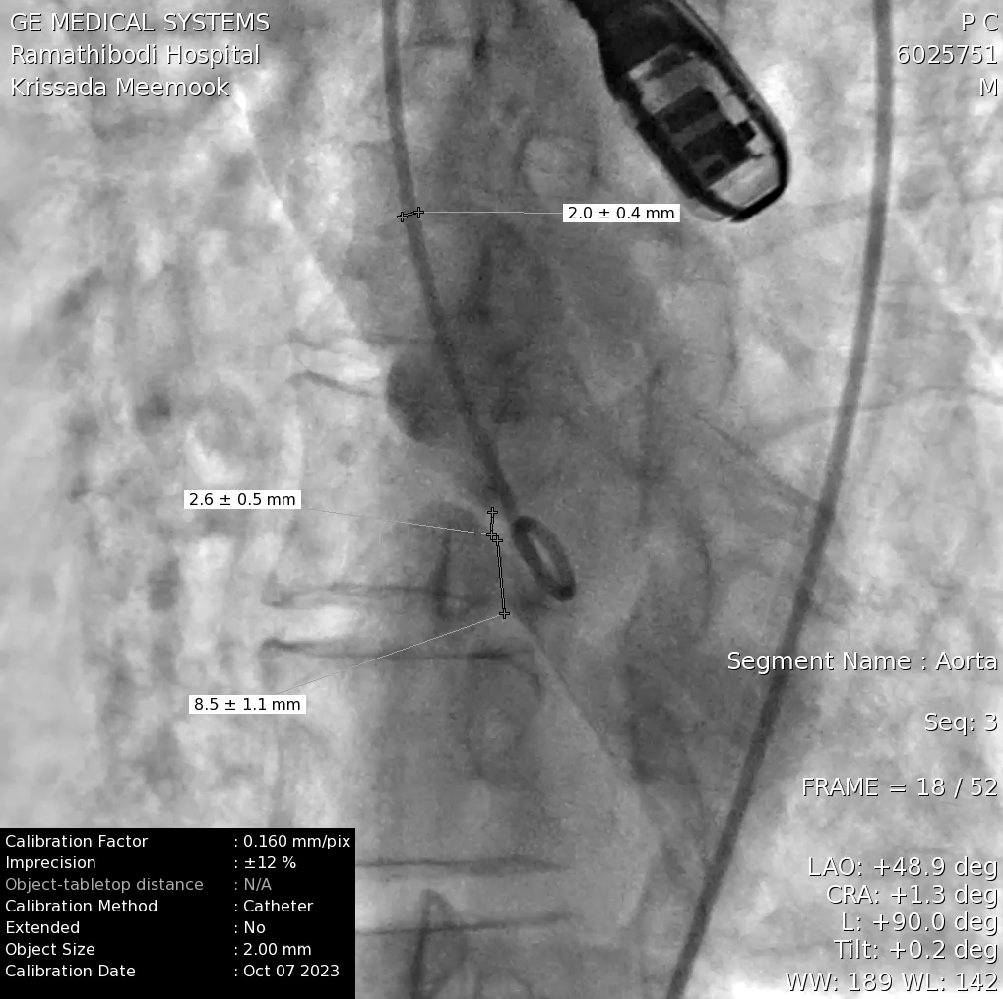
Right heart catheterization revealed the absence of an evident oxygen step-up and the absence of pulmonary hypertension (mean pulmonary arterial pressure: 19 mmHg).Additionally, it confirmed the presence of a significant left-to-right shunt with a pulmonary-to-systemic flow ratio (Qp:Qs) of 2.2. The left ventriculogram also demonstrated an 8.2 mm ventricular septal defect with a left-to-right shunt.


Interventional Management
Procedural Step
-The patient underwent a procedure under general anesthesia.






Case Summary
This patient required VSD closure due to LV volume load without pulmonary hypertension. While surgical closure typically yields low operative mortality and favorable long-term results, the presence of pectus excavatum and resultant restrictive lung disease posed a high operative risk. Therefore, we opted for an alternative method: transcatheter closure. Despite the inherent risks like complete AV block, TR, and AR associated with transcatheter VSD closure, the procedure was completed without any complications in this case.

