Lots of interesting abstracts and cases were submitted for TCTAP 2024. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-094
The Last Hope
By Choutchung Tinakorn Na Ayudhya, Vorarit Lertsuwunseri
Presenter
Choutchung Tinakorn Na Ayudhya
Authors
Choutchung Tinakorn Na Ayudhya1, Vorarit Lertsuwunseri1
Affiliation
King Chulalongkorn Memorial Hospital, Thailand1,
View Study Report
TCTAP C-094
Coronary - Complex PCI - Left main
The Last Hope
Choutchung Tinakorn Na Ayudhya1, Vorarit Lertsuwunseri1
King Chulalongkorn Memorial Hospital, Thailand1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
A 76 year-old-man presented with typical chest pain while on hemodialysis for 1 week. His underlying diseases were ESRD s/p HD, HT, DLP, paroxysmal AF and IHD s/p multiple episodes of PCI with DES at LM-proximal LAD, mid LAD and mid RCA then develop severe ISR so patient underwent CABG x 2 times in 2021 and redo in 2022 due to graft failure.


Relevant Test Results Prior to Catheterization
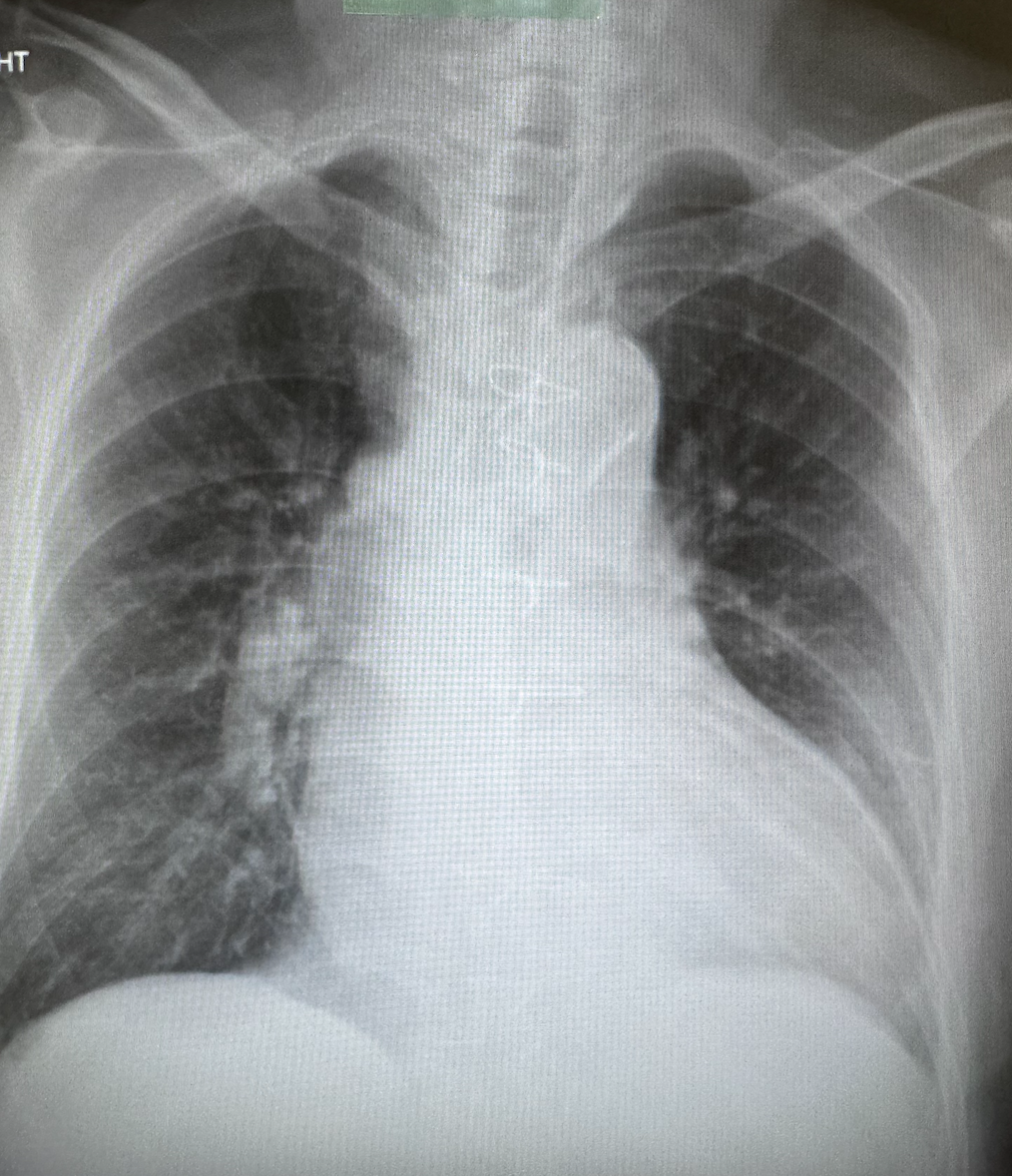
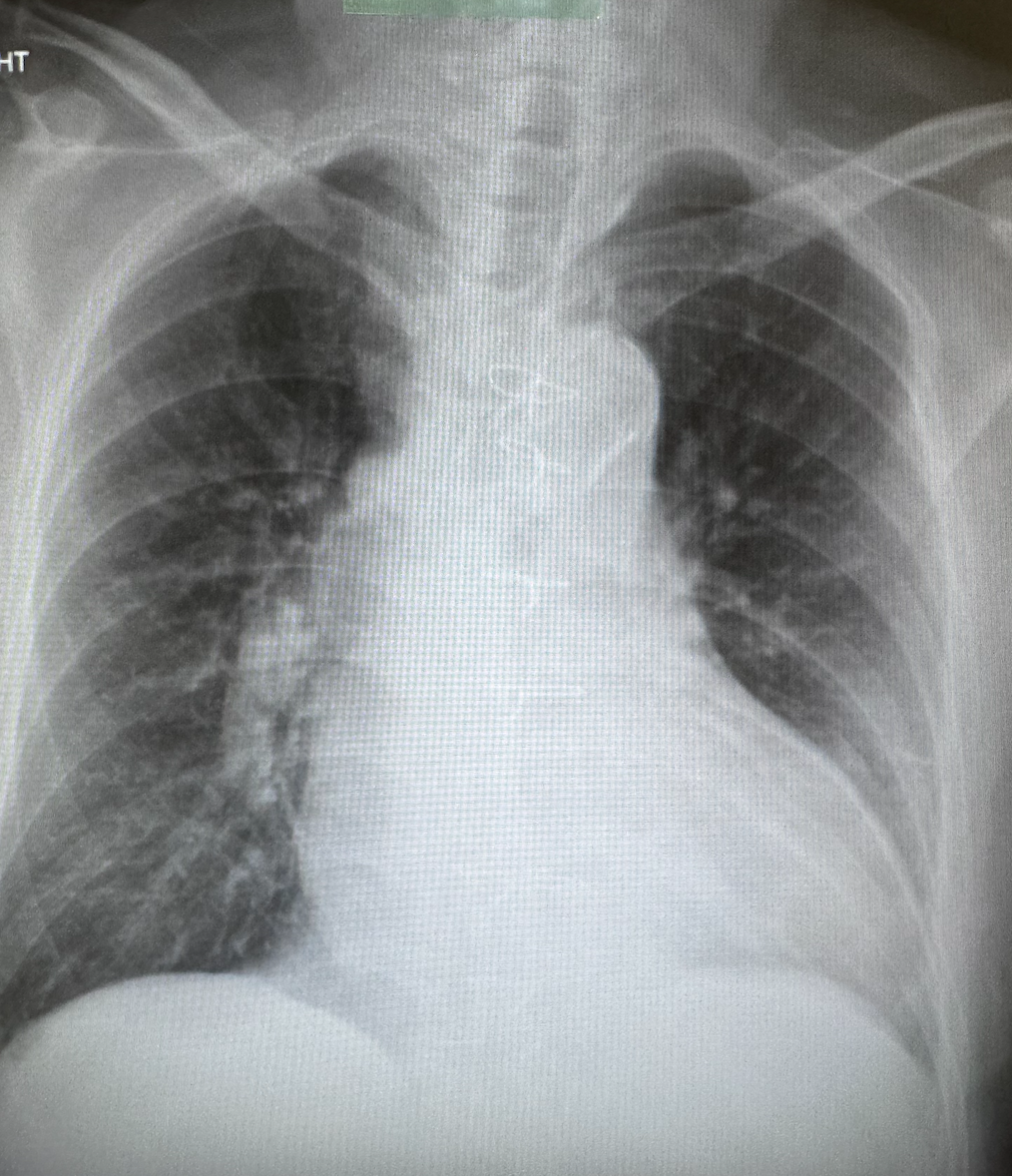
CXR showed cardiomegaly without cephalization or pulmonary congestionEKG showed sinus tachycardia rate 70/min LAD LVH with horizontal st depression in V5-V6LAB hsTnI = 20.3 ng/L NT-pro BNP > 35,000 pg/ml Hct 32.4 Bun 66 Cr 12.6Echo dilated LV size with severely impaired LV systolic function LVEF = 26% by Biplane with RWMAs hypokinesia in anterior, septal and inferior wall from bas to apex, no evidence of LV thrombus, no pericardial effusion
Relevant Catheterization Findings
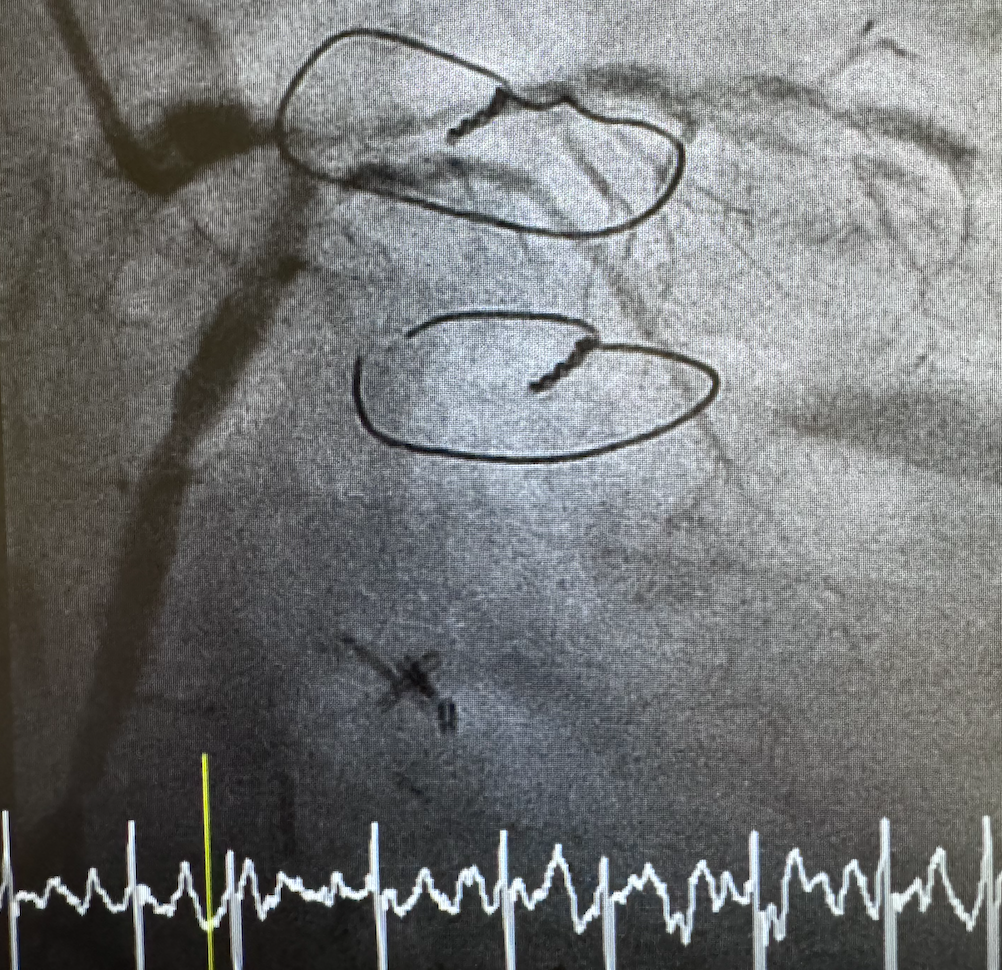
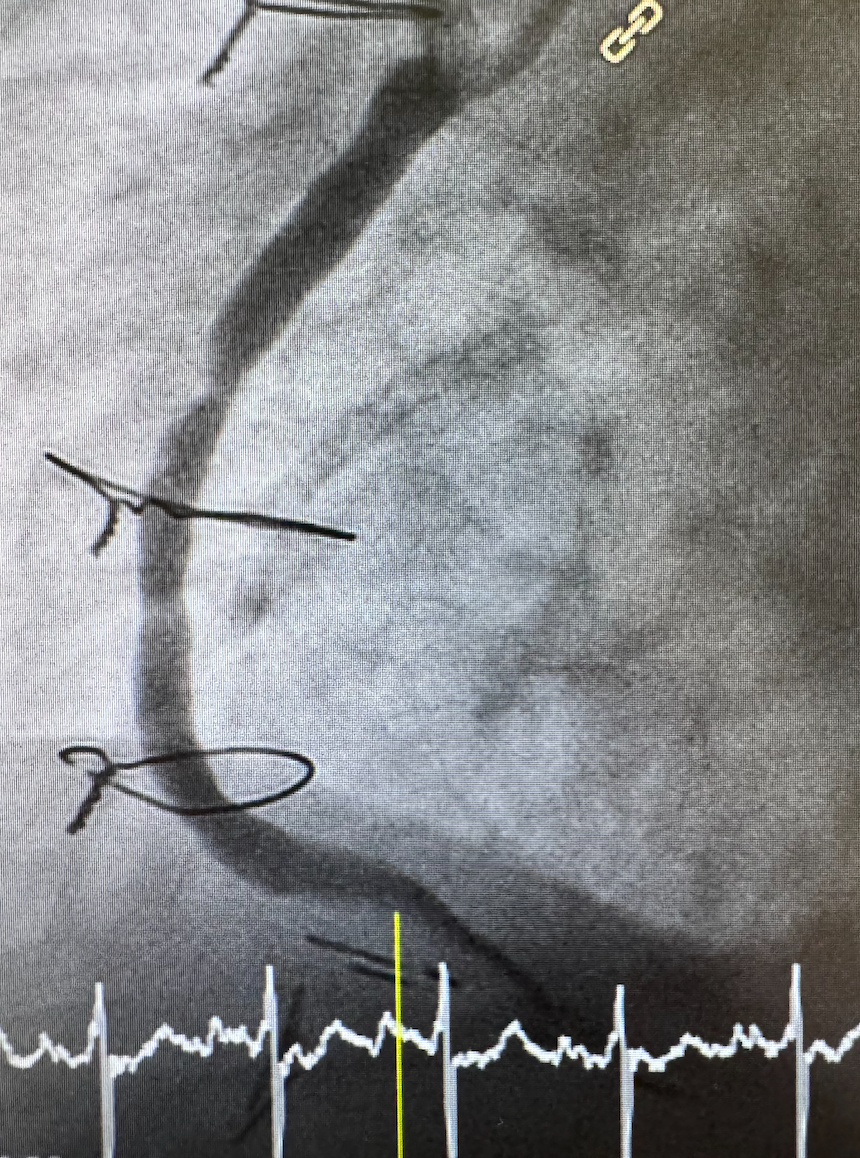
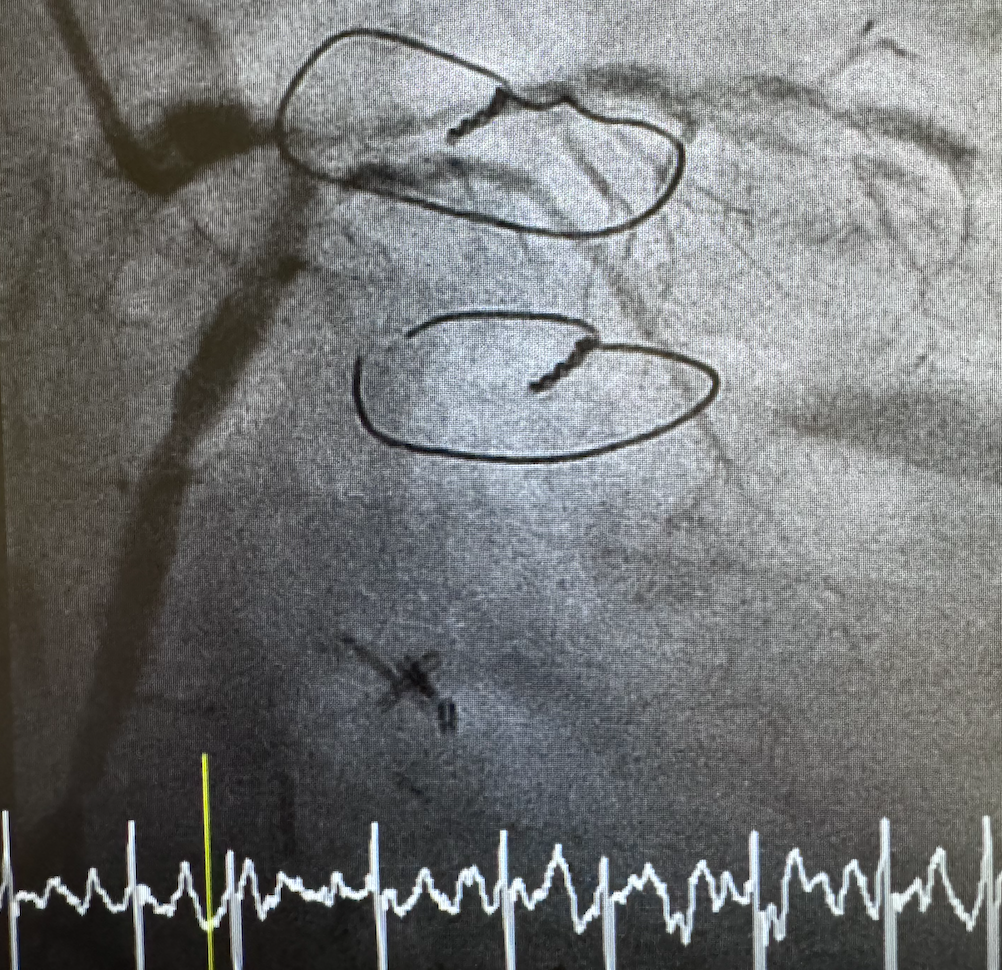
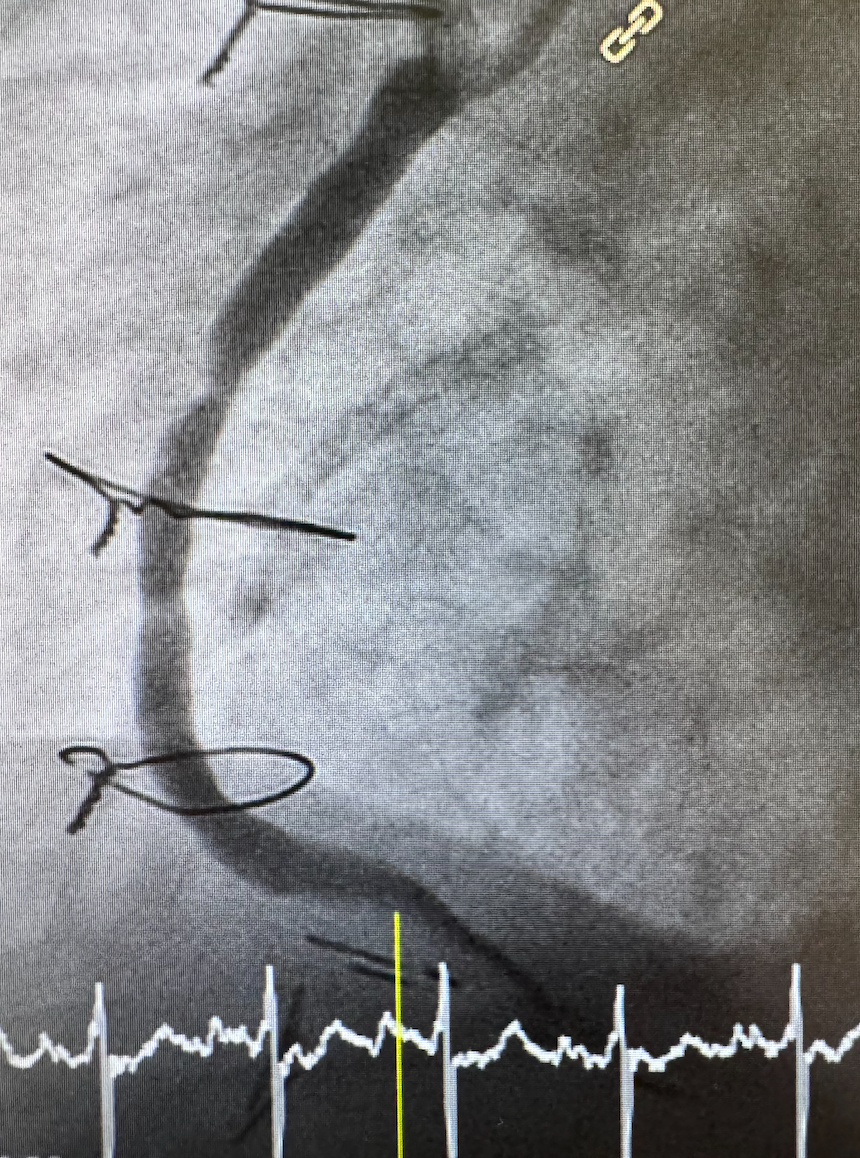
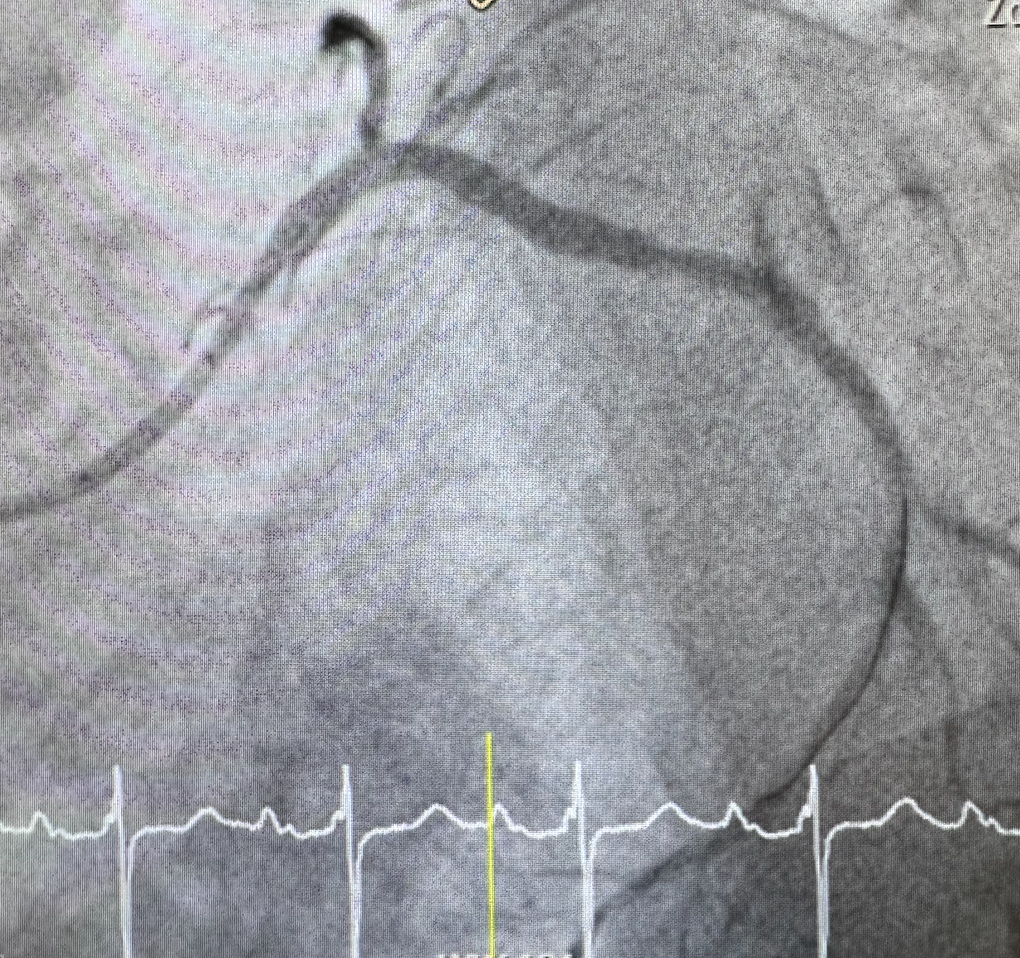
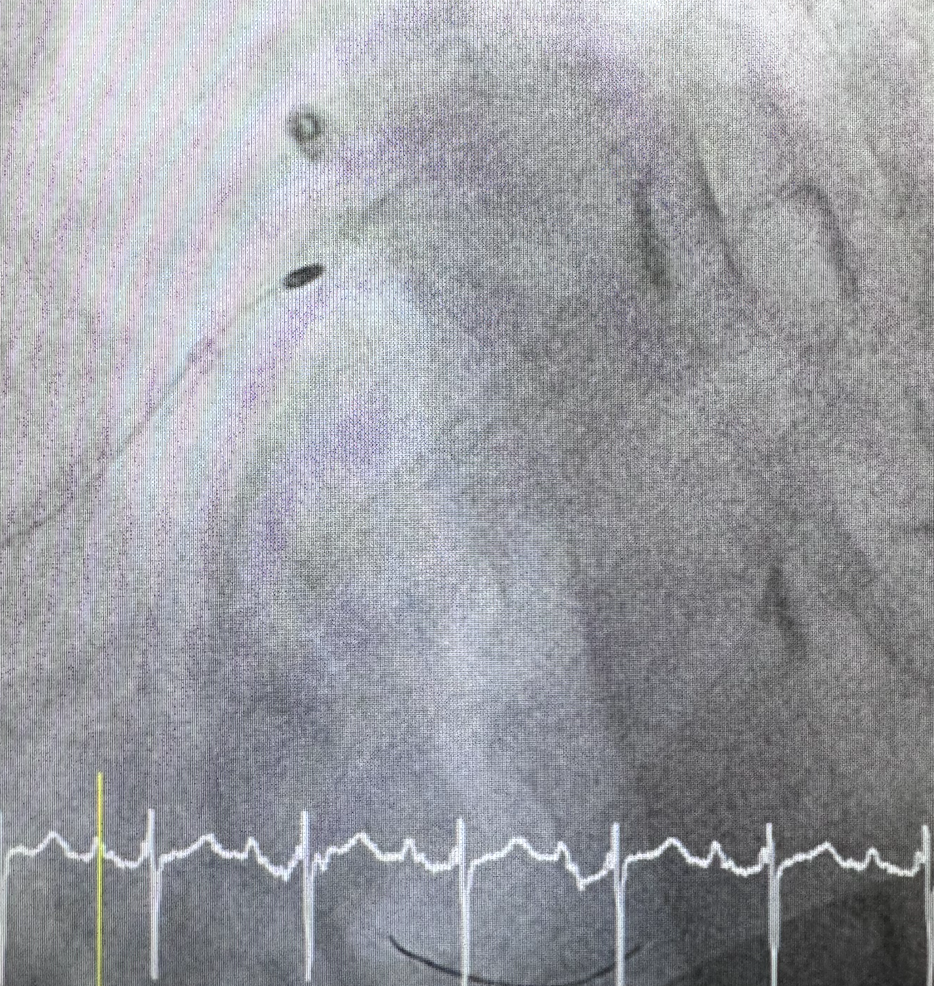
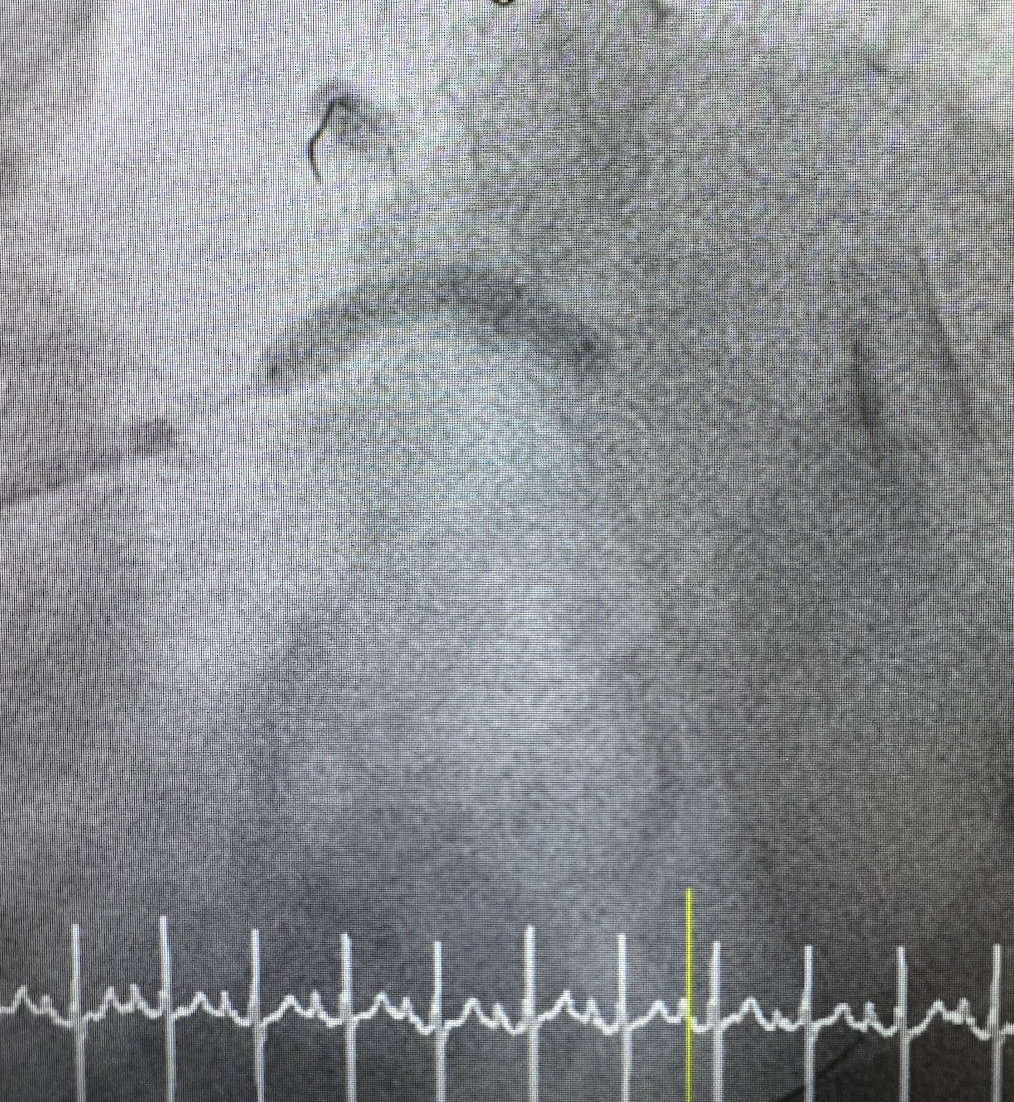
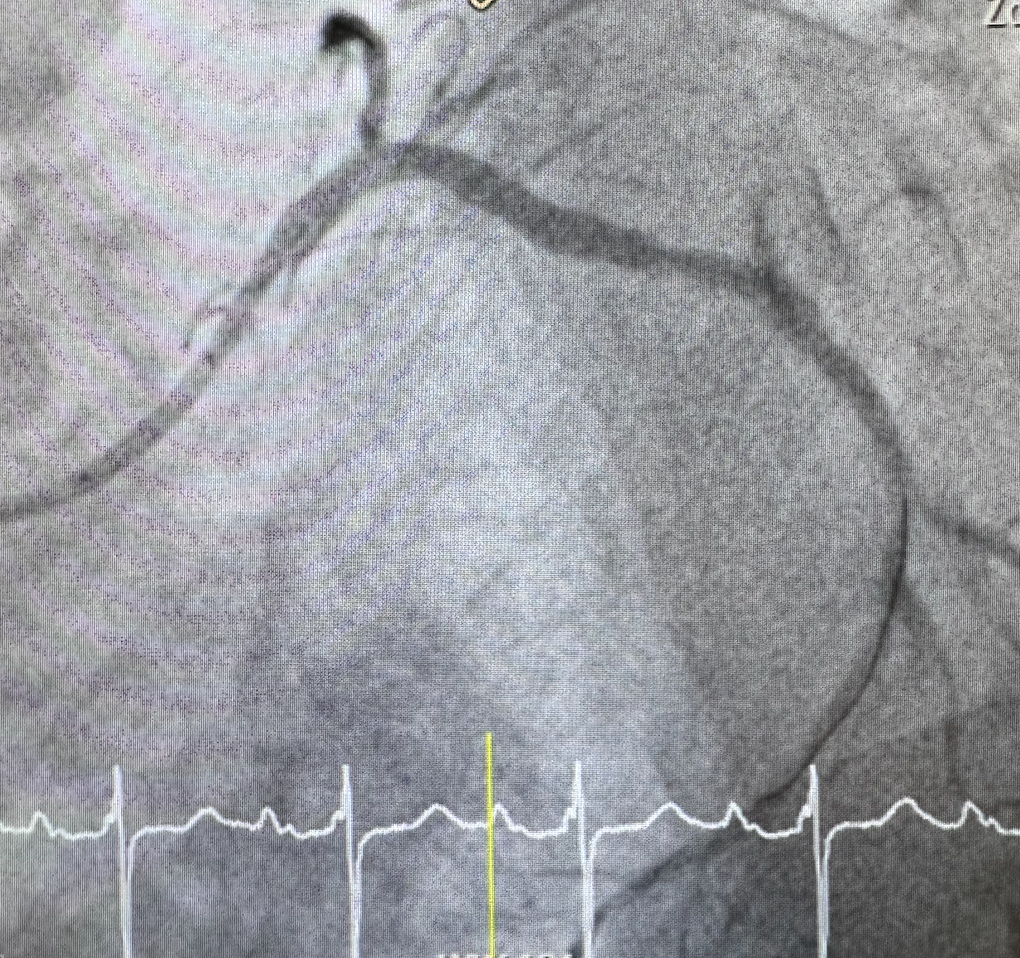
There was 80% mid to distal LM bifurcation (ISR at LM-LAD stent: Onyx 3.0x15 mm) Medina 1-1-1. 95% stenosis at proximal LAD, 100% stenosis at mid LAD, 80% calcified stenosis at proximal Lcx 100% stenosis at mid RCA (ISR at Cypher stent unknown size).There was 80% stenosis at mid SVG to PDA. Patent SVG to LAD and SVG to OM.


Interventional Management
Procedural Step
Culprit lesion was LM to proximal Lcx.A 7 Fr XB 3.5 guiding was engaged into LCA via right femoral artery.A Sion blue ES wire with 130cm fine cross microcatheter could advance into distal Lcx then wire was exchanged to RotaExtrasupport wire.Rotablator was done at Lm-proximal Lcx with Burr 1.75 at 190,000 rpm x 7 runs but could not pass lesion. Step down to 1.5 burr was done at 170,000 rpm x 3 runs and could pass lesion. step up burr to 1.75 at 170,000 rpm x 1 run for further debulking.A sion blue ES was wired to distal Lcx, A Fielder FC was wire to distal LADPre-dilated at proximal Lcx with NC balloon 3.5x15 mm at 20 atmResolute Onyx 4.0x22 mm was deployed at LM-proximal Lcx at 14 ATMFielder FC was retracted into guiding and rewire to mid LADstrut opening was done at LM-LAD with SC balloon 1.5x15 mm at 14 ATMPOBA was done at proximal LAD with NC balloon 3.0x15 mm at 20 ATM follow by DCB 3.0x20 mm at 10 ATMPost-dilated at LM-LCx was done with NC balloon 4.0x15 mm at 18 ATM.Final angiogram showed well expanded stent at LM-LCX with good coronary blood flow to both LAD and Lcx without evidence of complicationsWe also performed PCI to SVG to PDA using JR4 guiding and FilterWireEZ and direct stent with Resolute Onyx 5.0x30 mm at 16 ATM for complete revascularization in this patient.
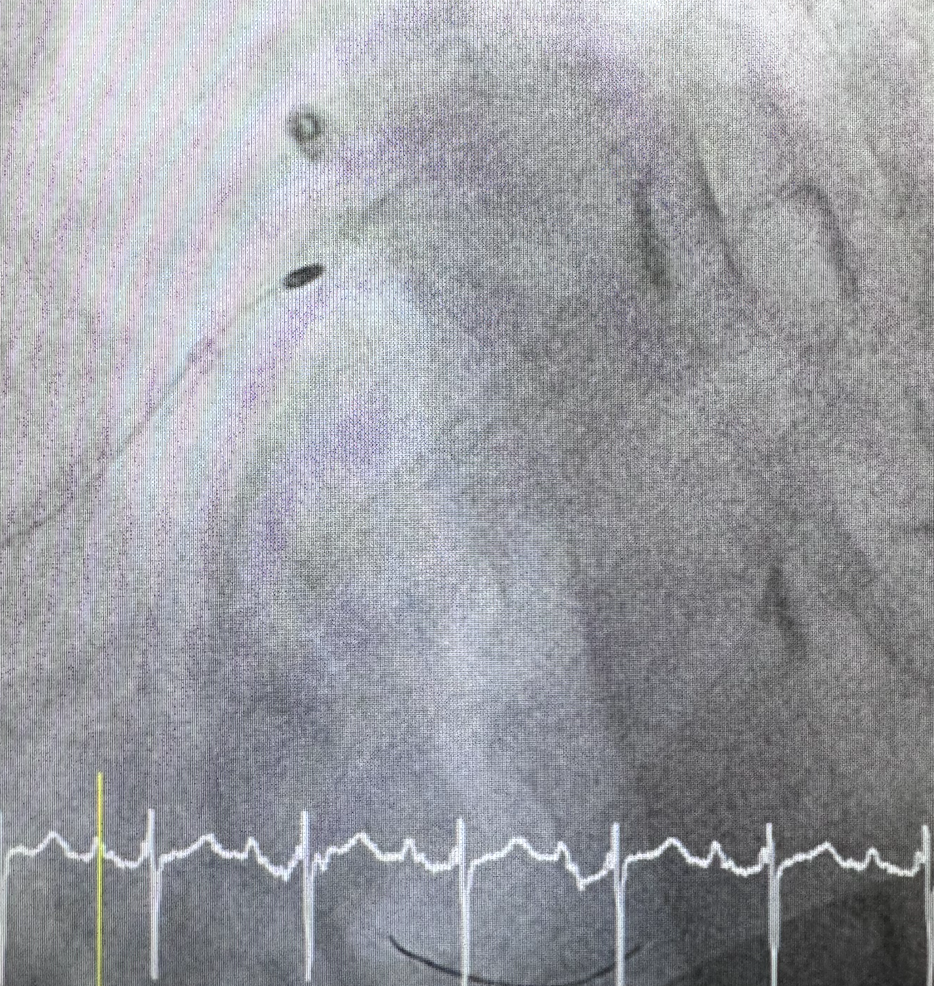
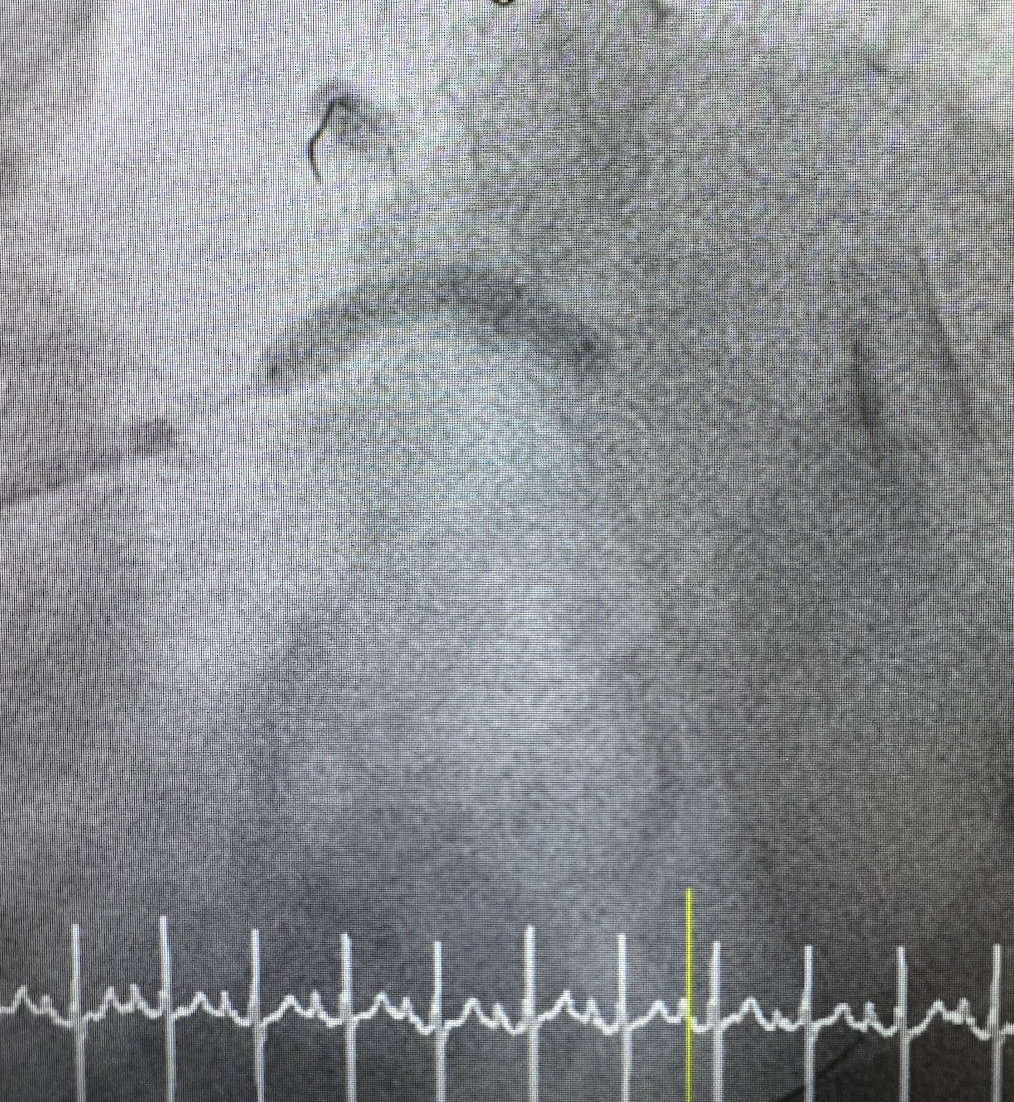
Case Summary
In this case we demonstrate that PCI in patient post CABG patient by correcting both native vessel and graft could be performed safely when surgical risk for redo CABG was high. Rotablator though previous stent may be difficult and required higher rotaspeed than usual. If rotaburr could not passed lesion step down of burr size was another option to pass lesion and then step back to previous burr size for adequate lesion preparation before pre-dilatation and stenting.

