Lots of interesting abstracts and cases were submitted for TCTAP 2024. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-005
A Case Report: Young MI Patient With Spontaneous Coronary Artery Dissection in Both Lad and Rca Artery: What Should We Do?
By Quan Manh Nguyen, Tung Ngo
Presenter
Tung Ngo
Authors
Quan Manh Nguyen1, Tung Ngo1
Affiliation
Vietnam National Heart Institute, Vietnam1,
View Study Report
TCTAP C-005
Coronary - ACS/AMI
A Case Report: Young MI Patient With Spontaneous Coronary Artery Dissection in Both Lad and Rca Artery: What Should We Do?
Quan Manh Nguyen1, Tung Ngo1
Vietnam National Heart Institute, Vietnam1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
Male patient, 35 years old
Relevant Test Results Prior to Catheterization
Bedside emergency echocardiography:


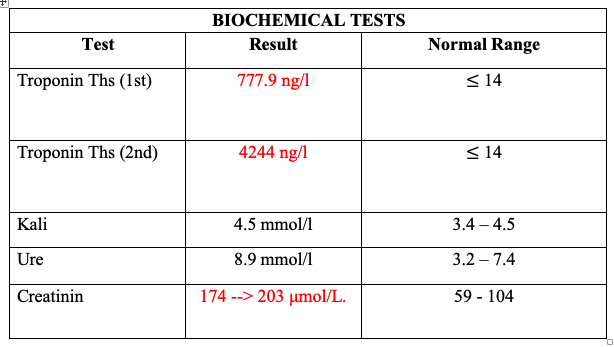


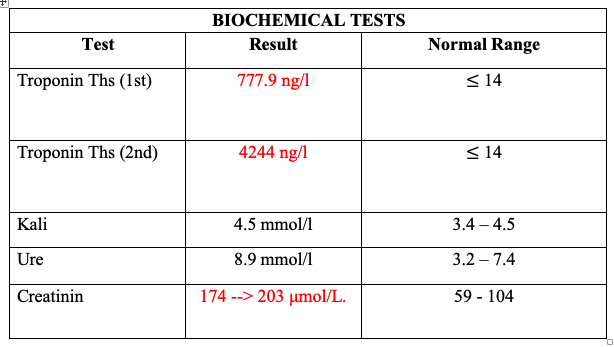
Relevant Catheterization Findings
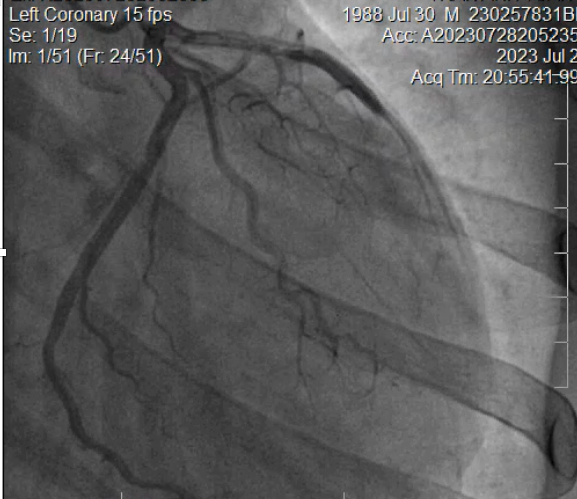
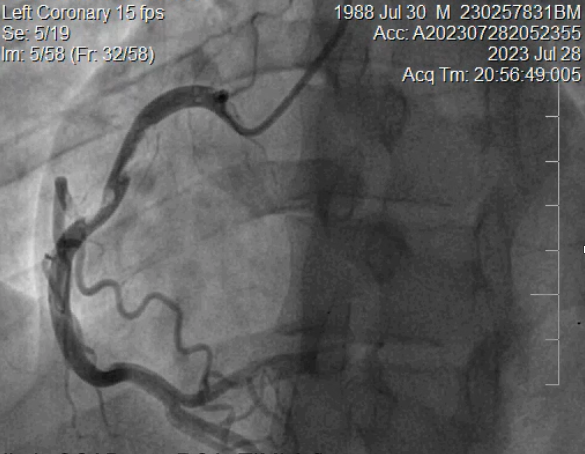
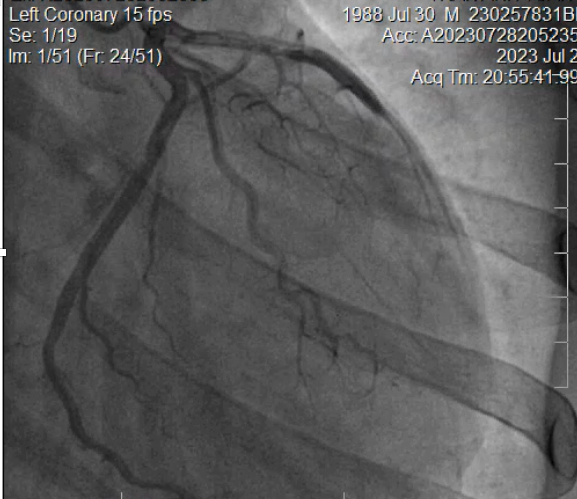
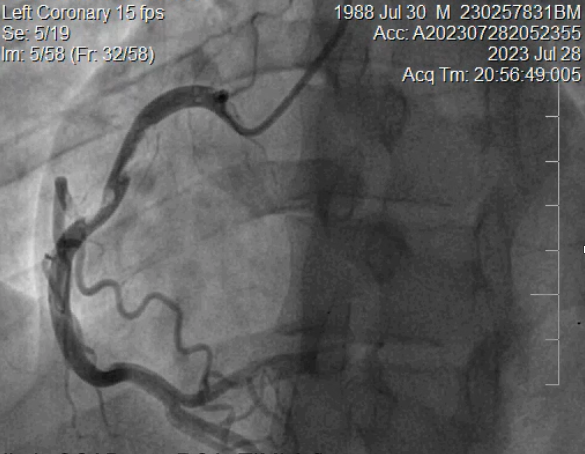
Angiogram: SCAD type 1 at p-LAD caused TIMI 1 flow, Lcx seems normal. Likely SCAD at p-RCA, TIMI 3 flow. Maybe Thombus?
Interventional Management
Procedural Step
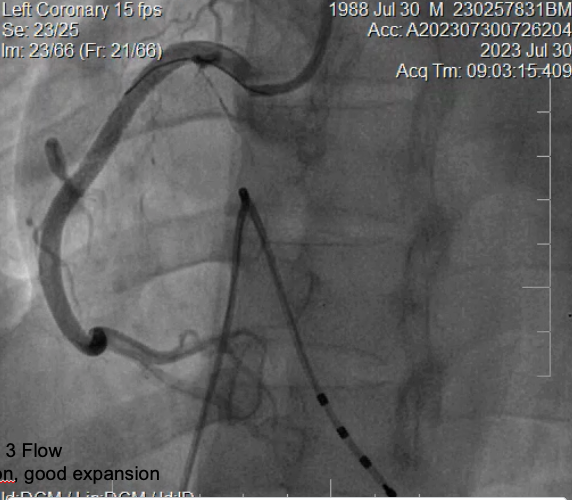
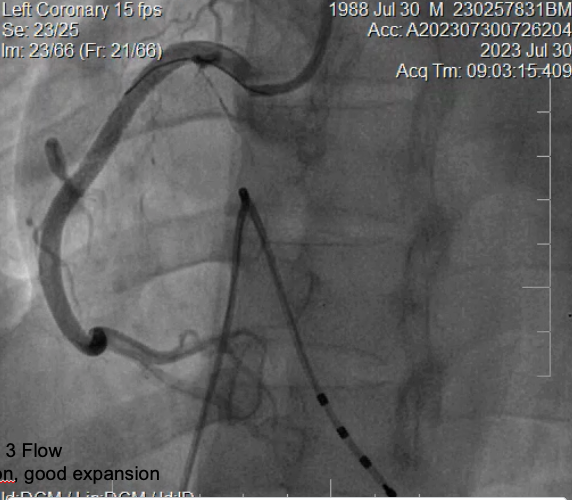
EBU 3.5. Right radial artery. wire: BMW Runthrough. we perform slightly pre-dilate the deployed stent at LAD. Result: Good LAD TIMI Flow STOP. We plan to perform 2nd coronary angiography after a few days. Right after PCI: Stable hemodynamic, symptoms relieved. After 48 hours: recurrent Chest pain, and dizziness. ECG: BAV III. Indications: Temporary pacemaker + Re- angiography. Result: LAD stent is still good. The RCA vessel wall is more 'solid' and the flow is still good ( better than 2 days ago) but the vessel wall is not as smooth then we performed IVUSIVUS image: RCA vessel wall hematoma + Ruptured atherosclerotic plaque --> PCI RCA with DES 4.0X 38 mm, TIMI 3 Flow. IVUS after stenting: No dissection, no malposition, good expansion. After 2nd PCI: Relieved chest pain. Heart rate is 90 beats/minute. Blood pressure 120/80 mmHg (Noradrenaline 0.1 ug/kg/pg).The patient is stable and discharged after 5 days
Case Summary
1. SCAD is rare but the incidence tends to be increased and dissection of multiple vessels occurs in 9-23%

