Lots of interesting abstracts and cases were submitted for TCTAP 2024. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-116
A Challenging Case of a Difficult-To-Wire Diagonal With an Unexpected Perforation!
By An Shing Ang, Eran Wen Jun Sim, Thet Khaing, Fahim Jafary
Presenter
An Shing Ang
Authors
An Shing Ang1, Eran Wen Jun Sim2, Thet Khaing2, Fahim Jafary2
Affiliation
Woodlands Health, Singapore1, Tan Tock Seng Hospital, Singapore2,
View Study Report
TCTAP C-116
Coronary - Complication Management
A Challenging Case of a Difficult-To-Wire Diagonal With an Unexpected Perforation!
An Shing Ang1, Eran Wen Jun Sim2, Thet Khaing2, Fahim Jafary2
Woodlands Health, Singapore1, Tan Tock Seng Hospital, Singapore2,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
The patient is a 59-year-old gentleman who presented for Non-ST-elevation myocardial infarction (NSTEMI). He has a past medical history of hypertension, hyperlipidemia, and smoking. He had undergone percutaneous coronary intervention (PCI) to his right coronary artery (RCA) a few days earlier (Figure 1 and 2) and was brought back to the lab for staged PCI to the left anterior descending artery (LAD). Physical examination was unremarkable.




Relevant Test Results Prior to Catheterization
His ECG showed T wave inversions in the inferior leads (Figure 3). His laboratory test results were within normal limits before his staged PCI. His creatinine was 78 umol/L (60-105), hemoglobin was 13.0g/dL (13.6-16.6), and platelet count was 279 x109. (150-360 x109). Transthoracic echocardiogram showed a left ventricular ejection fraction of 55% with regional wall motion abnormalites in the RCA territory.


Relevant Catheterization Findings
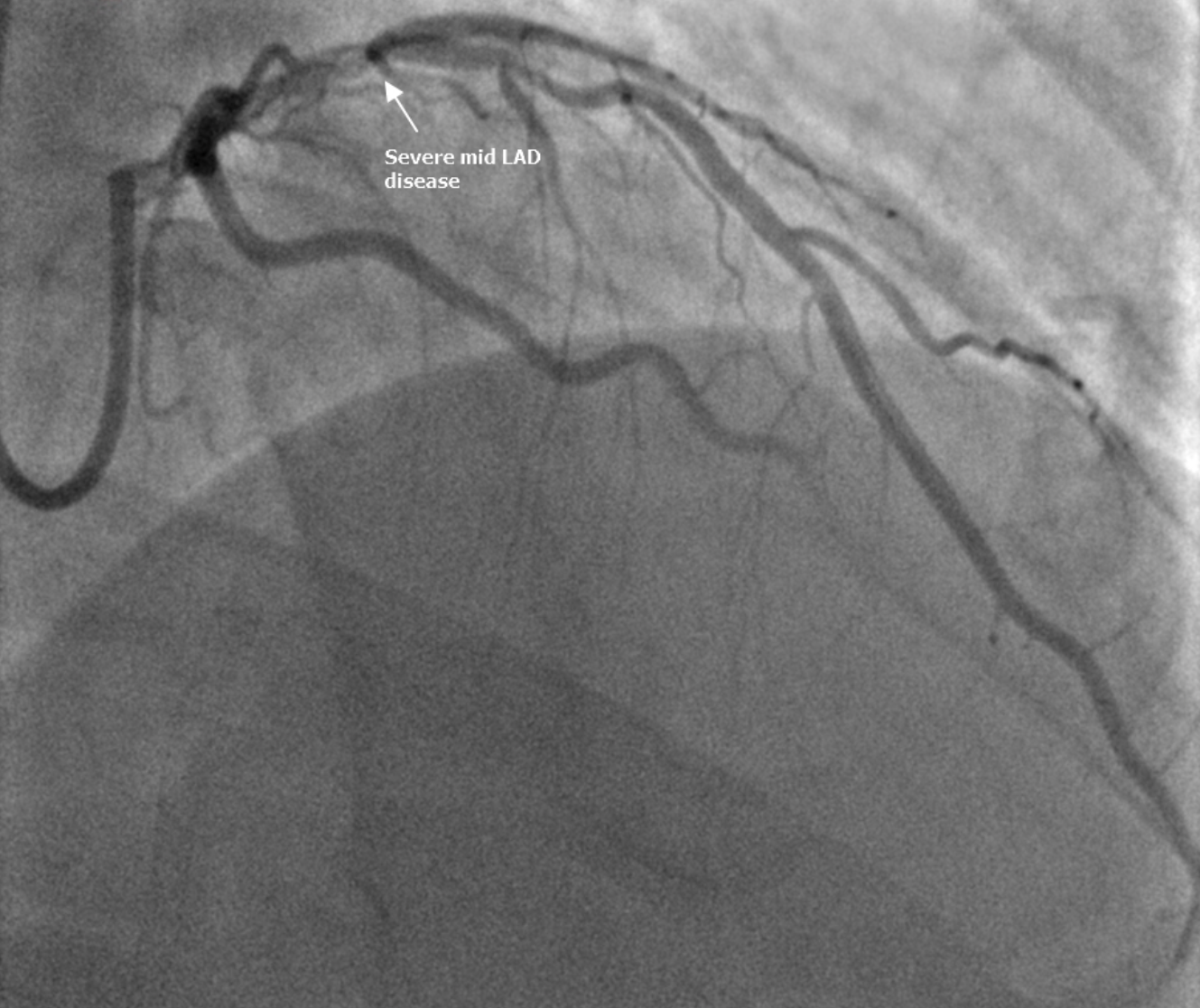
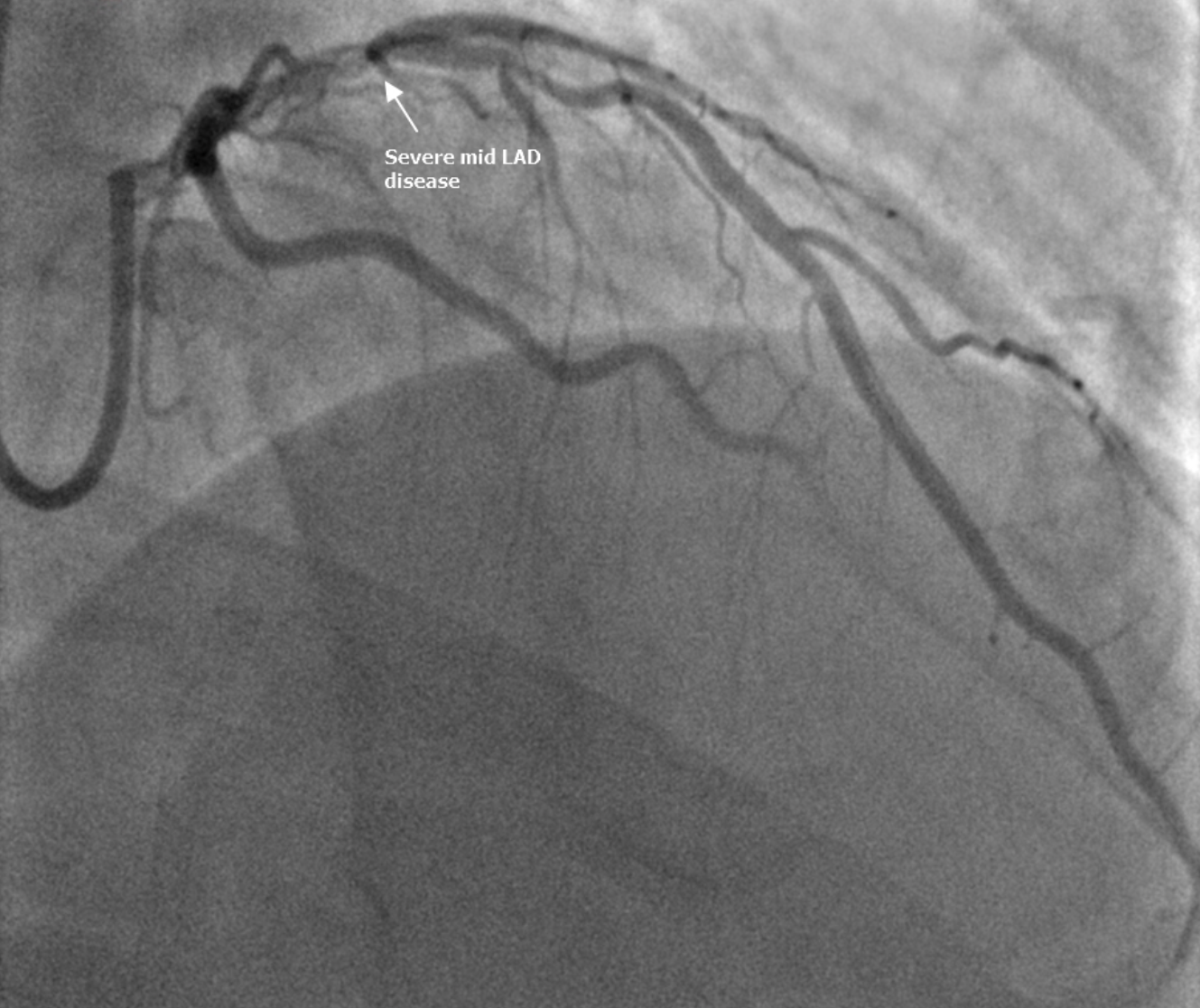
Coronary angiogram revealed patent RCA stents. There was an 80% proximal LAD stenosis just proximal to a large 1st diagonal branch (D1), which had a 70% ostial stenosis and a retroflexed origin (Figure 4 and 5). The left main and left circumflex artery were free of significant disease.


Interventional Management
Procedural Step
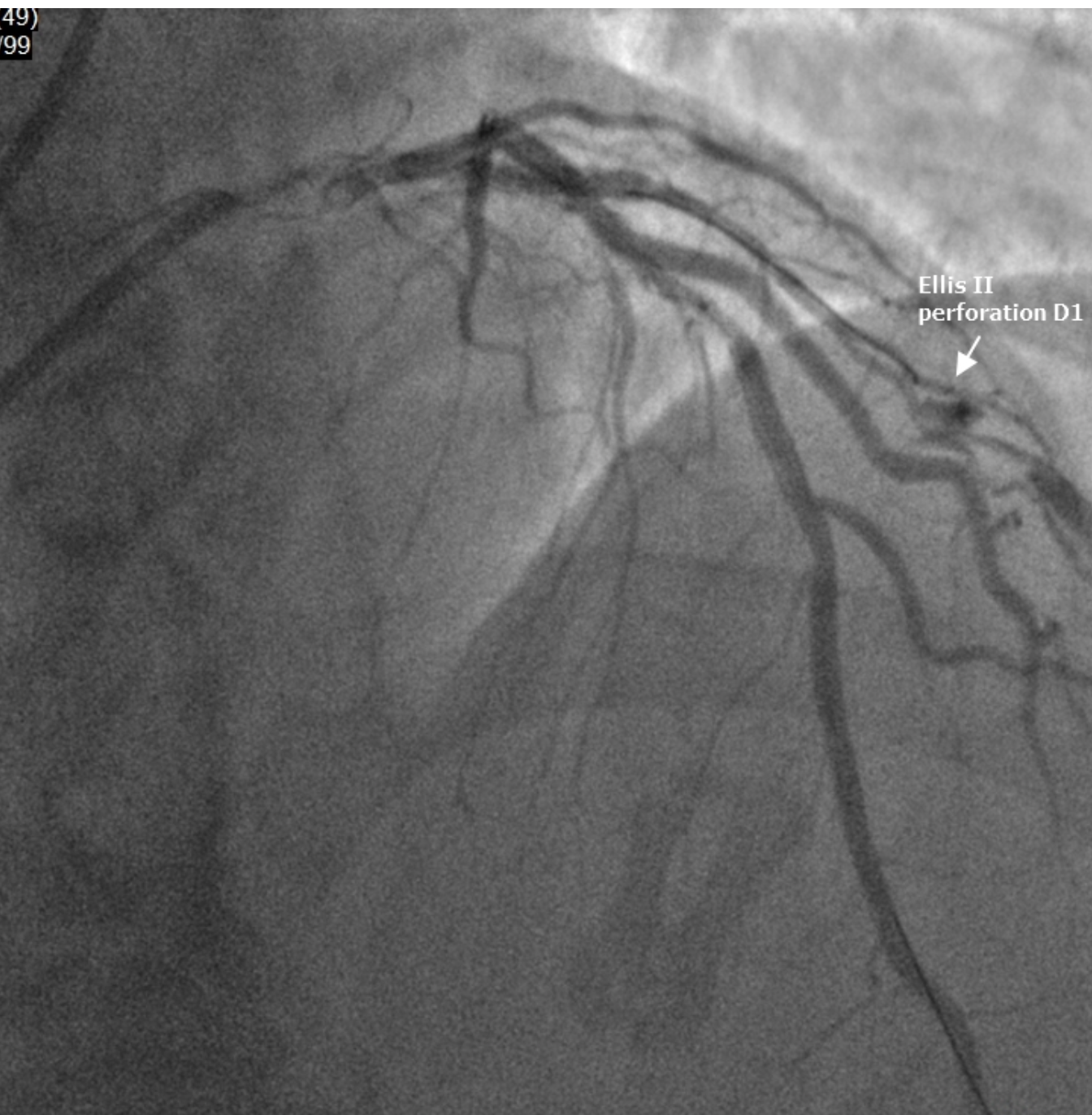
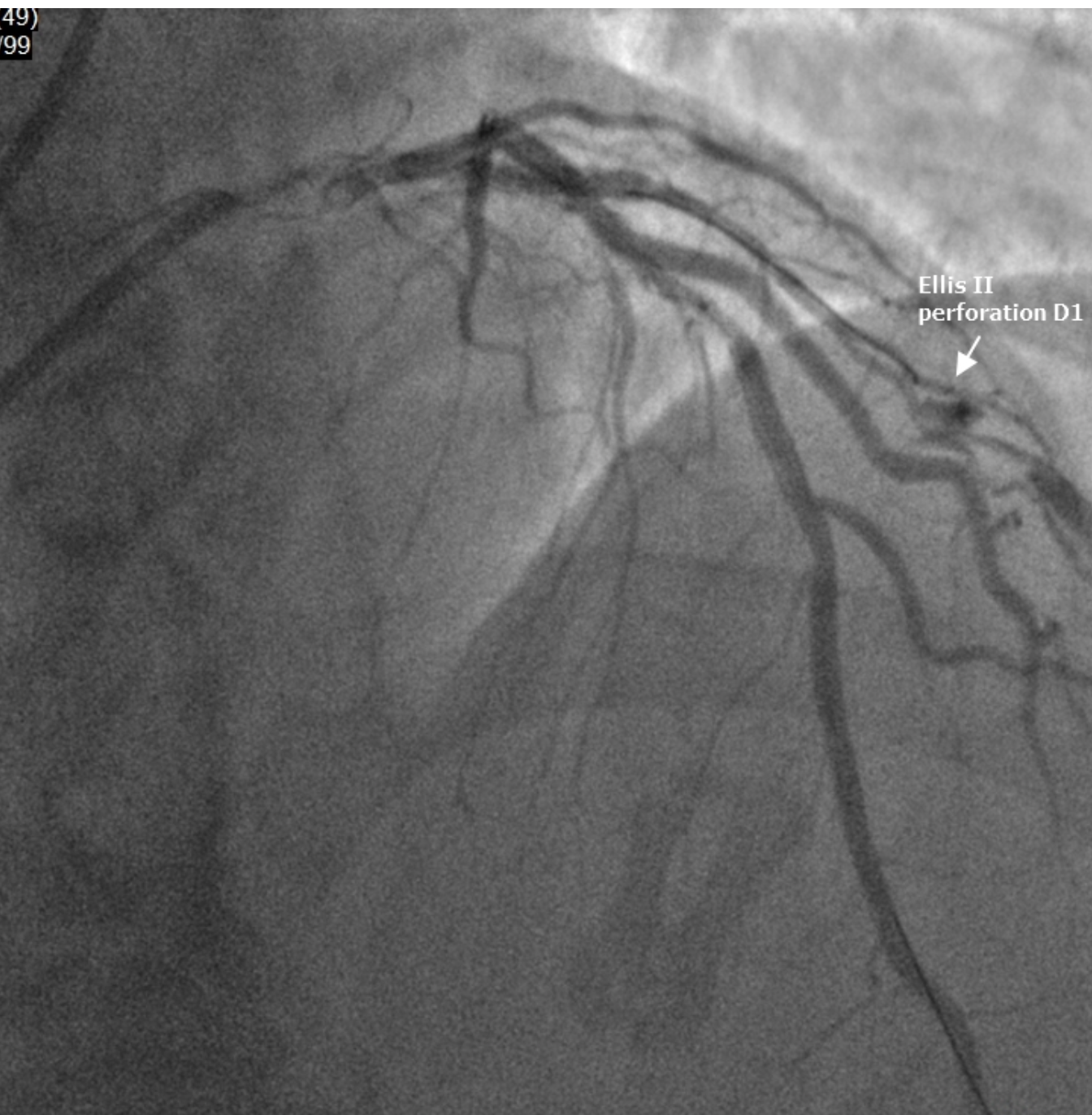
Given the retroflexed origin of the D1, we had difficulty wiring the D1. Attempts with a hydrophilic Sion Black wire and reverse wiring with a Sasuke dual-lumen catheter were all unsuccessful. We eventually wired the D1 with a Fielder XT-A with the aid of a re-cross microcatheter. Given the significant ostial D1 stenosis and difficulty in wiring D1, we planned for a 2-stent DK crush strategy to secure both the LAD/D1. We proceeded to deploy a 2.5x15mm Drug Eluting Stent (DES) in D1 extending into the LAD. Before crushing the stent, a recheck angiogram showed an Ellis 2 perforation in one of the branches of D1 (Figure 6). We immediately performed prolonged balloon inflation, but there was persistent contrast extravasation.
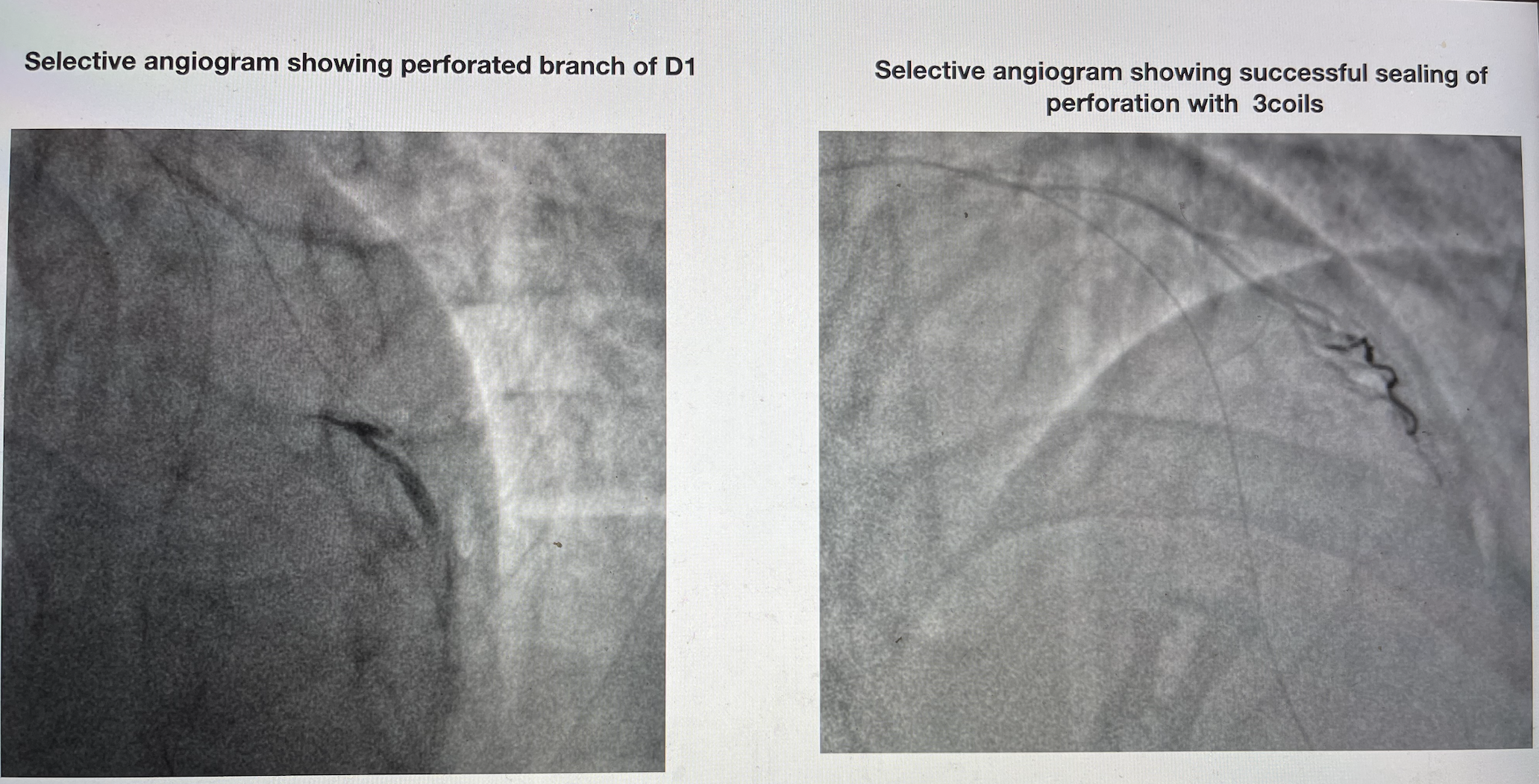
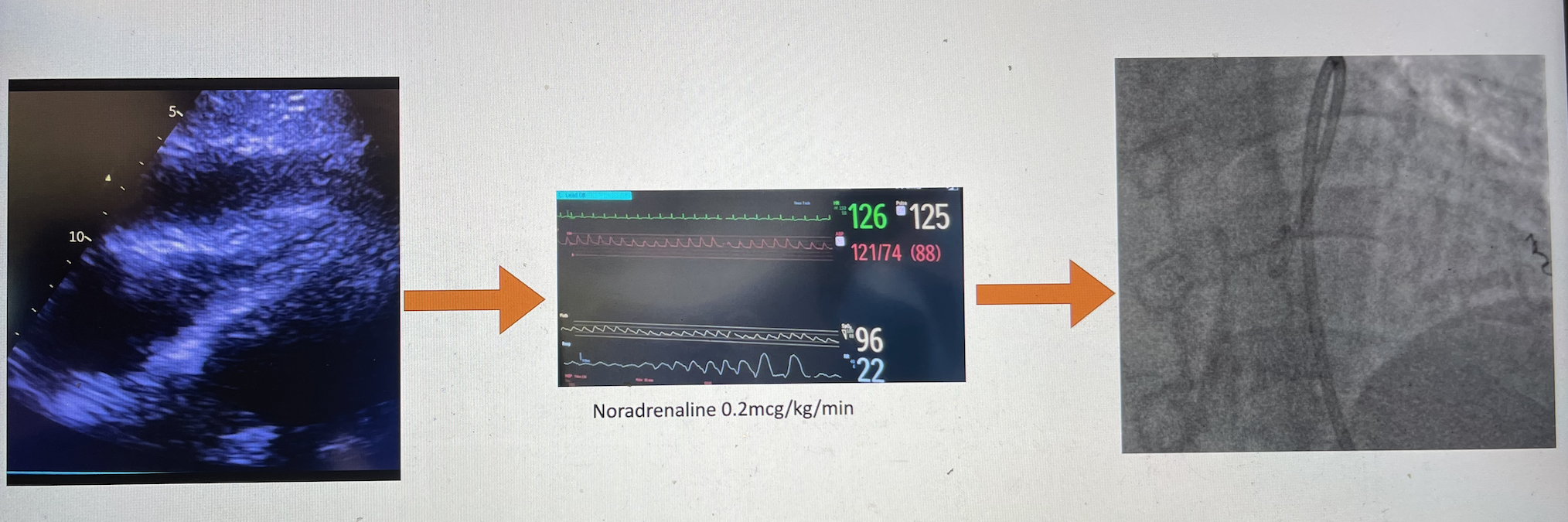
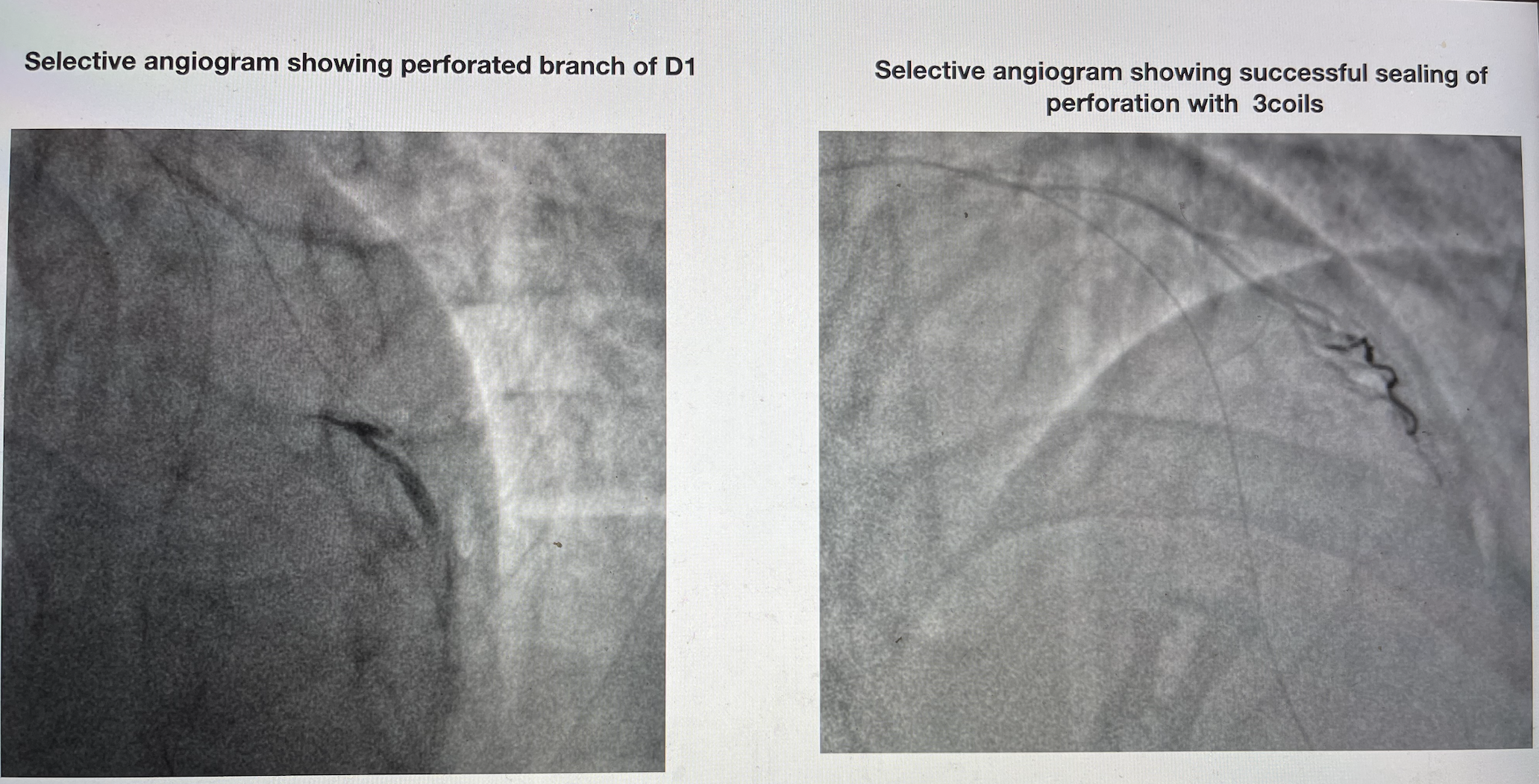
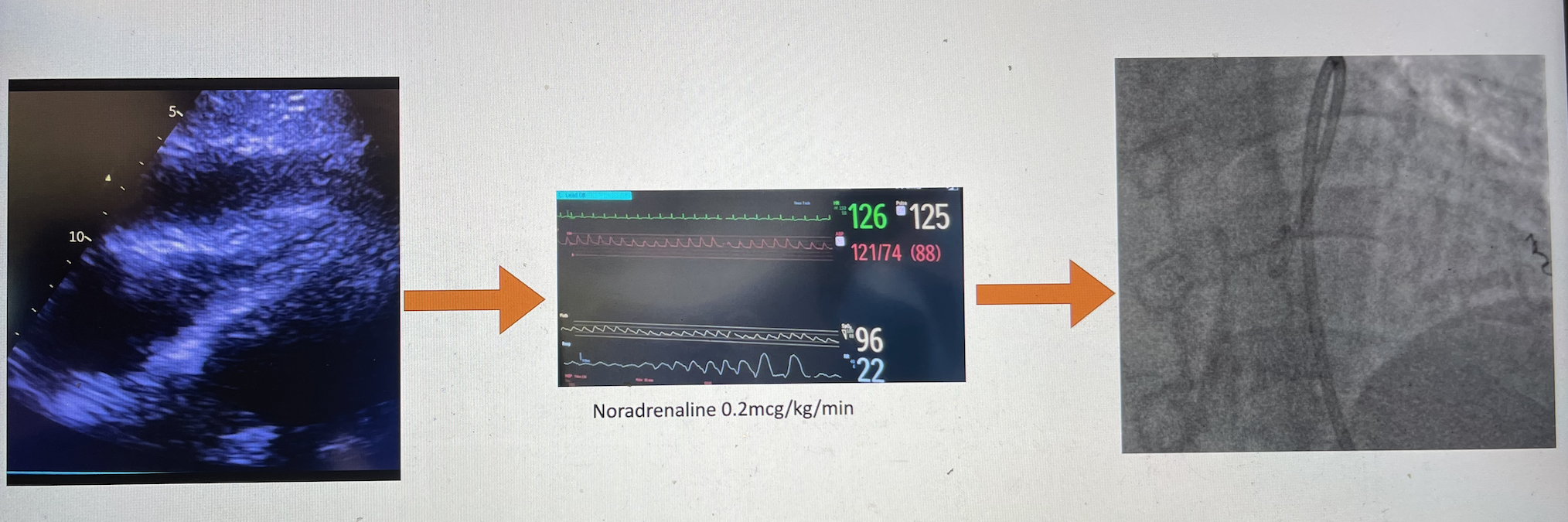
Bedside echocardiogram showed a small global pericardial effusion, and the patient remained hemodynamically stable. We managed to isolate the perforation to a branch of the D1 via selective angiograms with a microcatheter. We deployed 3 coils successfully (Figure 7), sealing the perforation. The pericardial effusion remained stable on echocardiogram.
We proceeded with the PCI as planned. However 2 hours after, the patient became hypotensive. Bedside echocardiogram showed a moderate pericardial effusion with evidence of tamponade. We performed emergency pericardiocentesis (Figure 8), with marked hemodynamic improvement. There was no further reaccumulation of pericardial effusion thereafter.
We proceeded with the PCI as planned. However 2 hours after, the patient became hypotensive. Bedside echocardiogram showed a moderate pericardial effusion with evidence of tamponade. We performed emergency pericardiocentesis (Figure 8), with marked hemodynamic improvement. There was no further reaccumulation of pericardial effusion thereafter.
Case Summary
The patient had presented for NSTEMI. He had undergone bifurcation stenting to the LAD/D1, which was complicated by diagonal perforation. We successfully sealed the perforation with 3 coils and managed to complete the procedure successfully. The patient subsequently developed pericardial tamponade, requiring pericardiocentesis, and was eventually discharged well..This case showcases varying techniques to overcome difficulties in wiring side branches and highlights the importance of guidewire management and the strategies to manage coronary perforations during PCI.

