Lots of interesting abstracts and cases were submitted for TCTAP 2024. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-027
Measure Twice, Cut Once
By Chi Na Cheng, Wai Lun Mak, Tsz Ho Chan, Shung Yee Wong, Chi Wing Wong
Presenter
Chi Na Cheng
Authors
Chi Na Cheng1, Wai Lun Mak1, Tsz Ho Chan1, Shung Yee Wong1, Chi Wing Wong1
Affiliation
Pok Oi Hospital, Hong Kong, China1,
View Study Report
TCTAP C-027
Coronary - Complex PCI - Bifurcation
Measure Twice, Cut Once
Chi Na Cheng1, Wai Lun Mak1, Tsz Ho Chan1, Shung Yee Wong1, Chi Wing Wong1
Pok Oi Hospital, Hong Kong, China1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
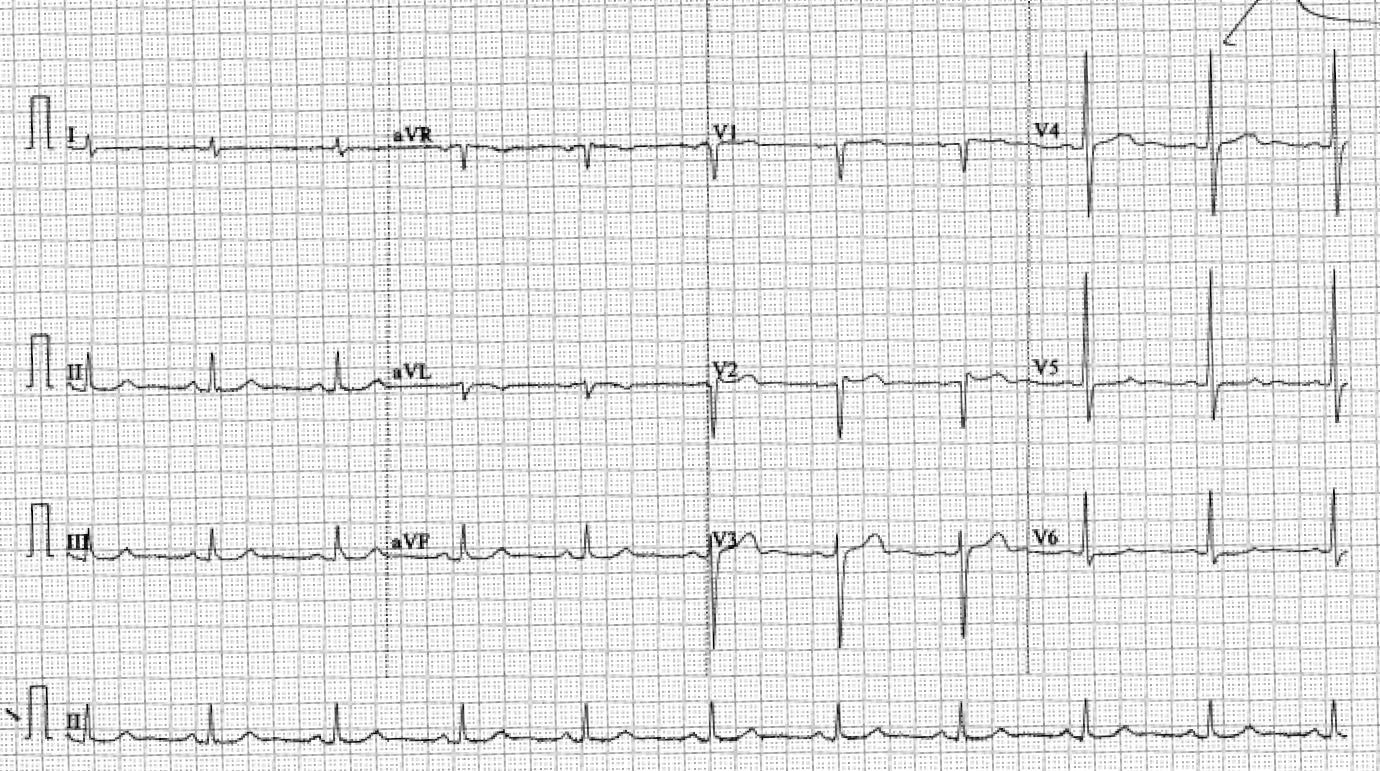
Mr Fu was a 72-year-old gentleman with history of hypertension and hyperlipidemia. He complained of exertional angina for 6 months. Physical examination was grossly unremarkable. ECG showed sinus rhythm.
Relevant Test Results Prior to Catheterization
Echocardiogram showed hypokiensia over anterior wall and basal septum, with an impaired LVEF of 45%.
Relevant Catheterization Findings
Coronary angiogram showed triple vessel disease with distal left main bifurcation disease (medina 1,1,1). Ostial to mLAD diffuse 80% stenosisOstial to mLCx diffuse 80% stenosisRCA dominant, diffuse moderate to severe steosis


Interventional Management
Procedural Step
F7 EBU 3.5 was engaged to LMS. Sion wire to left anterior descending artery (LAD), Runthrough extraFloppy to left circumflex artery (LCx). Altaview IVUS to LAD and LCx for vessel sizing and lesion analysis.
We decided to perform stenting to mid LAD first, then treat the left main stem (LMS) bifurcation with DK Crush technique. Lesion preparation to LAD was done with Lacrosse NSE 2.0/13 at 14-24 atm. Stenting to mLAD was done with Ultimaster Nagomi 2.5/44 at 9-14 atm.
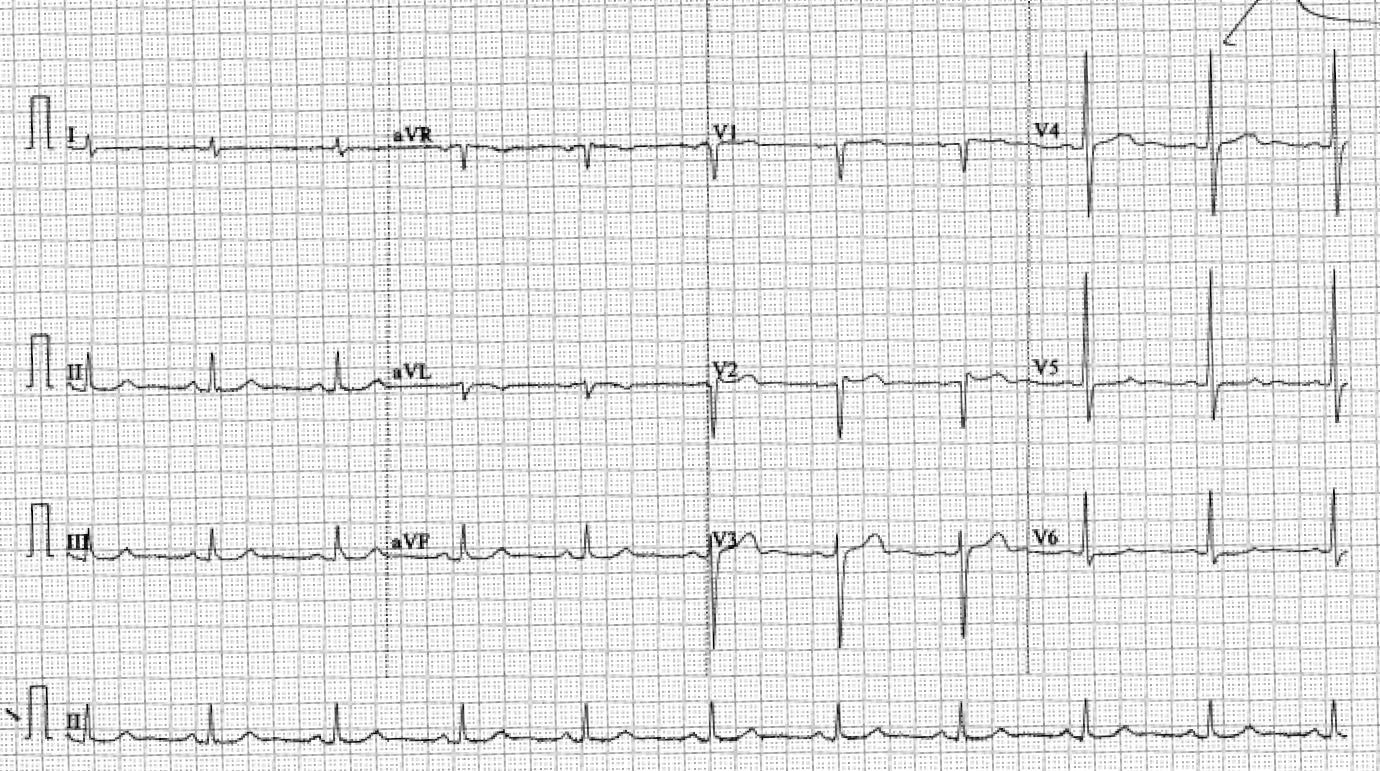
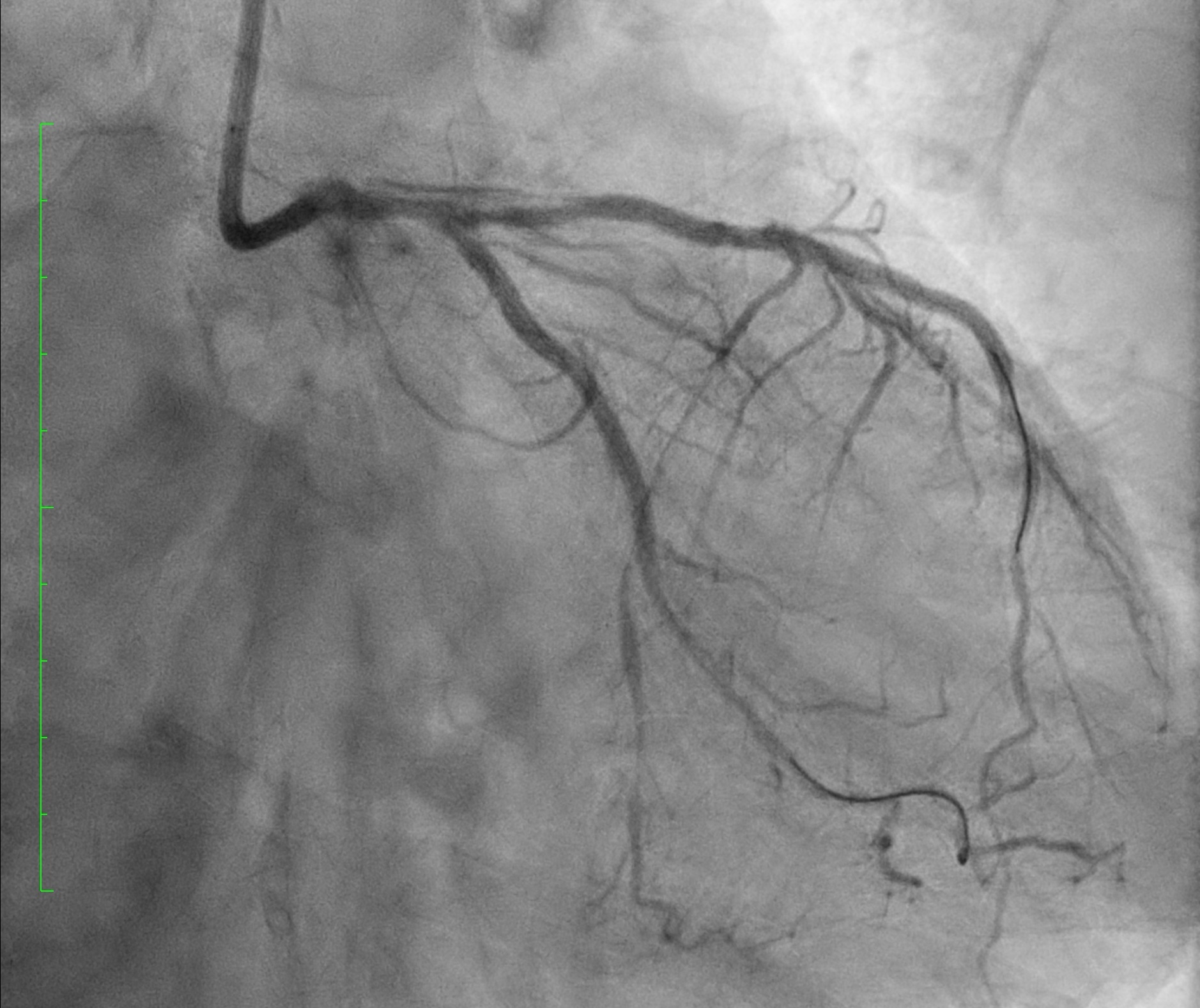
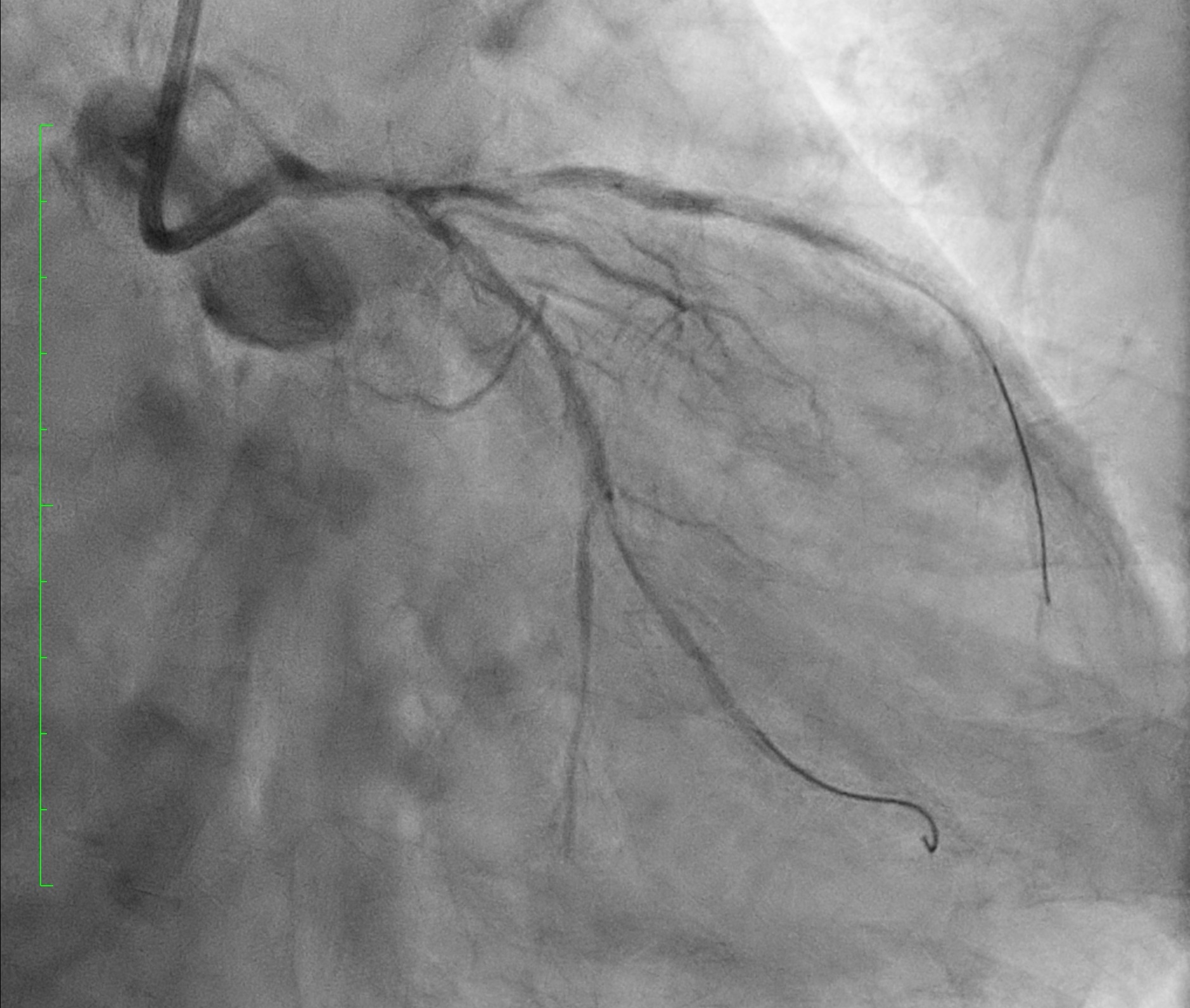
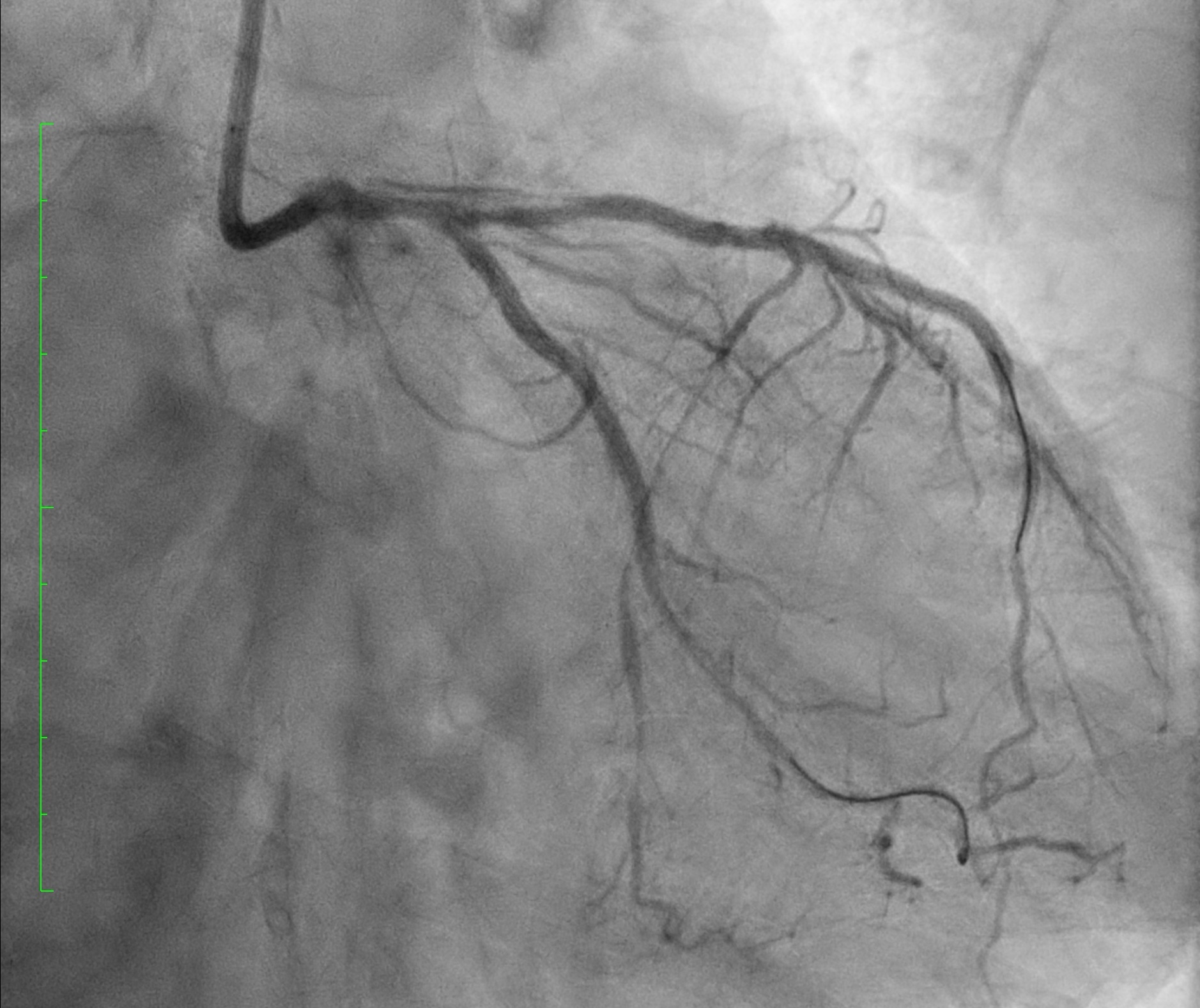
However, patient developed chest discomfort. Coronary angiogram showed type B coronary artery dissection LMS to LAD [see fig 1]. We decided to proceed to DK Crush to LMS bifurcation. Intended stenting to LCx with with Ultimaster Nagomi 2.25/38 at 10atm. [see fig 2]. Intended Crushing with Accuforce 3.5/15 to LMS-LAD.
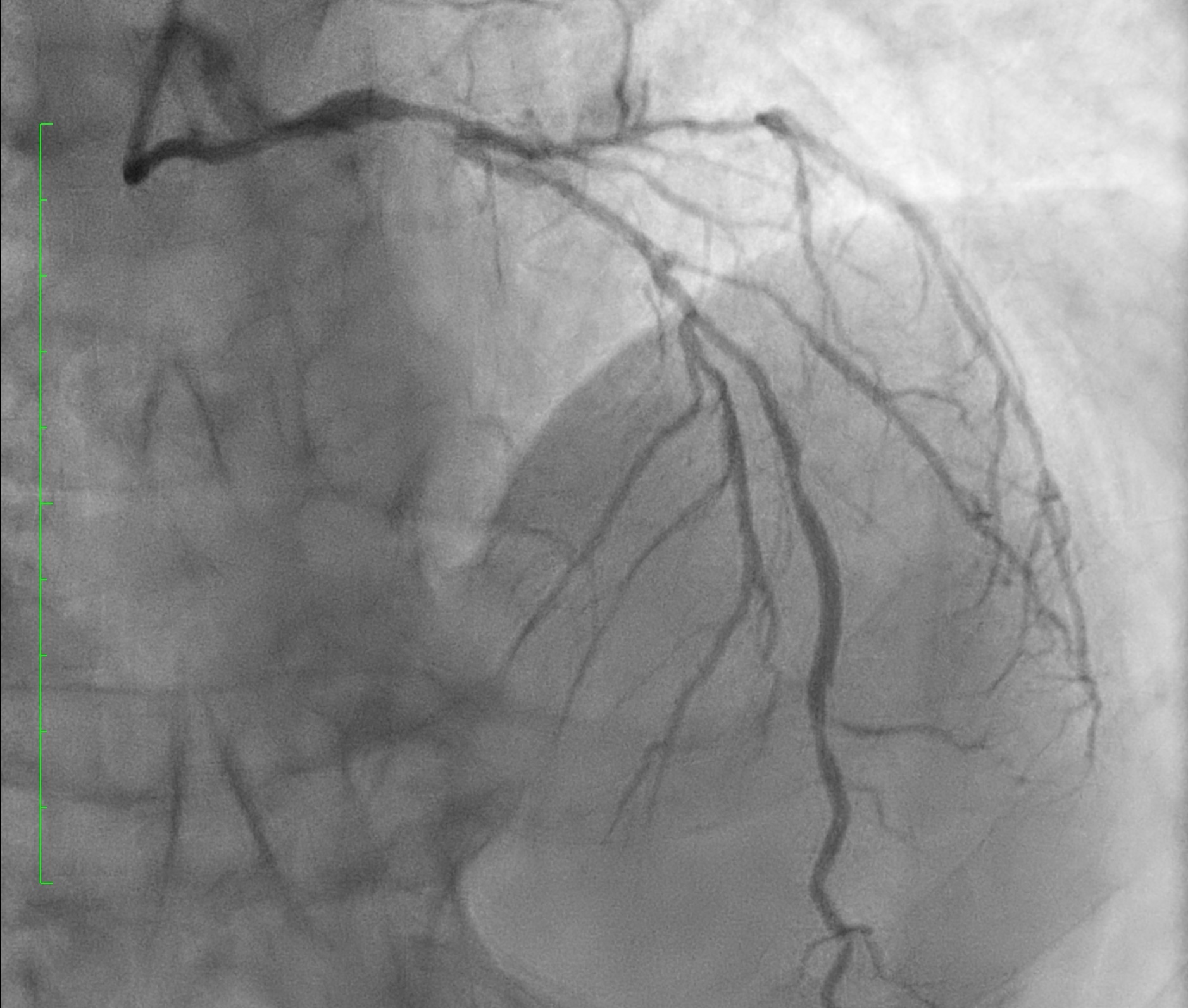
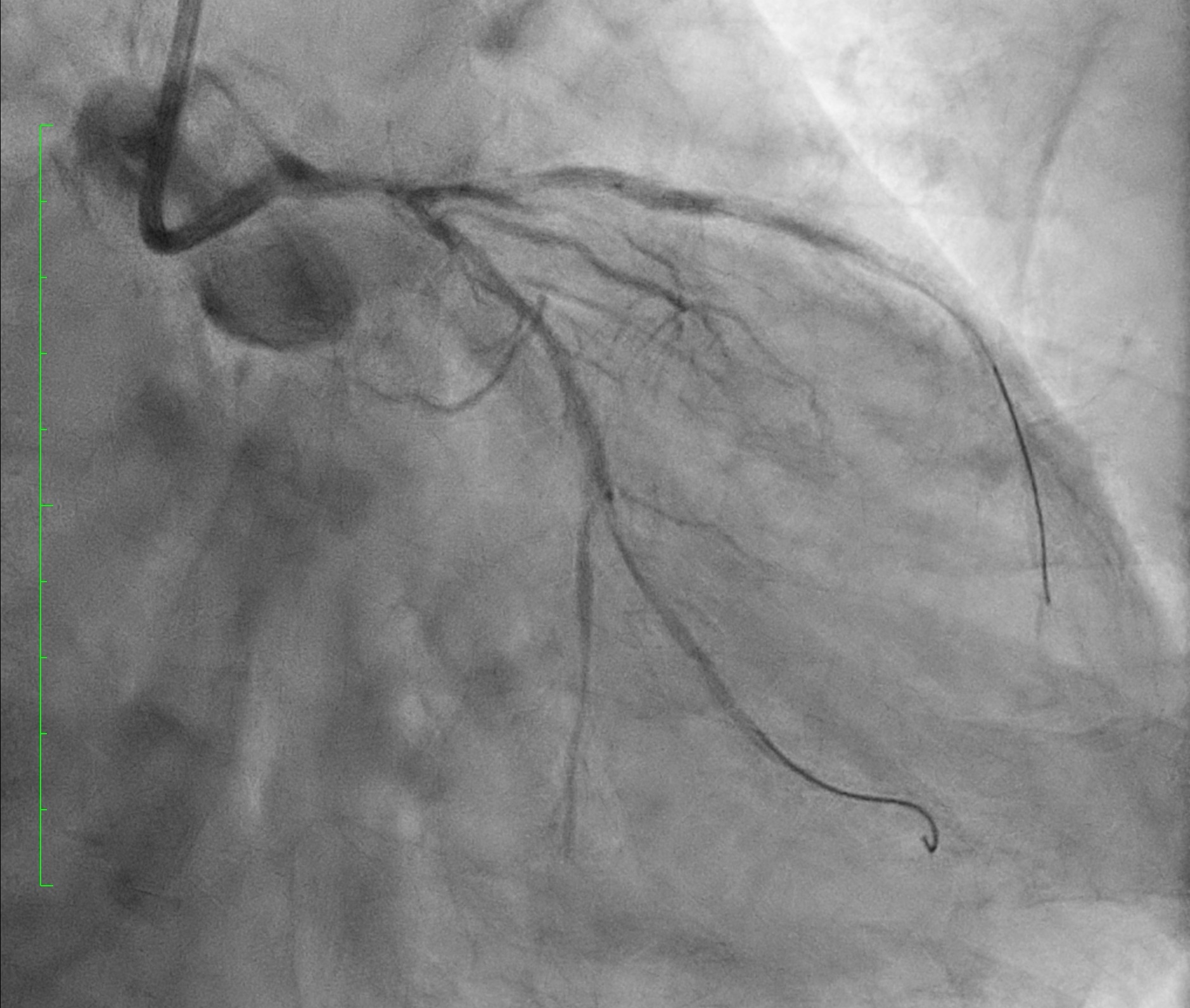
Coronary angiogram showed unintended too distal position of LCx stent, missing the ostial LCx lesion. [see fig 3]We decided to proceed to stenting to LMS-LAD. Kissing balloon inflation (KBI) to bifurcation with 3.0/15 NC SeQuent Neo and 2.5/15 NC Pantera Leo at 8atm. Stenting to LMS-LAD with Ultimaster Nagomi 3.0/33 at 12 atm. KBI to bifurcation with 3.0/15 NC SeQuent Neo and 2.5/15 NC Pantera Leo at 8atm. TIMI3 flow was maintained, and dissection was controlled
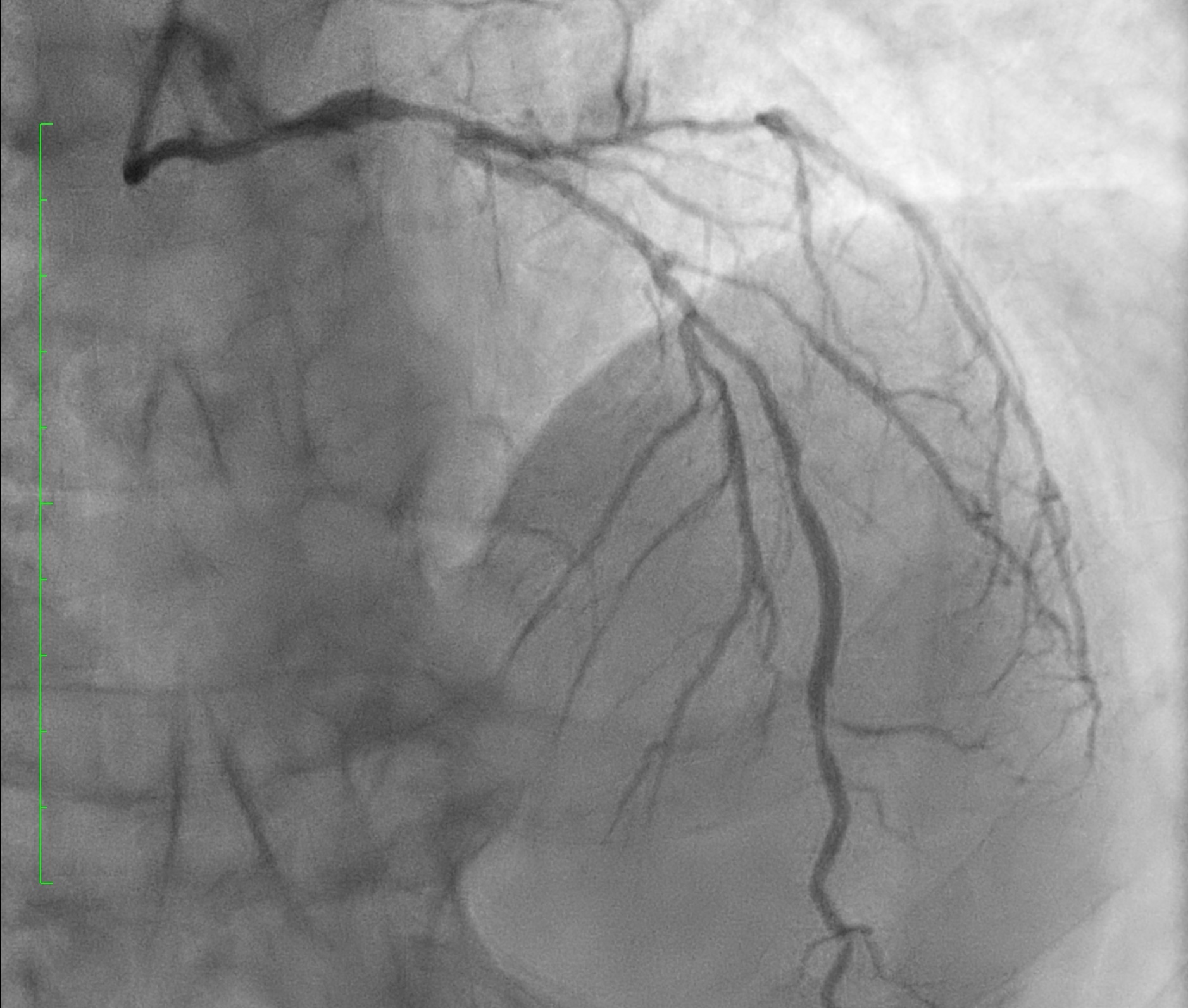
For the ostial LCx lesion, we decided to use drug-coated balloon angioplasty (DCB). DCB to ostial LCx with 2.5/15 Magic Touch at 12 atm.
Final angiogram and IVUS showed good result.

We decided to perform stenting to mid LAD first, then treat the left main stem (LMS) bifurcation with DK Crush technique. Lesion preparation to LAD was done with Lacrosse NSE 2.0/13 at 14-24 atm. Stenting to mLAD was done with Ultimaster Nagomi 2.5/44 at 9-14 atm.
However, patient developed chest discomfort. Coronary angiogram showed type B coronary artery dissection LMS to LAD [see fig 1]. We decided to proceed to DK Crush to LMS bifurcation. Intended stenting to LCx with with Ultimaster Nagomi 2.25/38 at 10atm. [see fig 2]. Intended Crushing with Accuforce 3.5/15 to LMS-LAD.
Coronary angiogram showed unintended too distal position of LCx stent, missing the ostial LCx lesion. [see fig 3]We decided to proceed to stenting to LMS-LAD. Kissing balloon inflation (KBI) to bifurcation with 3.0/15 NC SeQuent Neo and 2.5/15 NC Pantera Leo at 8atm. Stenting to LMS-LAD with Ultimaster Nagomi 3.0/33 at 12 atm. KBI to bifurcation with 3.0/15 NC SeQuent Neo and 2.5/15 NC Pantera Leo at 8atm. TIMI3 flow was maintained, and dissection was controlled
For the ostial LCx lesion, we decided to use drug-coated balloon angioplasty (DCB). DCB to ostial LCx with 2.5/15 Magic Touch at 12 atm.
Final angiogram and IVUS showed good result.

Case Summary
Dissection is a well known complication which may progress and limit the coronary blood flow. Rapid identification is important.
In our case of unintended too distal landing of side branch stent, we chose to use DCB as a strategy to avoid extra stent layer and prevent late lumen loss. The patient will have coronary angiogram for restudy. In case of suboptimal result of ostial LCx lesion, further stenting can be perform.
Prevention is still the key to optimise the result of revascularization.
In our case of unintended too distal landing of side branch stent, we chose to use DCB as a strategy to avoid extra stent layer and prevent late lumen loss. The patient will have coronary angiogram for restudy. In case of suboptimal result of ostial LCx lesion, further stenting can be perform.
Prevention is still the key to optimise the result of revascularization.

