Lots of interesting abstracts and cases were submitted for TCTAP 2024. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-026
No Lumen Lasts Forever.
By Yuen Hoong Phang, Abd Syukur Abdullah, Kai Soon Liew, Chai Yih Tan, Huan Yean Kang, Aditya Fahmi Prianda
Presenter
Yuen Hoong Phang
Authors
Yuen Hoong Phang1, Abd Syukur Abdullah1, Kai Soon Liew1, Chai Yih Tan1, Huan Yean Kang1, Aditya Fahmi Prianda2
Affiliation
Sultanah Bahiyah Hospital, Malaysia1, Hasna Medika Kuningan Heart Hospital, Indonesia2,
View Study Report
TCTAP C-026
Coronary - Complex PCI - Bifurcation
No Lumen Lasts Forever.
Yuen Hoong Phang1, Abd Syukur Abdullah1, Kai Soon Liew1, Chai Yih Tan1, Huan Yean Kang1, Aditya Fahmi Prianda2
Sultanah Bahiyah Hospital, Malaysia1, Hasna Medika Kuningan Heart Hospital, Indonesia2,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
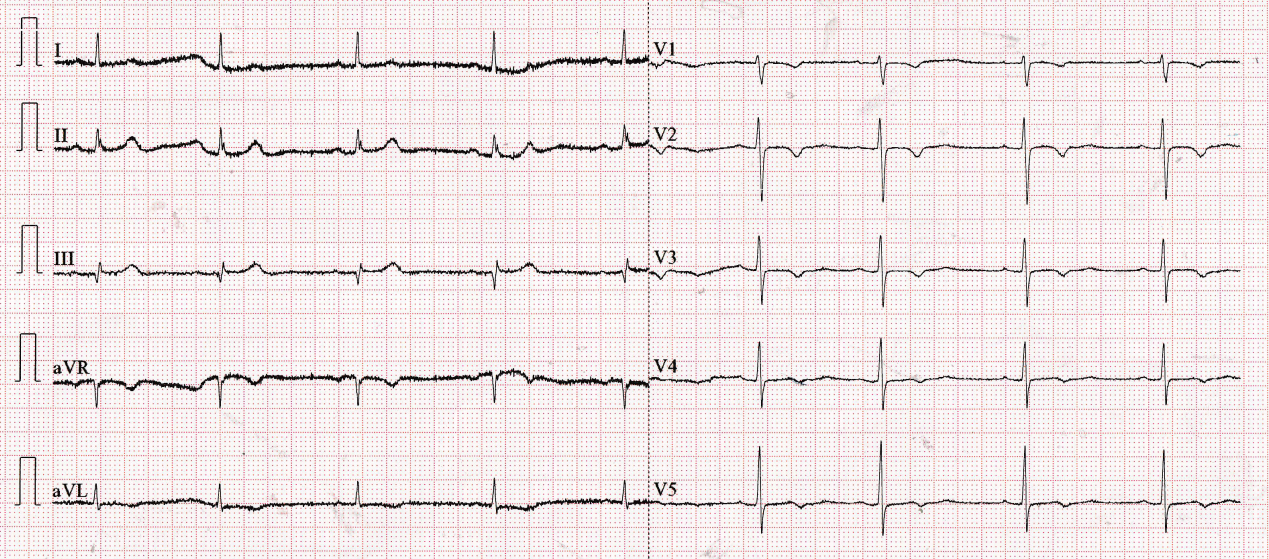
58 years old lady with underlying hypertension and recurrent angina was admitted for worsening angina. She was discharged a day back from a district hospital for similar complaint. Her blood pressure was elevated at 170/74, heart rate was 69 bpm, and saturating at 98% under room air. She was not in heart failure.
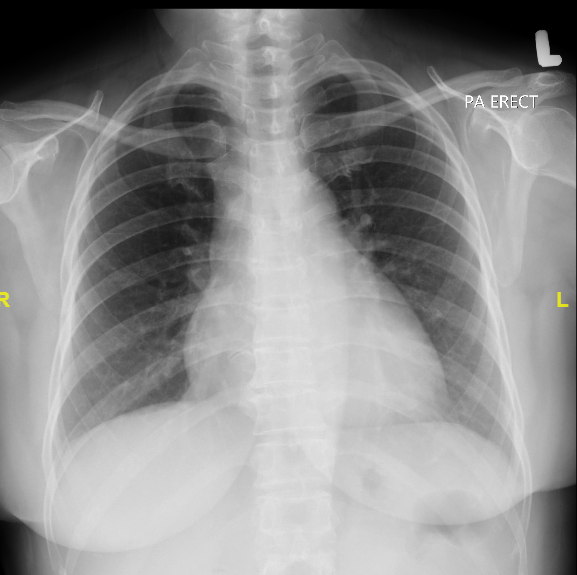
Relevant Test Results Prior to Catheterization
Her ECG showed a sinus rhythm with T inversion over V1-3. Her hemoglobin was 12.3, platelet counts was 352. Troponin and creatinine kinase were not elevated. Electrolytes were normal. Creatinine was 104umol/L. Bedside echocardiogram noted ejection fraction was preserved and valves were normal.
Relevant Catheterization Findings
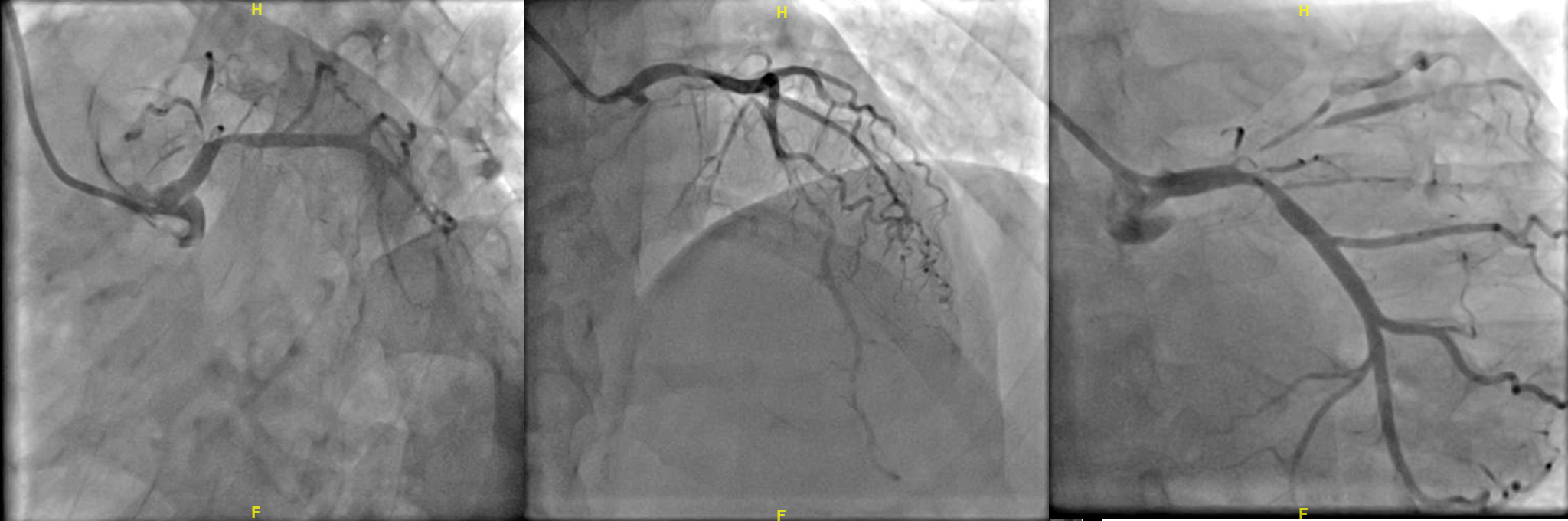
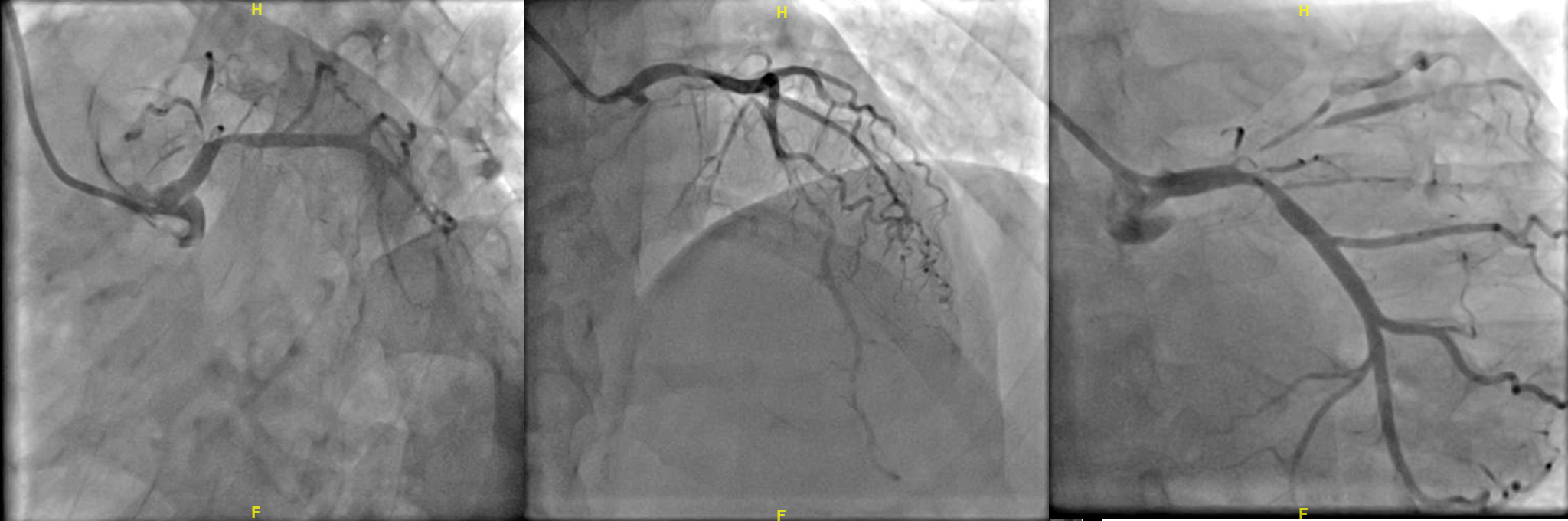
Coronary angiogram noted a co-dominant system with bifurcation lesion in involving left main to LAD and LCX with medina 0,1,1. RCA was normal and supplying collateral to LAD.


Interventional Management
Procedural Step
PCI was performed via right femoral approach with 7F EBU to LCA. LCX was wired with with Runthrough Floppy. Wiring of LAD was attempted with Sion Blue, but unsuccessful. Wire escalation was done to Fielder XTR and then to Gaia 1 which crossed the lesion. On wire crossing, there was lost of antegrade flow. Right radial approach with diagnostic JR catheter was used to visualise the LAD collateral which confirmed wire in true lumen. Lesion was predilated with SC Balloon 1.00x5mm @ 12-14atm, SC Balloon 1.5x15mm at 14atm, SC Balloon 2.0x20mm at 14 atm. Antegrade flow was restored. IVUS run was done to LAD to measure the vessel size, and lesion was predominantly fibrous plaque. IVUS run was done to LCX and noted ostium was diseased, but MLA was 7mm3. Hence, decision was made for provisional stenting. LAD was predilated with SC 3.0x20mm at 6-18atm. LM to LAD was stented with 3.5x38mm at 9atm( 3.50). As LCX flow was good, and MLA size was large, decision was made to remove the LCX wire prior to post dilatation. Stent was post dilated with stent balloon at 12atm (3.62mm) and noted patient became bradycardic and hypotensive. Noted plaque shift to LCX with Timi 1 flow. LCX was rewired with Runthrough floppy and was predilated with NC 3.00x20mm at 16atm(3.09). An TAP was performed with 3.5x18mm at 9atm(3.50). Kissing balloon was performed with NC Balloon 4.00x15mm(4.36) and stent balloon 3.5x18mm(3.55). POT was done with NC 4.5x8mm at 14atm (4.5). Final angiogram noted TIMI3 flow.






Case Summary
Bifurcation lesion requires continuous attention to both branches, despite initial relative sufficient IVUS lumen size. As the procedure continues, and especially post stenting, the risk of plaque shift is significant. The choice of left main stent with regards for expansion limit and number of connectors, skills for swift rewiring and bail out stenting are crucial skills in bifurcation procedure. In our case, the guard was down once decision not intervene the LCX post initial IVUS and the focus was mainly on the LAD. An initial two stents strategy would be a safer approach considering a diseased LCX ostium of a left dominant system. A TAP was done as a bail out and achieved a good outcome.

