Lots of interesting abstracts and cases were submitted for TCTAP 2024. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-052
I See, I Stream and I Conquer: A Case of IVUS Guided 3D Rewiring of RCA CTO-ISR
By Heng Shee Kim, Vicknesan Kulasingham, Hou Tee Lu, Mahadevan Gurudevan, Anek Kanoksilp
Presenter
Heng Shee Kim
Authors
Heng Shee Kim1, Vicknesan Kulasingham2, Hou Tee Lu1, Mahadevan Gurudevan3, Anek Kanoksilp4
Affiliation
Sultanah Aminah Hospital, Malaysia1, Ministry of Health Malaysia, Malaysia2, Sultanah Amina Hospital, Malaysia3, Central Chest Institute of Thailand, Thailand4,
View Study Report
TCTAP C-052
Coronary - Complex PCI - CTO
I See, I Stream and I Conquer: A Case of IVUS Guided 3D Rewiring of RCA CTO-ISR
Heng Shee Kim1, Vicknesan Kulasingham2, Hou Tee Lu1, Mahadevan Gurudevan3, Anek Kanoksilp4
Sultanah Aminah Hospital, Malaysia1, Ministry of Health Malaysia, Malaysia2, Sultanah Amina Hospital, Malaysia3, Central Chest Institute of Thailand, Thailand4,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
A 46-year-old smoker with hypertension and IHD history presented with typical angina and was diagnosed with NSTEMI. Physical examination was unremarkable. Inpatient CAG revealed two-vessel disease. PCI to LAD was performed, and a staged PCI for RCA CTO-ISR was planned a month later. However, he was readmitted a week later due to ADHF. Repeated CAG showed a patent LAD stent and similar RCA CTO-ISR. He was treated with optimal medical therapy and discharged with a plan to stage PCI to RCA later.
Relevant Test Results Prior to Catheterization
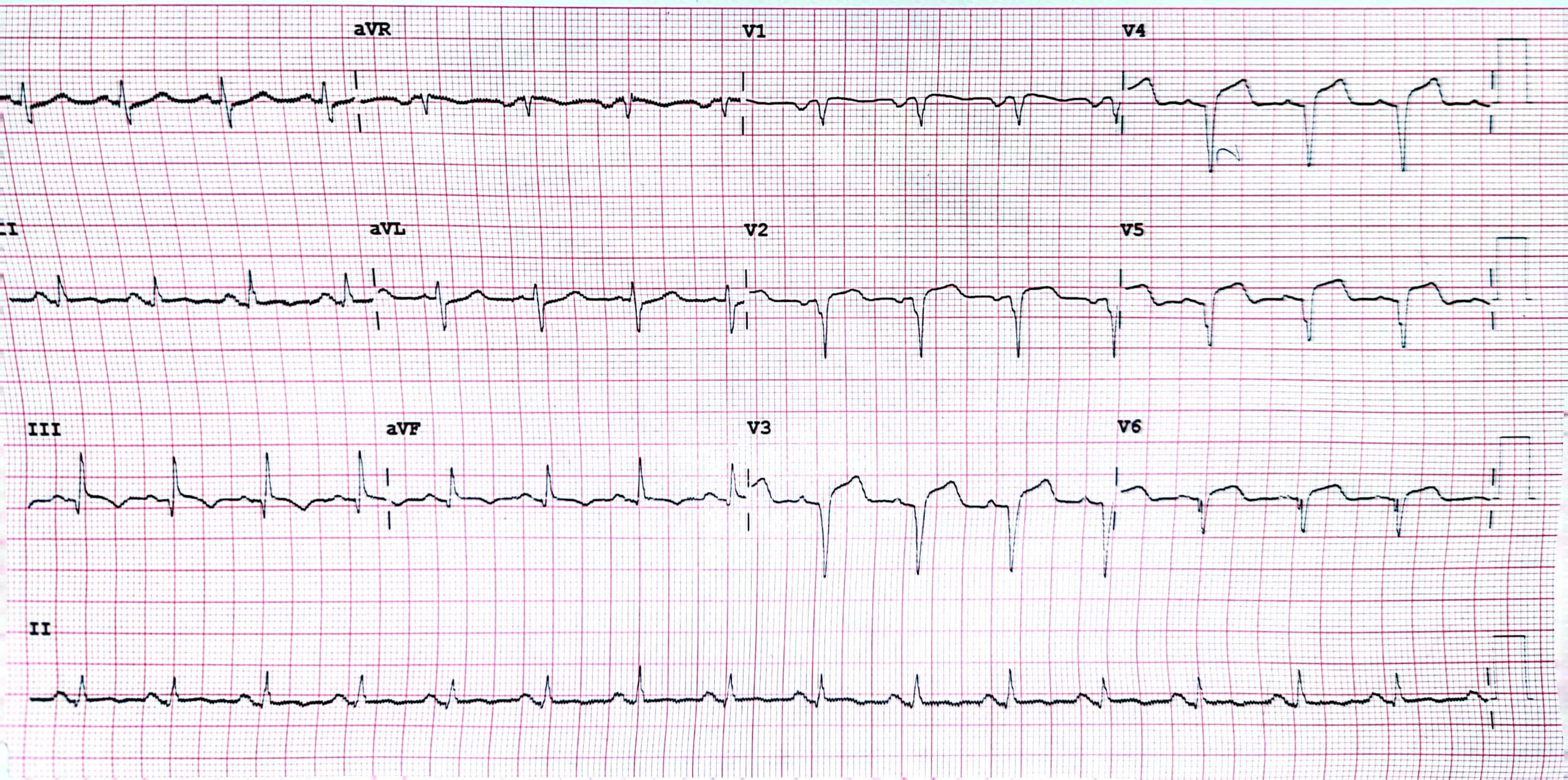
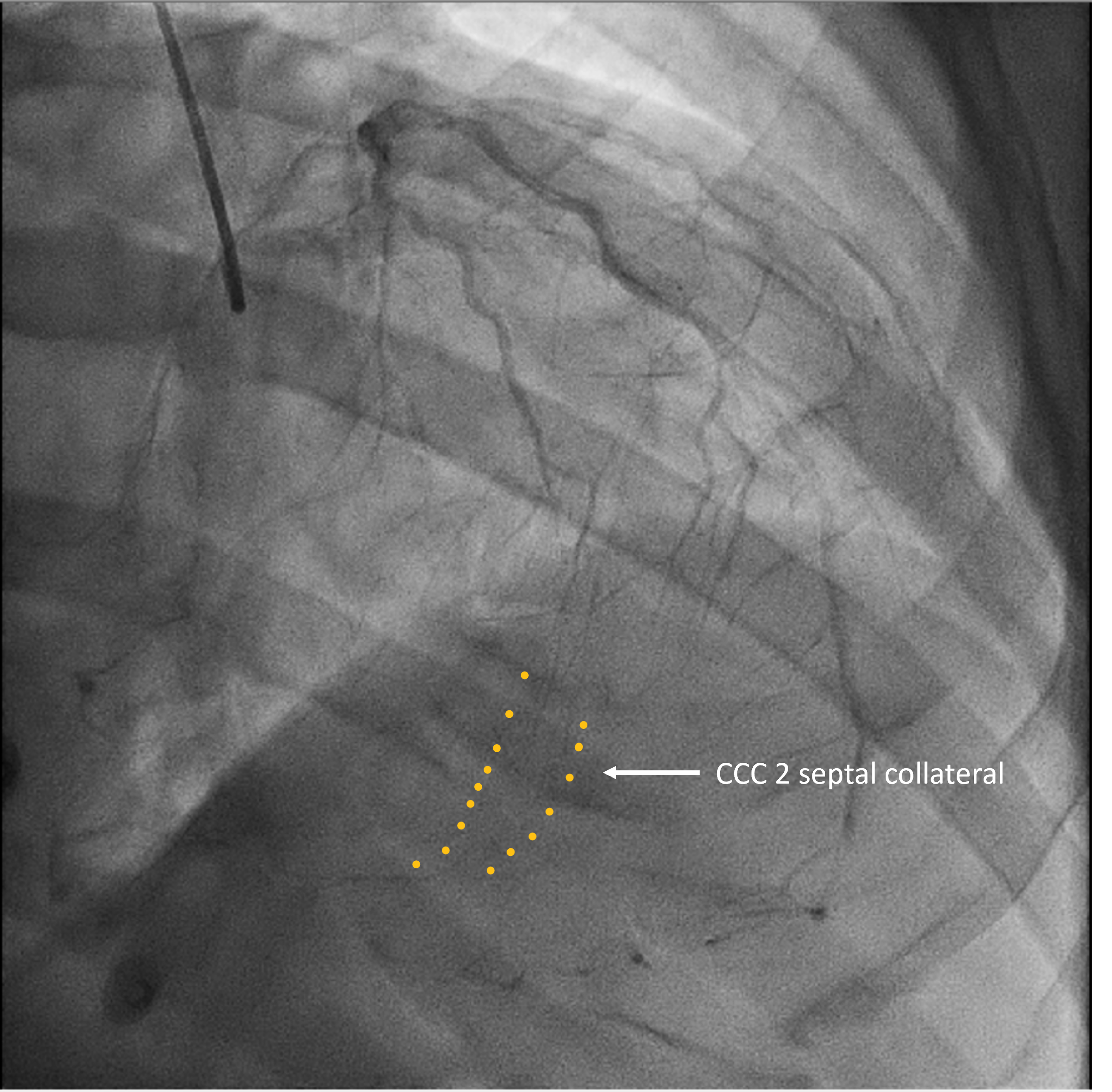
High-sensitive Troponin T during NSTEMI admission: 221.83 ng/LCreatinine 93 umol/L, estimated GFR 85 mL/min/1.73 m²Total cholesterol 3.7 mmol/L, LDL Cholesterol 2.2 mmol/L; HDL Cholesterol 0.7 mmol/L; Triglyceride 1.7 mmol/LHbA1c: 6.3 mmol/LECG: Q-wave lead V1 to V6Echocardiogram: Poor left ventricular ejection fraction of 30 - 35%, mildly dilated left ventricle, anteroseptal, anterior and apical hypokinesia, functional all valve with mild mitral regurgitation. Chest x-ray: Cardiomegaly
Relevant Catheterization Findings
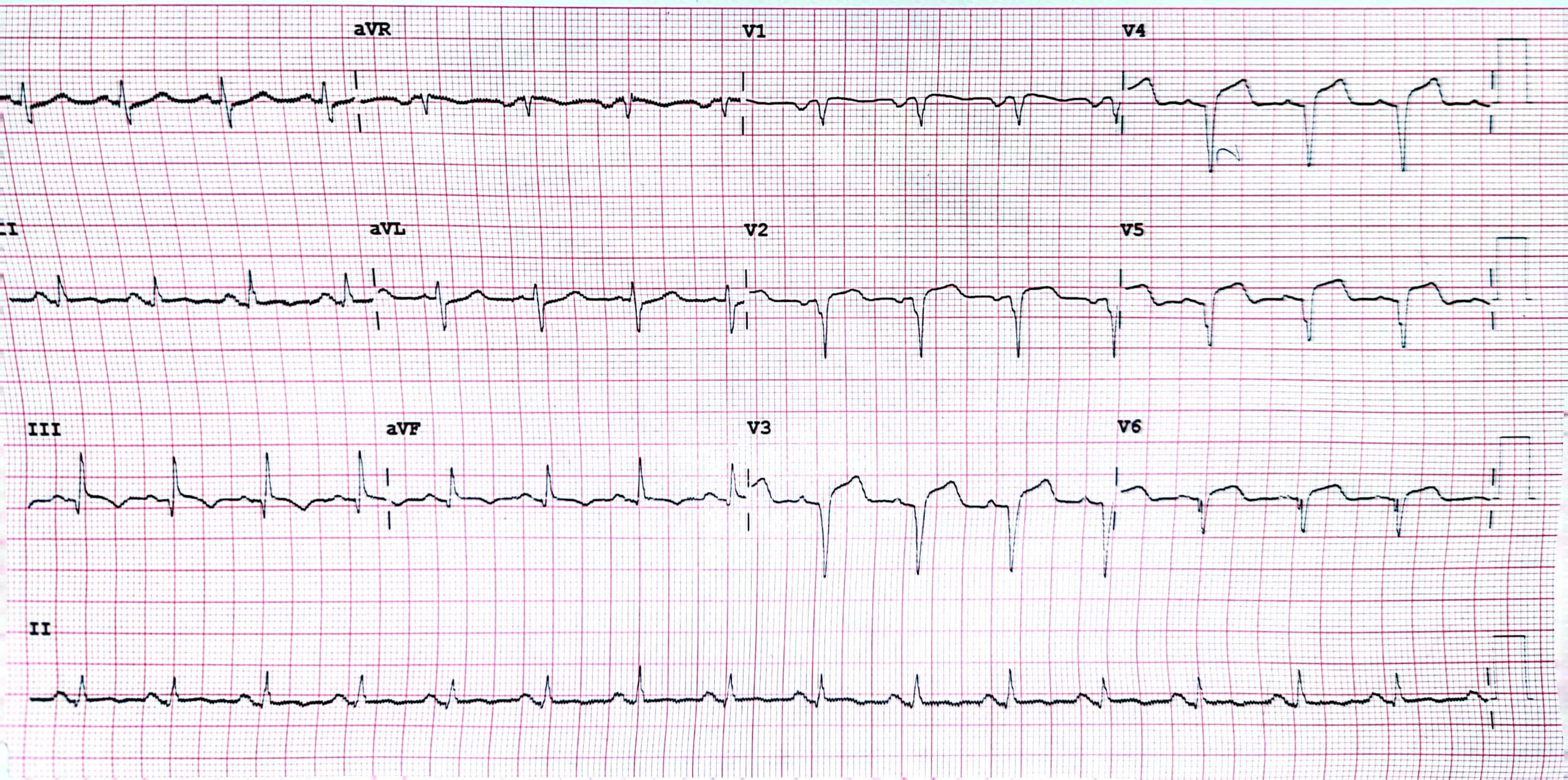
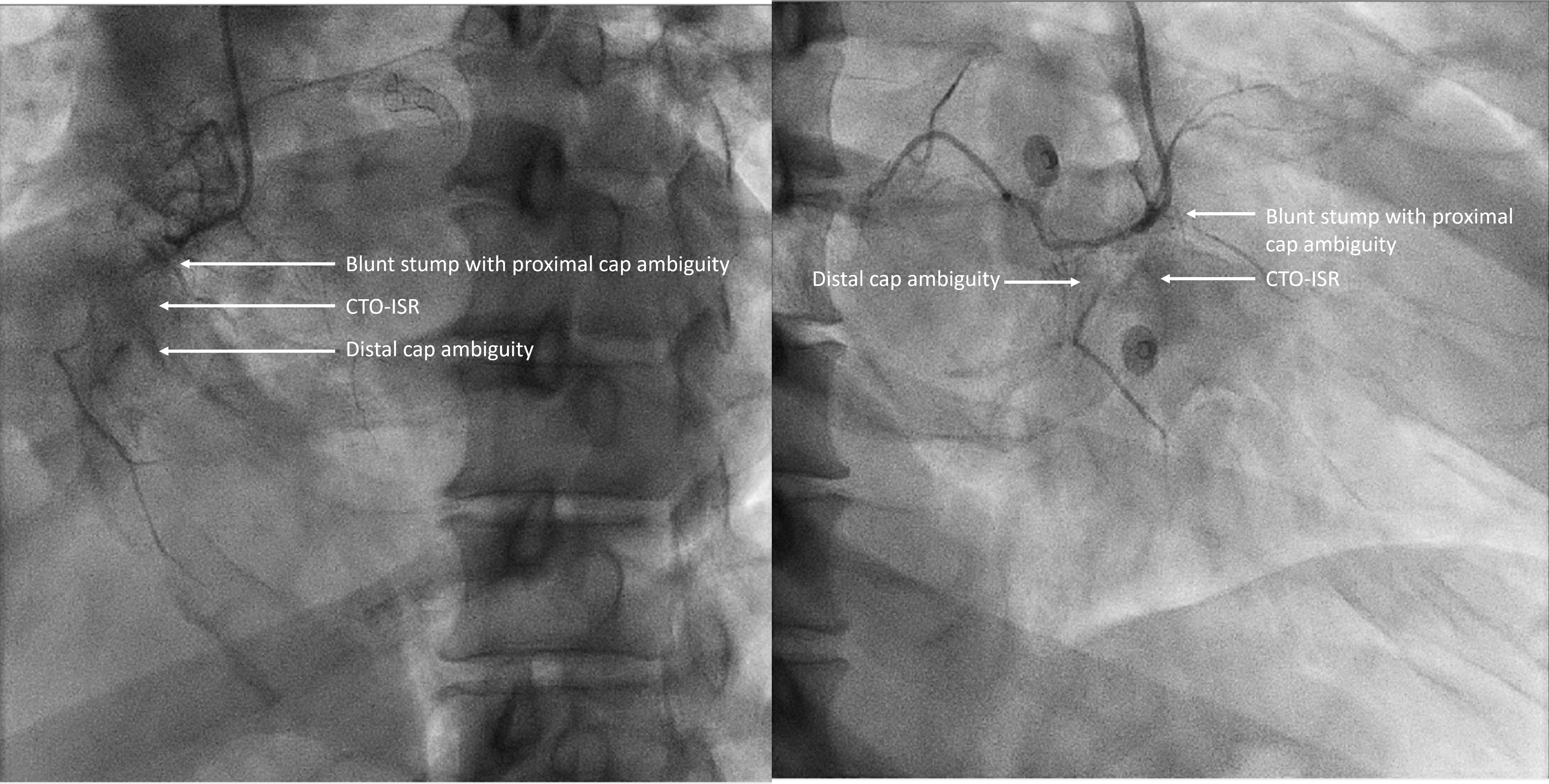
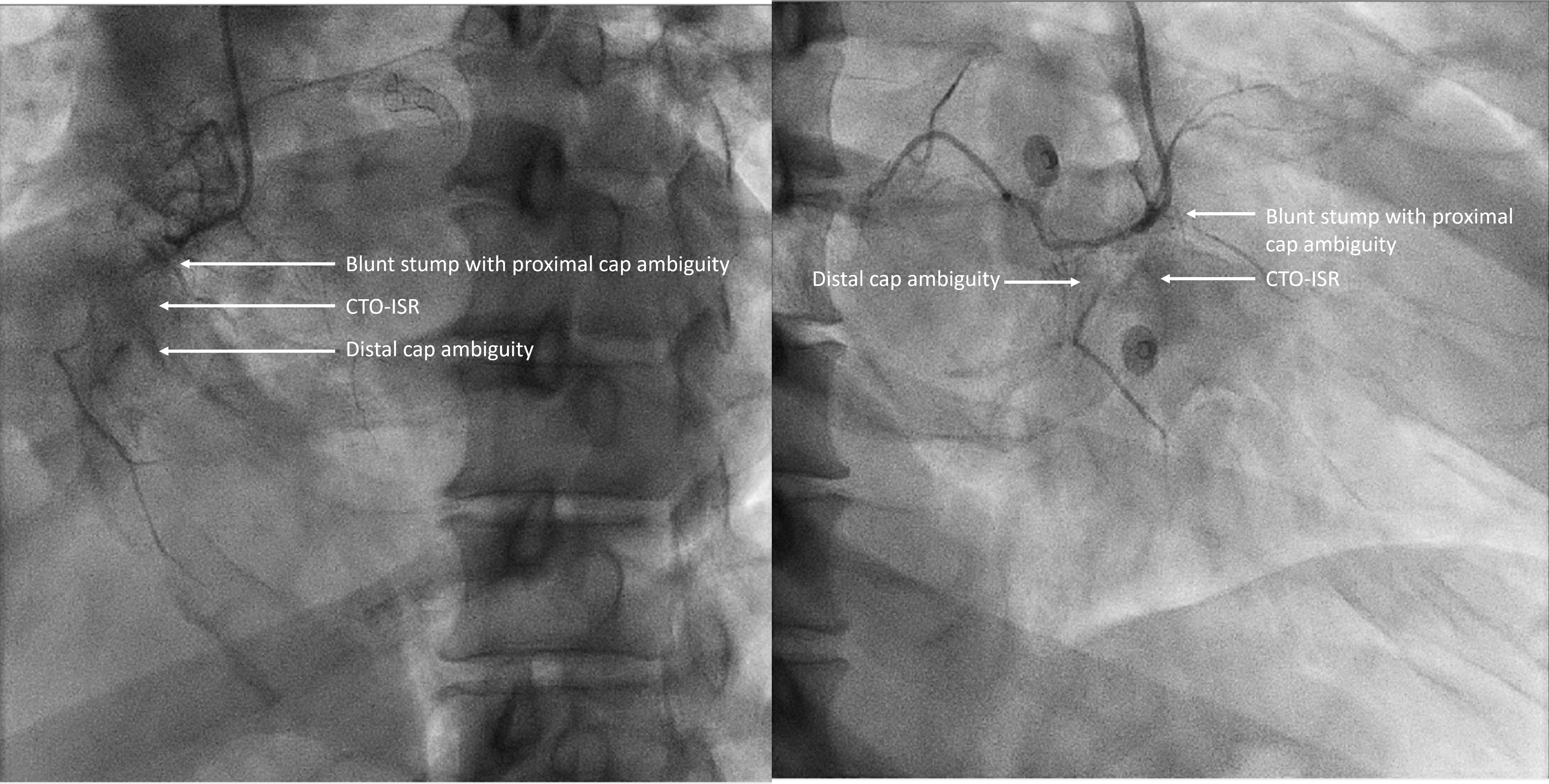
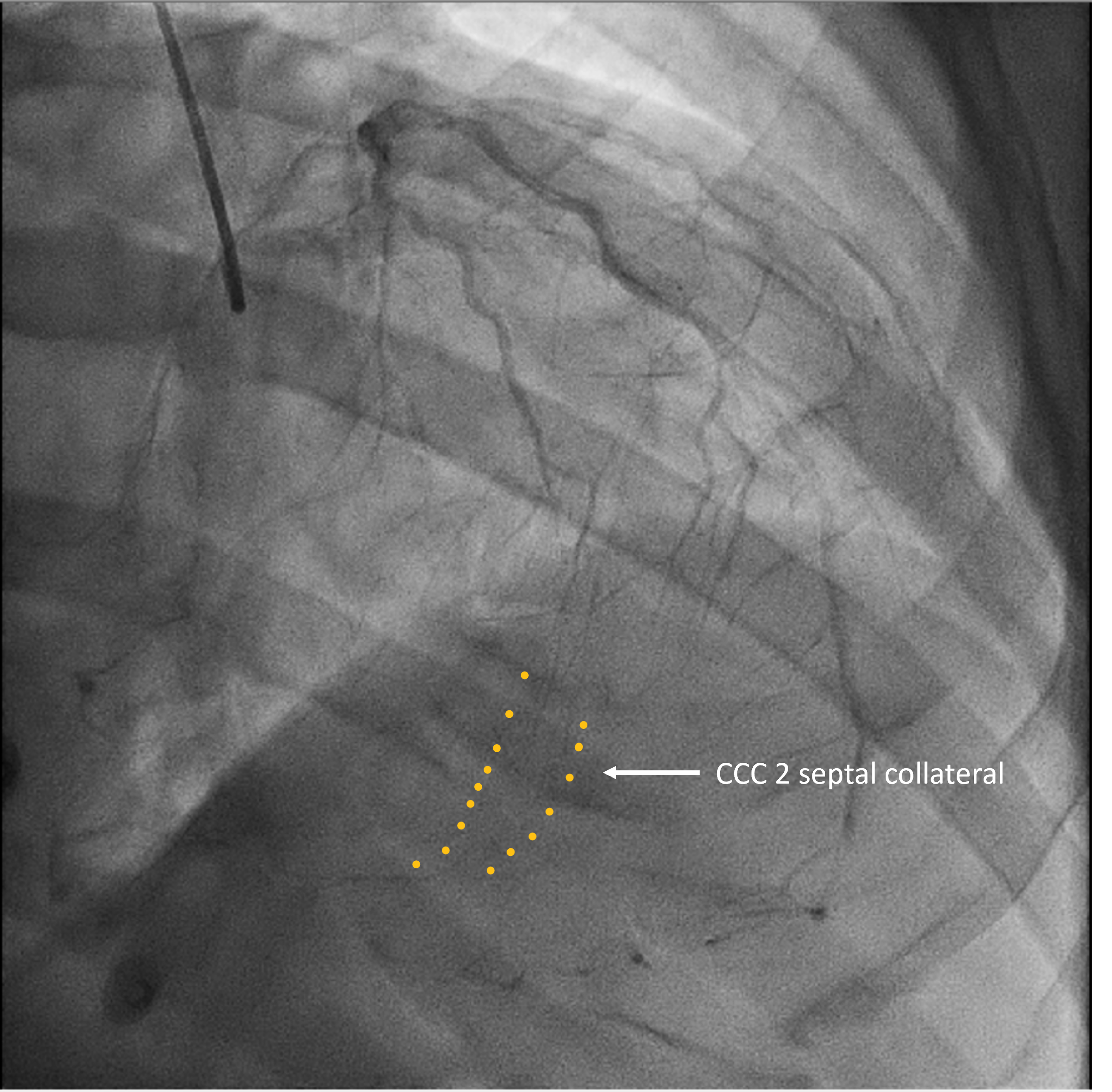
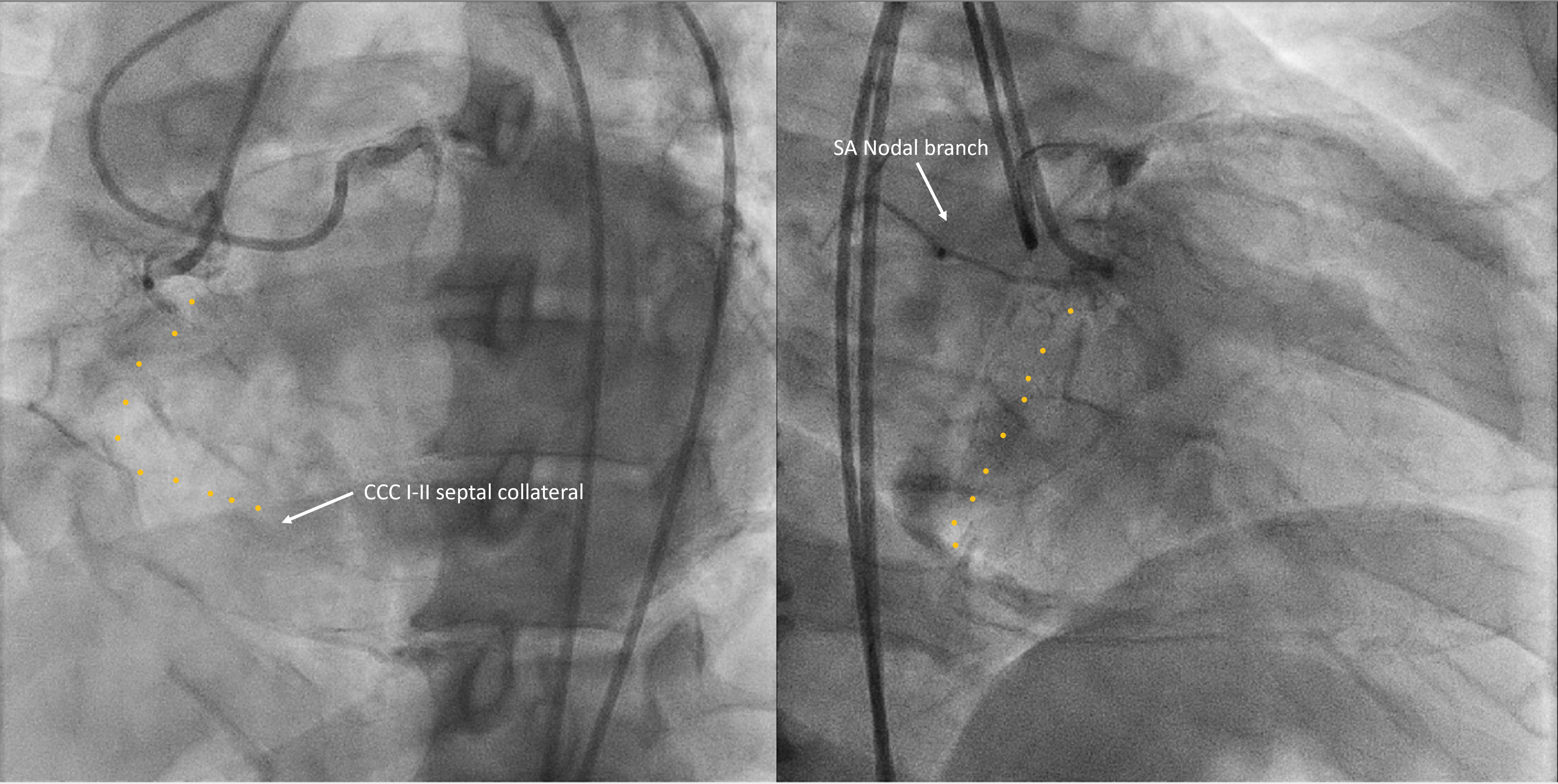
Initial CAG: 70% stenosis pLAD-mLAD and pRCA CTO-ISR. Bridging collateral from pRCA and retrograde collateral from septal artery.LAD lesion successfully treated with DES-PCI. Relook CAG one week later showed patent LAD stent with similar RCA finding.RCA CTO ISR Assessment: J-CTO Score 2; PROGRESS-CTO Score 3. pRCA – severe disease with blunt ambiguous proximal and distal cap. Collateral: antegrade CCC 0-1 bridging collateral to mRCA. Retrograde: CCC II septal collateral till RCA cruz.
Interventional Management
Procedural Step
Access & GC: Femoral 6F JL4, Femoral 7F JR 4.Strategy: Antegrade approach; if failed, consider bidirectional followed by 3D IVUS guided wiring.
Initial dual injection CAG showed CCC I-II poor septal collateral. Using dual lumen microcatheter DLC, wired to the SA branch, and anchored with a 1.5x10 balloon due to pRCA disease and unstable GC position. Started CTO wiring with Fielder XTA and Corsair Pro XS MC. After 10min of unsuccessful wiring, AWE to GAIA I which eventually crossed the CTO lesion. Predilated dRCA to pRCA with 1.0x10 before IVUS. However, only able to deliver the IVUS till the pRCA, which showed a large intraluminal size. Despite being prepared with 2.5x15 SC, only managed to pass the IVUS till the cruz of RCA. Unfortunately, IVUS showed a long segment of subintimal wiring.
Attempted retrograde approach but failed to identify a suitable interventional septal collateral. Opted to perform CTO tip detection using live IVUS with 3D wiring technique. Performed Slipstream technique using DLC, as part of the parallel wiring with live IVUS. Successfully wired the intraluminal/intraplaque with Conquest Pro wire, confirmed by IVUS, antegrade tip, and retrograde injection.
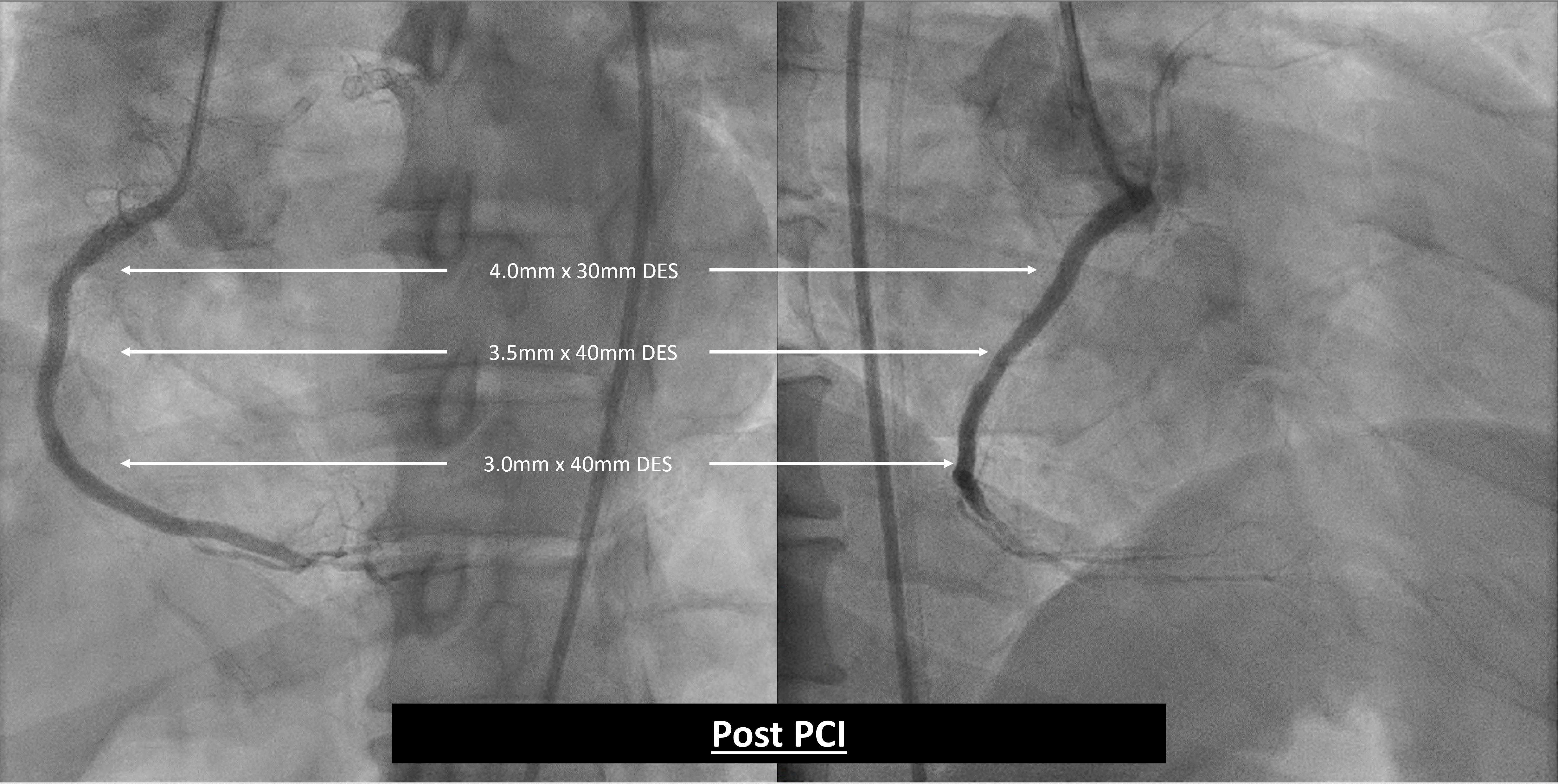
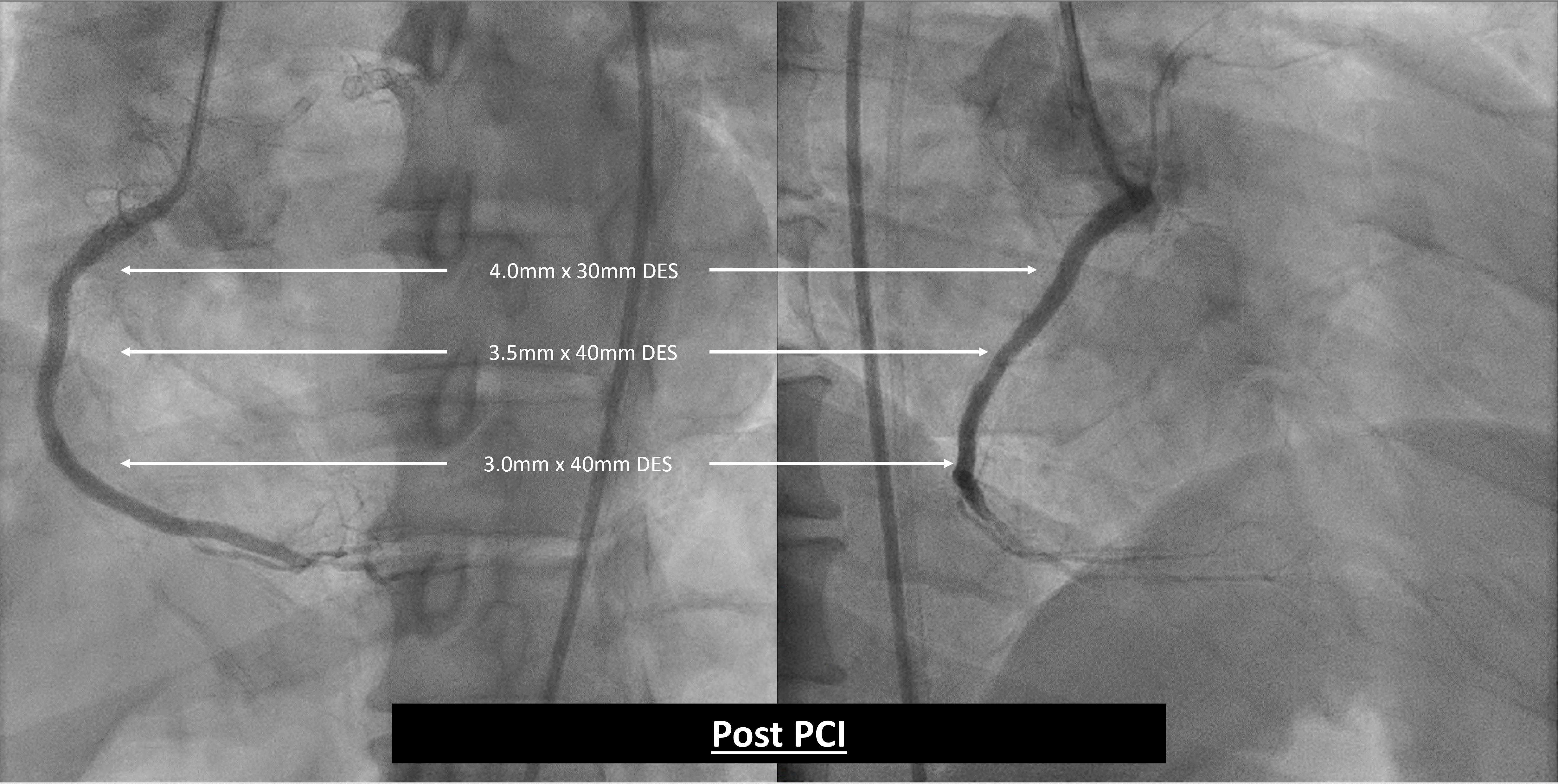
With guide extension, POBA from dRCA to pRCA using SC: 1.0x10, 1.5x10, 2.5x15, and 3.0x20. DRCA stented with 3.0x40, mRCA with 3.5x40, and pRCA with 4.0x30 DES up to the ostial successfully. Stent post dilated up to 4.2mm. Post PCI, angiographically and IVUS showed good results with no complications.
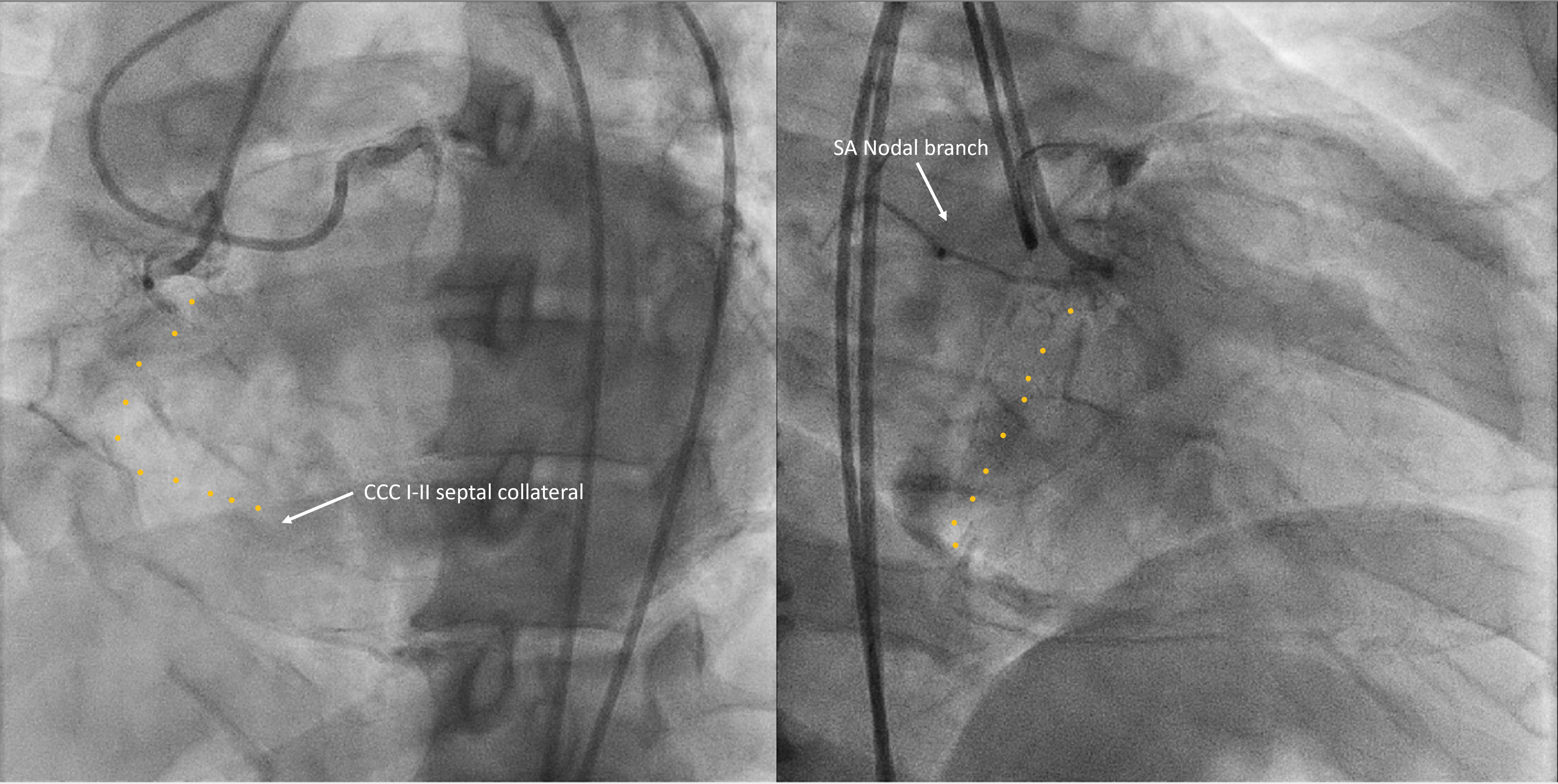

Initial dual injection CAG showed CCC I-II poor septal collateral. Using dual lumen microcatheter DLC, wired to the SA branch, and anchored with a 1.5x10 balloon due to pRCA disease and unstable GC position. Started CTO wiring with Fielder XTA and Corsair Pro XS MC. After 10min of unsuccessful wiring, AWE to GAIA I which eventually crossed the CTO lesion. Predilated dRCA to pRCA with 1.0x10 before IVUS. However, only able to deliver the IVUS till the pRCA, which showed a large intraluminal size. Despite being prepared with 2.5x15 SC, only managed to pass the IVUS till the cruz of RCA. Unfortunately, IVUS showed a long segment of subintimal wiring.
Attempted retrograde approach but failed to identify a suitable interventional septal collateral. Opted to perform CTO tip detection using live IVUS with 3D wiring technique. Performed Slipstream technique using DLC, as part of the parallel wiring with live IVUS. Successfully wired the intraluminal/intraplaque with Conquest Pro wire, confirmed by IVUS, antegrade tip, and retrograde injection.
With guide extension, POBA from dRCA to pRCA using SC: 1.0x10, 1.5x10, 2.5x15, and 3.0x20. DRCA stented with 3.0x40, mRCA with 3.5x40, and pRCA with 4.0x30 DES up to the ostial successfully. Stent post dilated up to 4.2mm. Post PCI, angiographically and IVUS showed good results with no complications.

Case Summary
Overcoming challenges of ambiguous caps, subintimal wiring, and poor retrograde collateral, the procedure utilized a unique combination of Slipstream technique, live IVUS, and DLC for CTO tip detection using live IVUS with 3D wiring technique. Despite initial setbacks, successful antegrade wiring with GAIA I and subsequent stenting from dRCA to pRCA achieved optimal results, demonstrating the efficacy of this tailored approach in a complex scenario.

