Lots of interesting abstracts and cases were submitted for TCTAP 2024. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-029
A Challenging Case of Szabo Technique for Ostial Lesion in a Left Main Trifurcation
By Khoo Song Weng Ryan, Houng Bang Liew, Chong Wei Loong, Neerusha Kaisbain, Chew Fui Lo, Pangeran Akbar Syah
Presenter
Khoo Song Weng Ryan
Authors
Khoo Song Weng Ryan1, Houng Bang Liew1, Chong Wei Loong2, Neerusha Kaisbain1, Chew Fui Lo1, Pangeran Akbar Syah3
Affiliation
Queen Elizabeth II Hospital, Malaysia1, KPJ Sabah Specialist Hospital, Malaysia2, Gunung Jati General Hospital, Cirebon, Indonesia, Indonesia3,
View Study Report
TCTAP C-029
Coronary - Complex PCI - Bifurcation
A Challenging Case of Szabo Technique for Ostial Lesion in a Left Main Trifurcation
Khoo Song Weng Ryan1, Houng Bang Liew1, Chong Wei Loong2, Neerusha Kaisbain1, Chew Fui Lo1, Pangeran Akbar Syah3
Queen Elizabeth II Hospital, Malaysia1, KPJ Sabah Specialist Hospital, Malaysia2, Gunung Jati General Hospital, Cirebon, Indonesia, Indonesia3,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
A 55-year-old gentleman, ex-smoker with underlying Hypertension, Dyslipidaemia, and a history of NSTEMI a year ago, presented with sudden onset of chest pain in October 2023. General examination showed HR 78 bpm, sinus rhythm, BP 160/90mmHg; lungs and CVS unremarkable. ECG on arrival showed anteroseptal ST-segment elevation, consistent with acute extensive anterior STEMI. He was successfully re-perfused with Streptokinase and was listed for a pharmaco-invasive procedure the following day.
Relevant Test Results Prior to Catheterization
Troponin I was raised. Otherwise, other blood investigations are unremarkable. Chest X-ray showed clear lung fields with no cardiomegaly. Echocardiogram showed LVEF 45-50% with anterior, anteroseptal and apical hypokinesia.
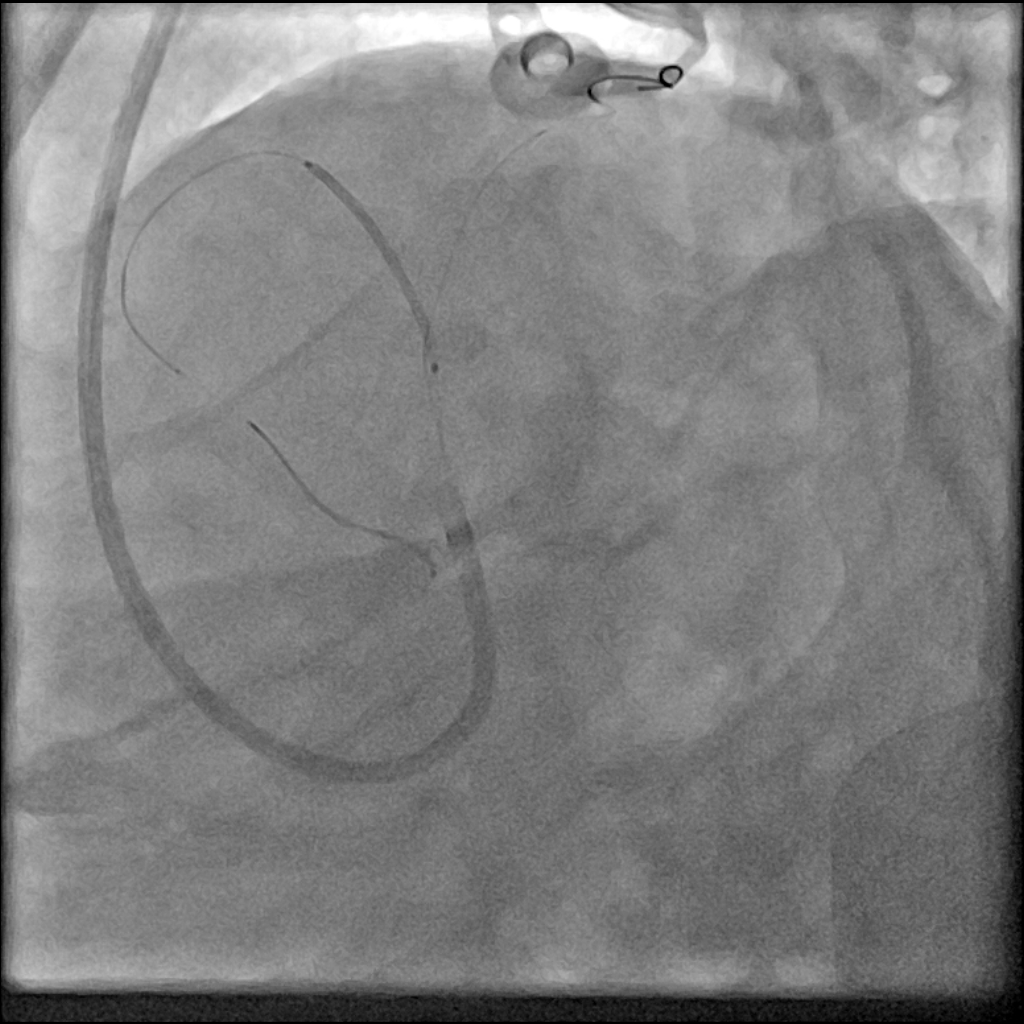
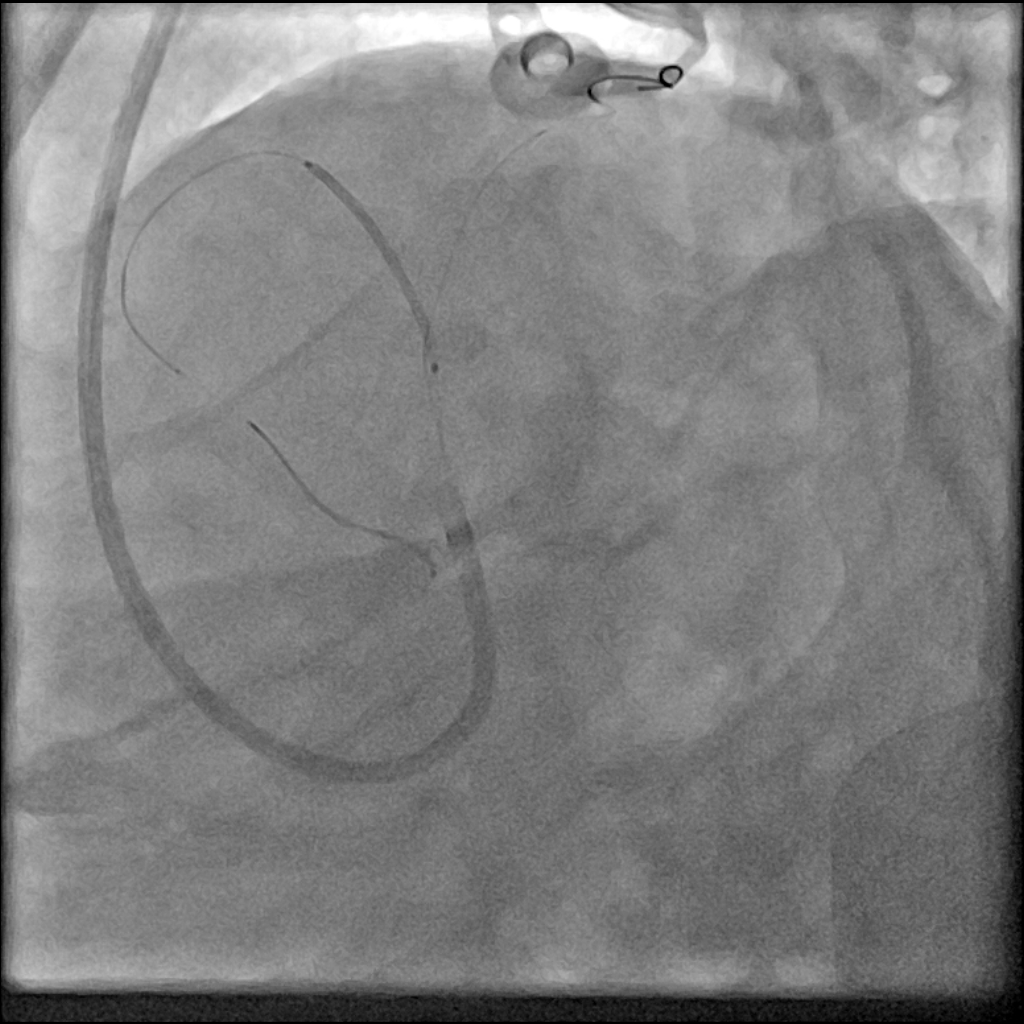
Relevant Catheterization Findings
A 6Fr trans-radial sheath was inserted. Coronary angiography showed mild disease of left main stem with trifurcation (Medina classification 0:1:0:1) with ostial to proximal LAD 70-90% disease involving D1 and mid-LAD 60-70% disease with both ostial D1 and D2 80-90% disease. LCx is dominant with mild irregularities and proximal main OM 40-50% disease. Ostial ramus 40-50% disease. RCA is recessive with mid 30-40% disease. We proceeded with PCI to LAD with IVUS and physiology guidance.






Interventional Management
Procedural Step
Trans-radial sheath was upsized to 7Fr. A 7Fr EBU 3.5 is used to engage the LCA and BMW guidewires are crossed into the distal LAD and distal ramus for protection. IVUS done for vessel sizing and plaque characterization from mid-LAD to LMS. IVUS Pre-PCI: mLAD after D2 (MLA: 3.4mm2, size: 3.7-3.9mm), pLAD (MLA: 4.5mm2, size: 3.9-4.4mm), oLAD (MLA: 3.6mm2, size: 4.3-4.9mm), dLMS (MLA: 17.3mm2, size: 5.8-6.6mm), mLMS (MLA: 18.3mm2, Size: 6-6.4mm). The proximal to ostial LAD lesion is pre-dilated with NC ScoreFlex 3.5x15mm (upto 12atm). The ostial to proximal LAD lesion is then stented with DES Resolute Onyx 3.5x20mm (12atm), using Szabo technique with the second wire in ramus for ostial LAD stent placement. Post-dilatation done with NC Sapphire 24 4.0x15mm (upto 14atm) with no residual disease/dissection. Post-stenting PdPa done via perforated balloon: 0.83 and QFR:0.75. After post-dilatation, the ramus guidewire is wired into distal D2. The mid-LAD lesion is pre-dilated with NC ScoreFlex 3.5x15mm (6atm) and the ostial-proximal D2 lesion is pre-dilated with NC Euphora 2.25x15mm (upto 14atm). The mid-LAD lesion is then treated with DCB Sequent Please NEO 3.0x25mm (6atm,60sec) and the ostial-proximal D2 lesion is treated with DCB Sequent Please NEO 2.25x15mm (6atm,60sec) with post-PCI PdPa: 0.95 and QFR: 0.87. IVUS post-PCI: pLAD (MSA: 8.2mm2), oLAD (MSA: 11.4mm2). Post-procedure, the radial sheath is removed.




Case Summary
Left main stem trifurcation stenosis with the complexity of 3 branches, with at least 4 variable angles, and variability in branch size and lesion severity, especially in ostial lesions, presents a challenge for percutaneous coronary intervention. In addition to optimal coronary angiographic views, the use of Szabo technique is feasible in tackling left main trifurcation with ostial disease of branches, followed by coronary imaging to achieve optimal stent expansion. The use of DCBs for the mid-LAD bifurcation lesion as part of a hybrid strategy reduces the total stent length and avoids stent in small side branches while maintaining an effective anti-proliferative action.

