Lots of interesting abstracts and cases were submitted for TCTAP 2024. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-012
A-Sixty-Five-Year-Old Man With Coronary Artery Aneurysm Experiences Acute Myocardial Infarction
By Lo-chia Yeh, Shih Wei Meng
Presenter
Lo-chia Yeh
Authors
Lo-chia Yeh1, Shih Wei Meng1
Affiliation
National Taiwan University Hospital, Taiwan1,
View Study Report
TCTAP C-012
Coronary - ACS/AMI
A-Sixty-Five-Year-Old Man With Coronary Artery Aneurysm Experiences Acute Myocardial Infarction
Lo-chia Yeh1, Shih Wei Meng1
National Taiwan University Hospital, Taiwan1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
A 65-year-old freelance worker with a history of stable lung adenocarcinoma and benign prostate hyperplasia presented with general weakness, syncope, chest tightness, and cold sweats during a routine follow-up at our outpatient department. The patient soon regained consciousness and was able to remember the whole process. He had a history of heavy smoking (up to 1 pack per day for 30 years). Upon examination, the patient displayed bilateral crackles and pitting edema in the lower limbs.
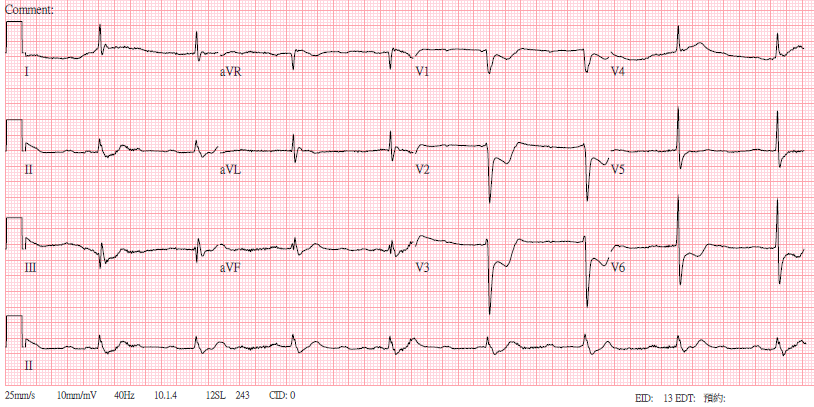


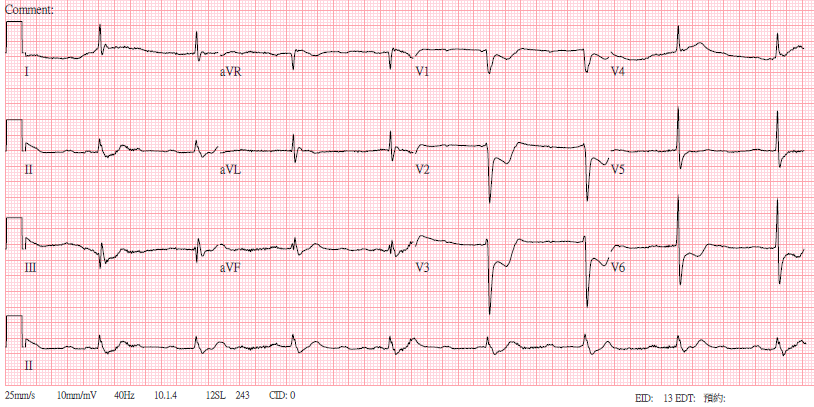


Relevant Test Results Prior to Catheterization
His ECG showed complete atrioventricular block with junctional rhythm, anteroseptal ST depression. Laboratory data showed lactic acidosis and elevated Troponin-T. The patient developed bradycardia and was treated with atropine and dopamine, but subsequently experienced dyspnea, desaturation, and cardiogenic shock. He was intubated and started on norepinephrine. A transthoracic echocardiogram showed posterior wall hypokinesia, indicative of a posterior myocardial infarction.
Relevant Catheterization Findings
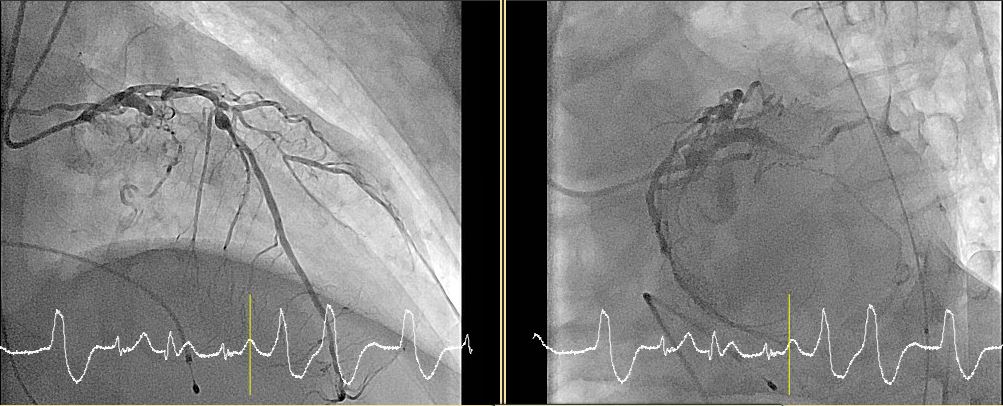
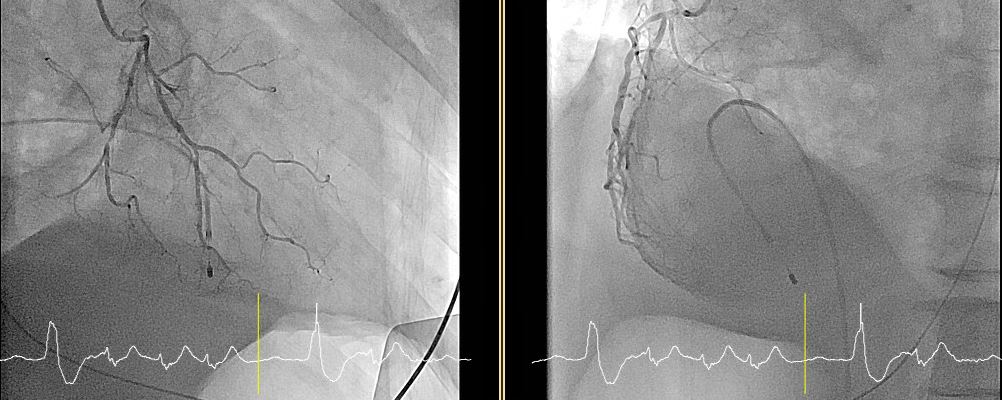
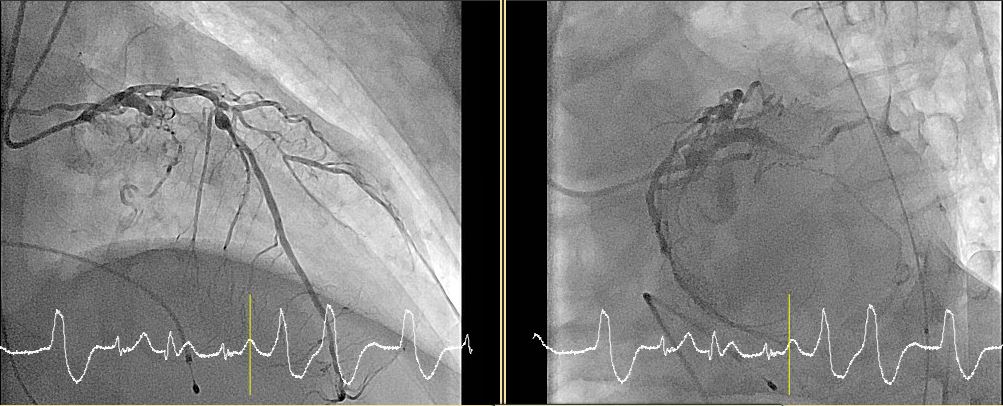
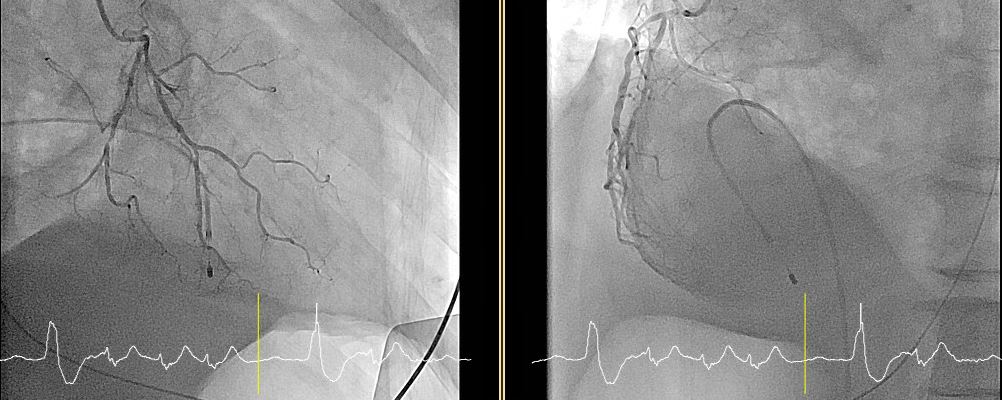
Prior to the PCI, a temporary pacemaker and an IABP (Maquet Datascope 40cc) were placed. The diagnostic catheterization revealed:LM (left main): Patent;LAD (left anterior descending): proximal, middle, diagonal bifurcation lesion (1,1,1) up to 50-60% stenosis with aneurysmal change;LCX (left circumflex): proximal, distal, OM bifurcation lesion(1,1,1) up to 99% stenosis with thrombus, distal chronic total occlusion (CTO);RCA (right coronary artery): hypoplasia, proximal up to 50 % stenosis.


Interventional Management
Procedural Step
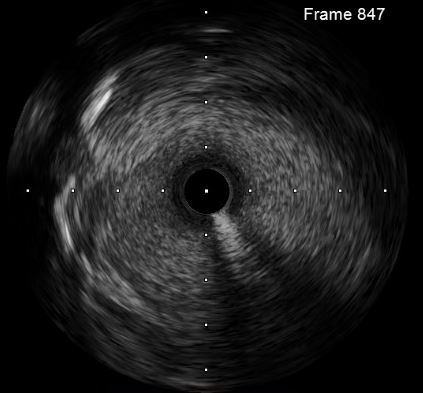
The clinical team engaged a cardiovascular surgeon for possible coronary artery bypass grafting (CABG) and prepared for ECMO (Extracorporeal Membrane Oxygenation) support in case of profound cardiogenic shock. The surgeon suggested perform PCI and mange to enhance antegrade flow first. During the procedure, the patient experienced non-sustained ventricular tachycardia (~150 bpm) without hypotension, which resolved without intervention. The guiding catheter "Medtronic EBU3.5 6Fr" was inserted into the left coronary artery, and the coronary wire " ASAHI Sion"was wired to his distal LCX. Thrombosuction was performed using the "Terumo ELIMINATE Aspiration catheter 6FR" for 4 times with red thrombi aspirated. IVUS imaging with "BOSTON IVUS cath 2.5F 40MHz" confirmed aneurysmal changes in the distal LCx but deemed stent placement challenging. The final flow achieved a TIMI II score (Thrombolysis in Myocardial Infarction). A V-A ECMO was inserted (with reperfusion tube), and the patient was transferred to the coronary care unit (CCU) as a bridge to CABG. Two days later, he underwent successful beating heart CABG with partial cardiopulmonary bypass (CPB).




Case Summary
This case involves a 65-year-old man with coronary artery disease complicated by acute coronary syndrome, Killip classification IV, cardiogenic shock, complete atrioventricular block, and post-PCI target vessel thrombosuction. The patient was supported with an IABP, temporary pacemaker, and V-A ECMO during his hospitalization. The presence of coronary artery aneurysms was a key factor in his condition, emphasizing the importance of angiography and intravascular imaging in diagnosis. The optimal management of such cases remains a topic of debate.

