Lots of interesting abstracts and cases were submitted for TCTAP 2024. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-051
A Challenging Two CTOs Case Report: Man Proposes, but God Disposes
By You-Ning Chang, Chuan-Tsai Tsai
Presenter
You-Ning Chang
Authors
You-Ning Chang1, Chuan-Tsai Tsai1
Affiliation
Taipei Veterans General Hospital, Taiwan1,
View Study Report
TCTAP C-051
Coronary - Complex PCI - CTO
A Challenging Two CTOs Case Report: Man Proposes, but God Disposes
You-Ning Chang1, Chuan-Tsai Tsai1
Taipei Veterans General Hospital, Taiwan1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
A 72-year-old Han Chinese male was diagnosed as type II DM, dyslipidemia, HTN for years and under medication controlled. He had received revascularization for LAD and a DES was deployed there and failed to revascularize RCA at that time. Prior 1 month admission, he experienced dyspnea and chest oppression tightness sensation and sought medical help. Otherwise, he denied tearing chest pain, weight gain, orthopnea. Physical exam showed clear breathing sound with regular heartbeat and no edema.
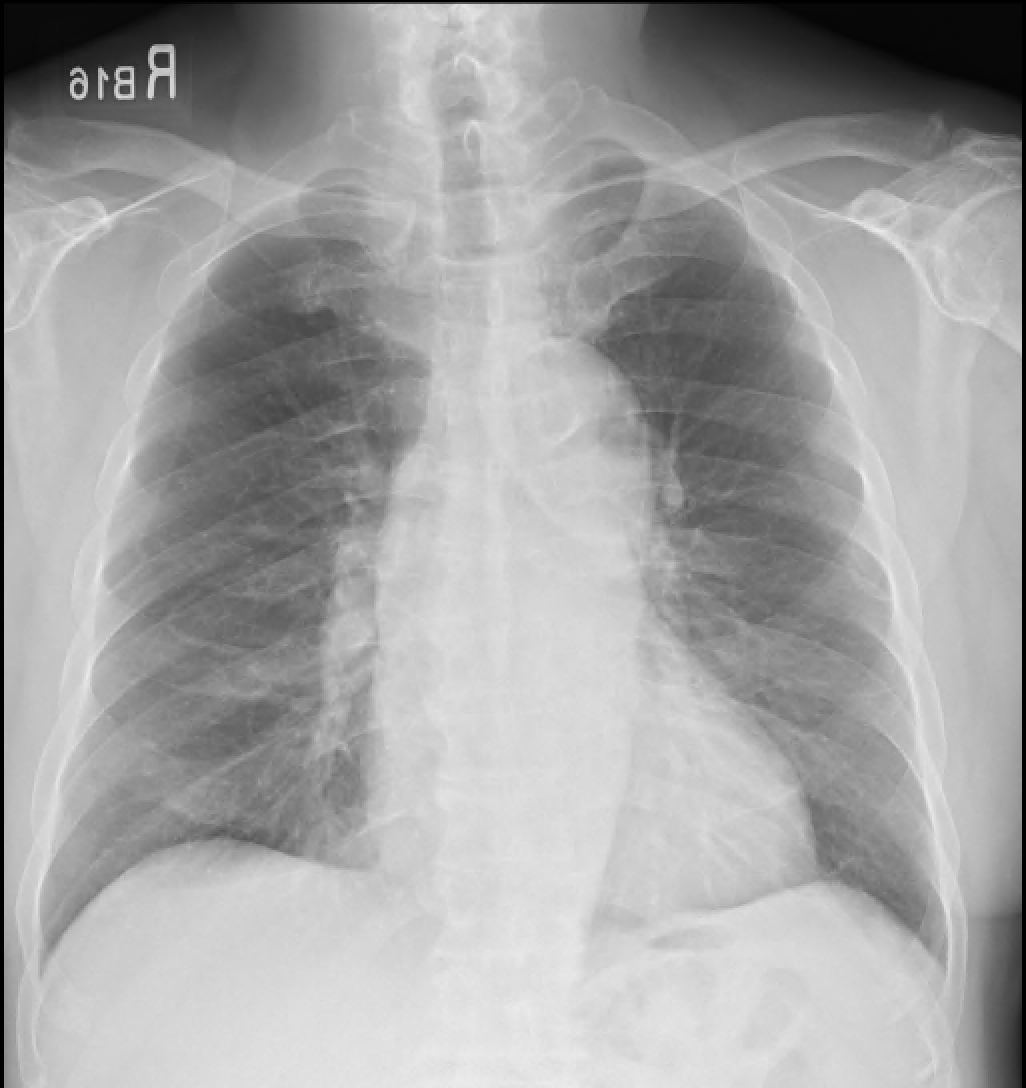

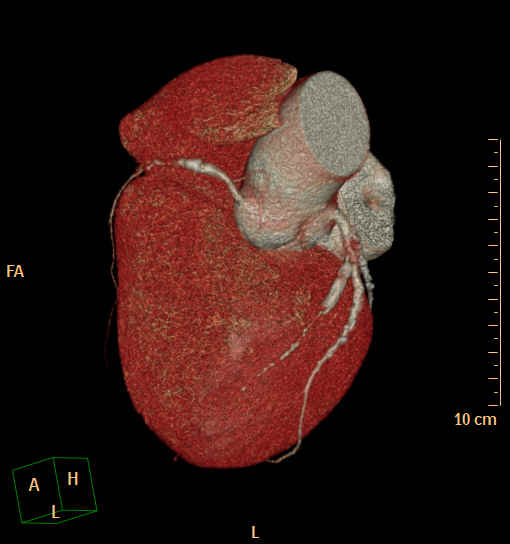
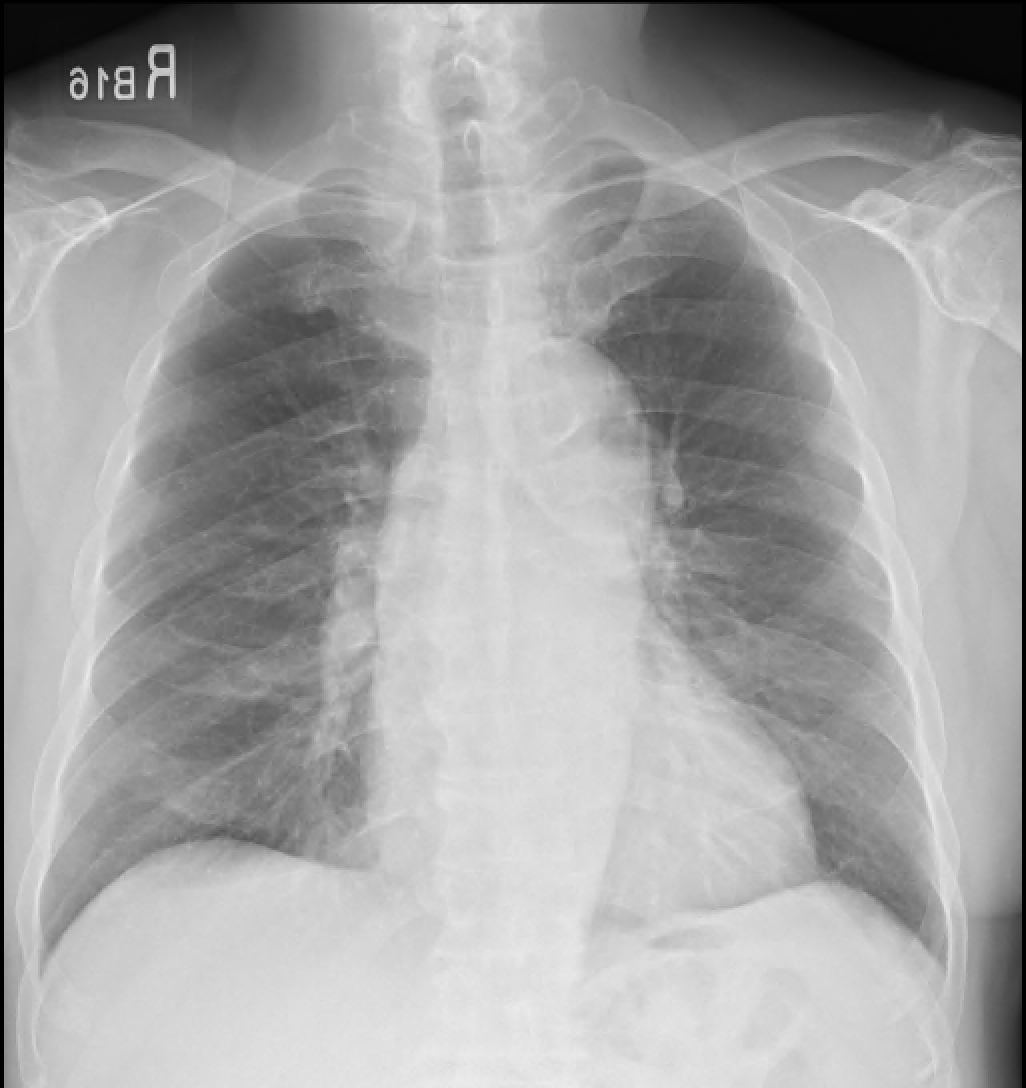

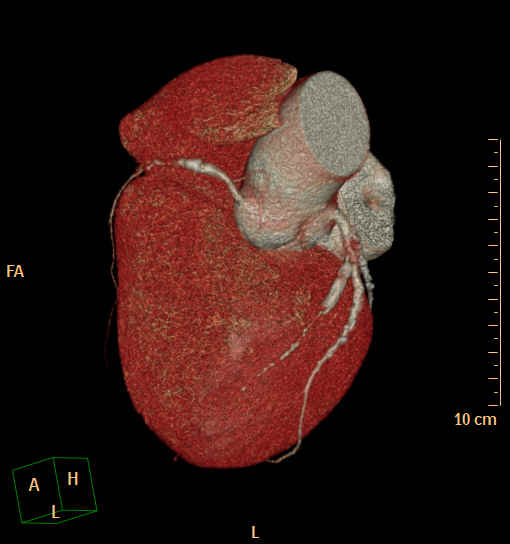
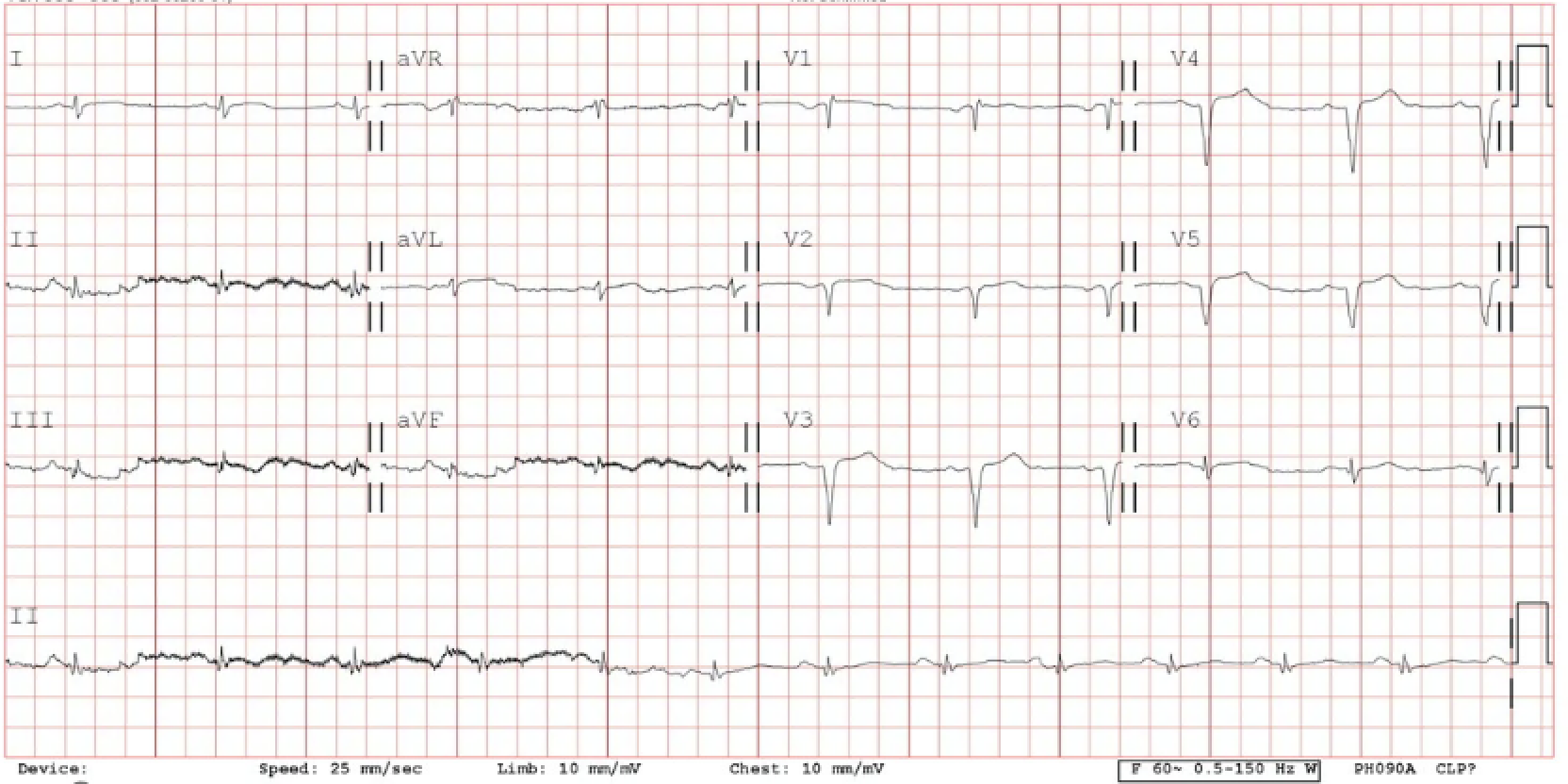
Relevant Test Results Prior to Catheterization
Coronary CTA revealed double vessel disease. The calcium score was 1291. Pre-procedure blood tests revealed normal results except renal impairment and hyperglycemia. The first time catheterization confirmed CTA results and RCA CTO, collateral from LCX and LAD-D1 with LAD-P CTO as well. We tried to revascularize proximal LAD and RCA CTO cap under support of microcatheters but failed. The patient experienced chest pain after the procedure and periprocedural MI. He was discharged 6 days smoothly.




Relevant Catheterization Findings
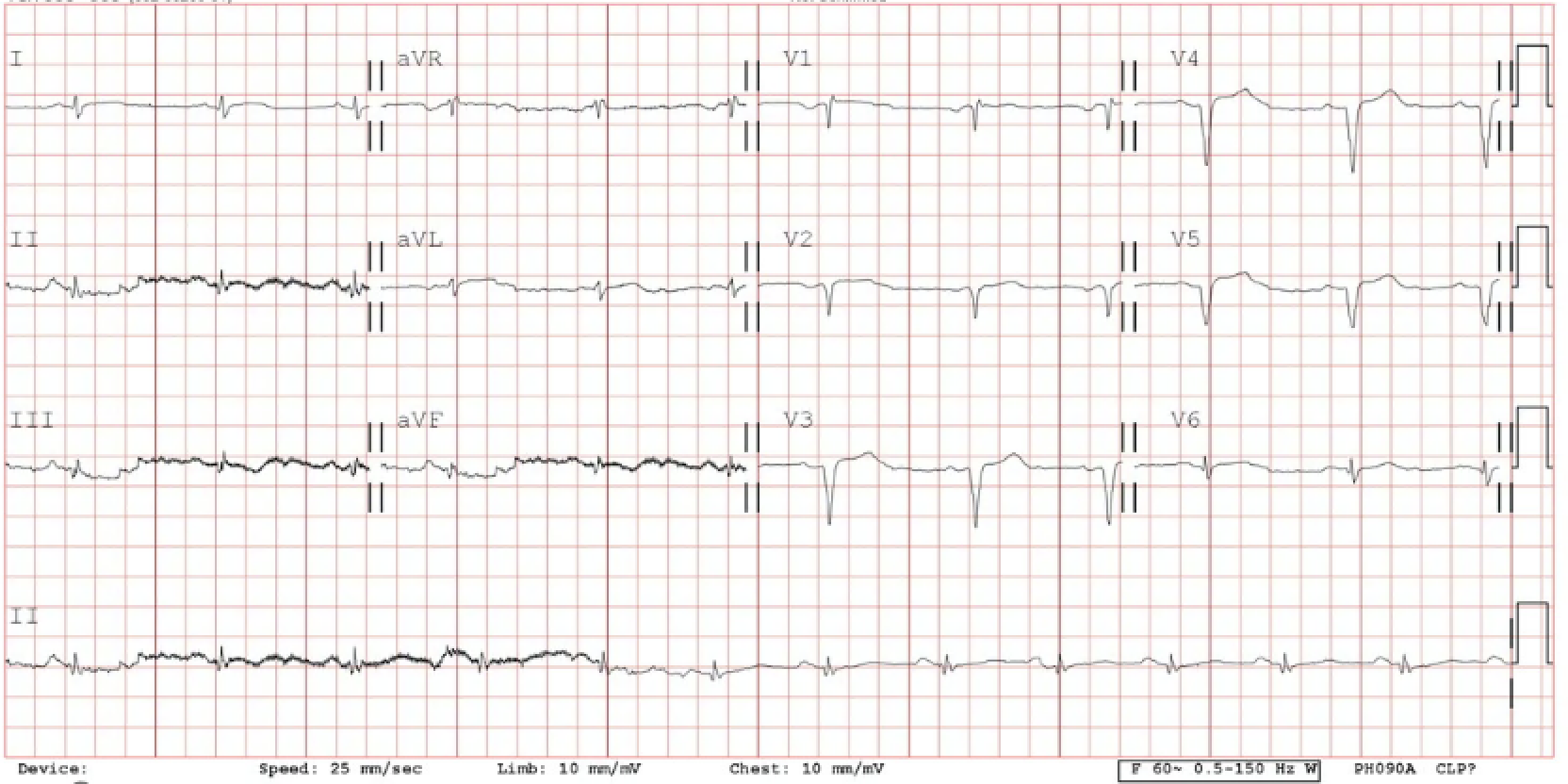
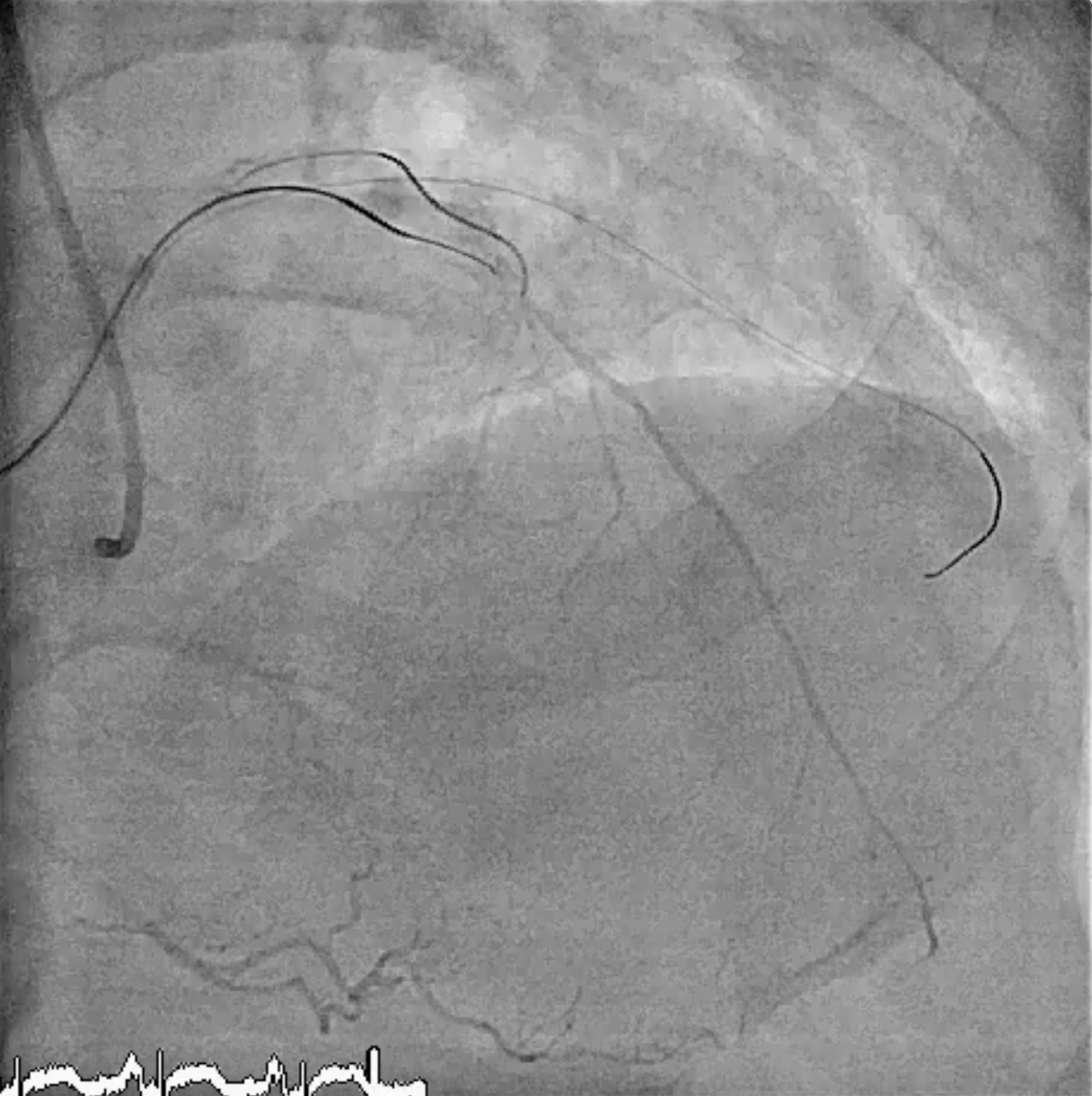
We tried to revascularize again 2 weeks after the first procedure. This time, our strategy was to revascularize LAD CTO under IVUS guidance to penetrate the CTO cap. If LAD CTO was successfully revascularized, a primary retrograde appraoch via LCX-OM branch epicardial collateral was planned for RCA CTO and then kissing wire or reverse CART technique. Hopefully, revascularize two CTOs in one stage procedure. However, during the second time CAG, we found CTO was extended to LAD-Os.


Interventional Management
Procedural Step
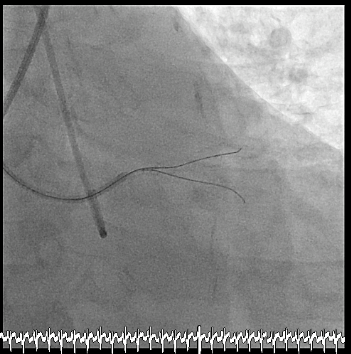
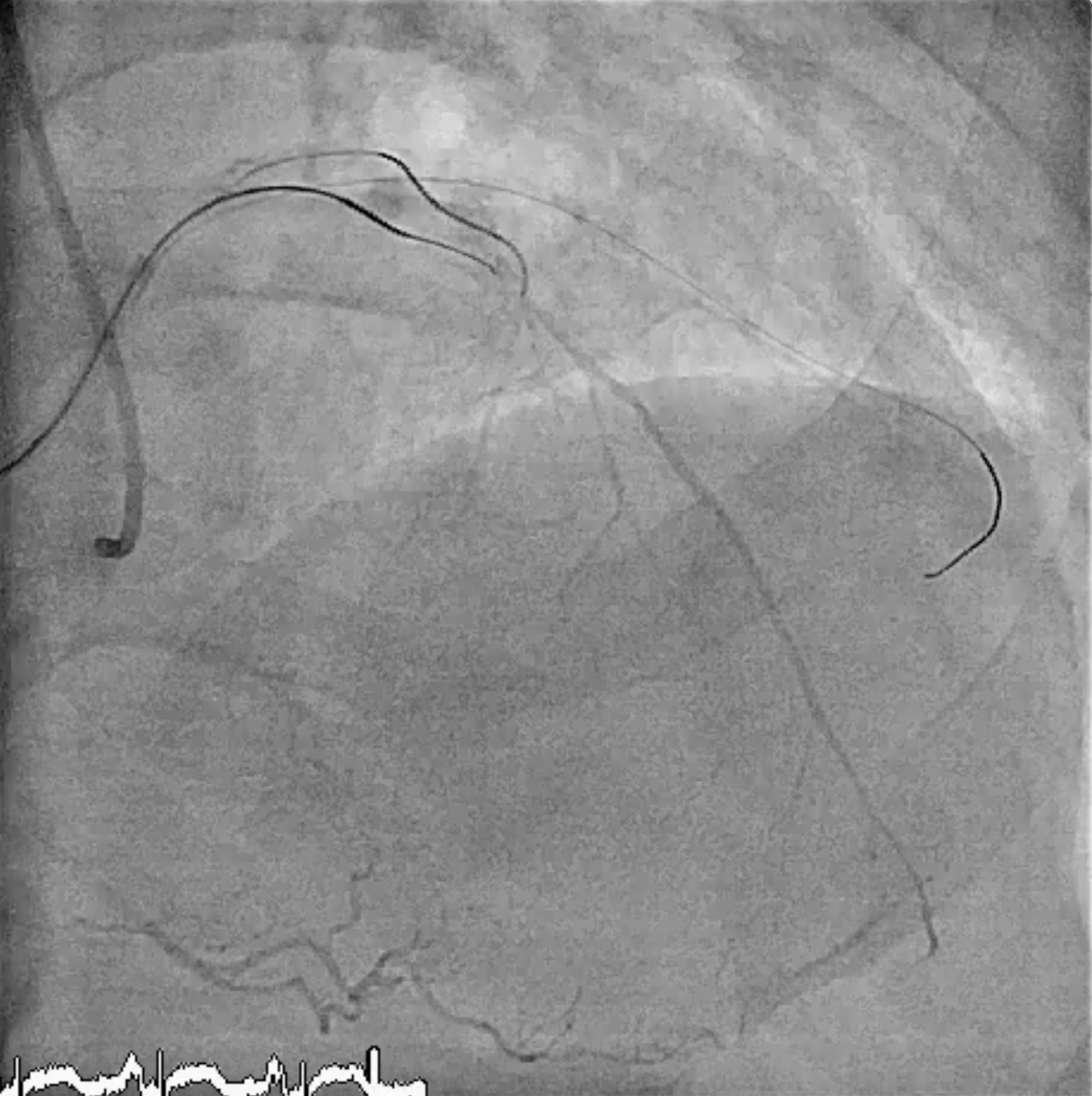
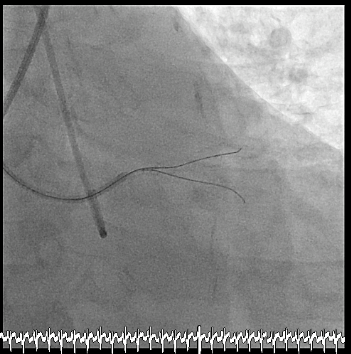
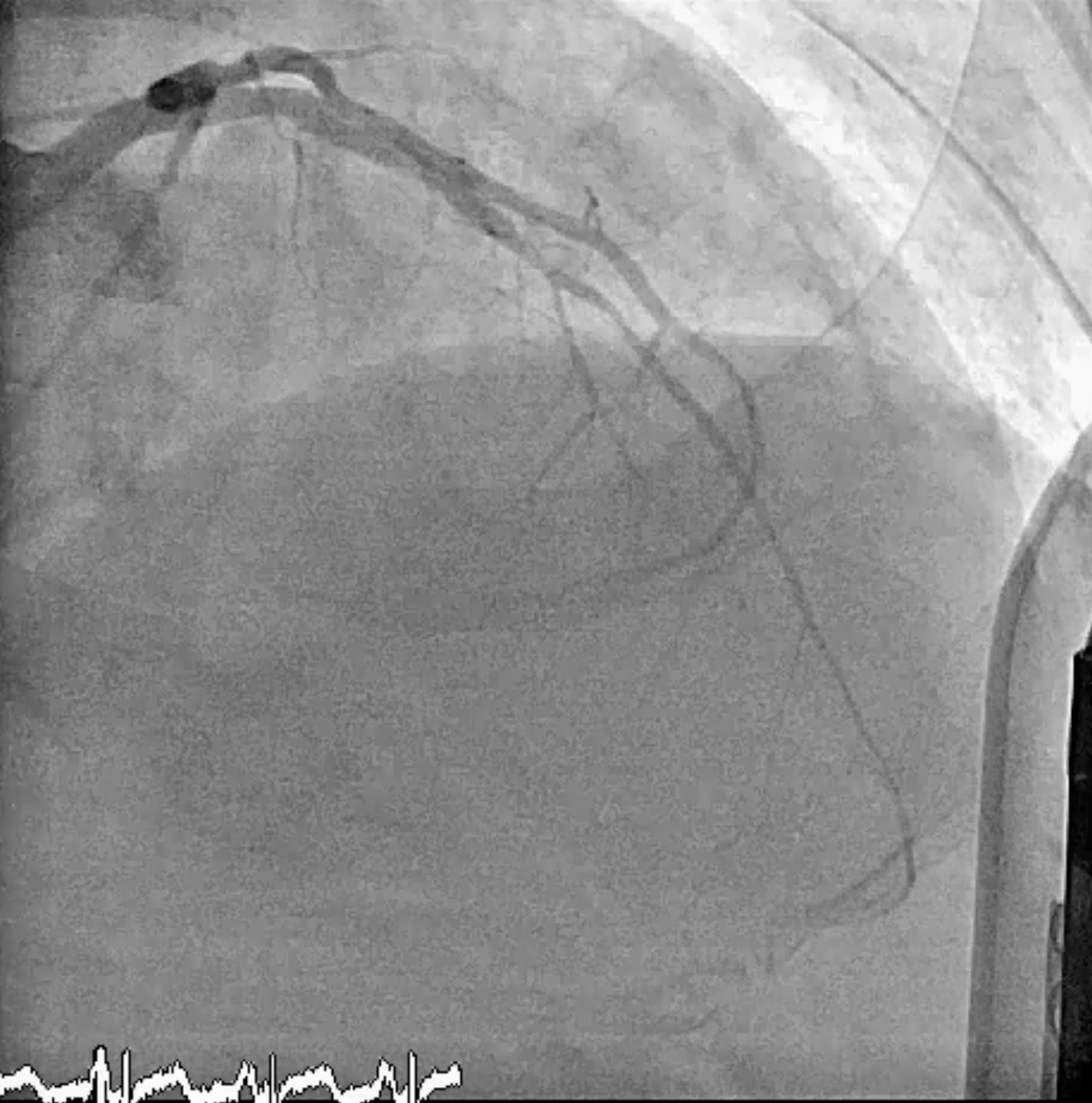
The CTO extended to LAD-Os might probably be an injury to proximal LAD in the first time procedure. After identification of LAD CTO entry cap with IVUS, UB3 GW was to LAD-D1 with assistance from Sasuke MC. IVUS identified UB3 GW was in true lumen of LAD-D1. We again identified LAD CTO entry cap with IVUS pullback from D1. A Conquest Pro 12 GW was successfully advanced to LAD-D with the assistance from Sasuke MC. We confirmed GW in true lumen of LAD from contracollateral angiography and IVUS. Subsequently dilated the CTO segment and a DES was deployed from LAD ostium to distal. We started to revascularize RCA with primary retrograde approach as planned. Retrograde collateral channel of LCX-OM was crossed by Sion GW with APT 1.7 Fr MC to PDA. We changed GW to XT-R which was advanced further to RCA-D but stopped by hard CTO lesion. We started antegrade approach with XT-R which was supported by APT 2.6 Fr MC. Antegrade XT-R reached distal RCA but MC couldn't advance down due to calcified lesion at middle RCA. We upgraded retrograde GW to Gaia 2nd then conquest pro 12 GW which successfully progressed to antegrade GC by kissing wire technique. RG3 was externalized. A 2.5 x 38 mm and a 3.0 x 38mm DES were deployed from RCA-D to RCA-P. Total flouroscopy time was 113 minutes. Total contrast amount was 195 ml. Hospital course was smooth and discharged two days later.


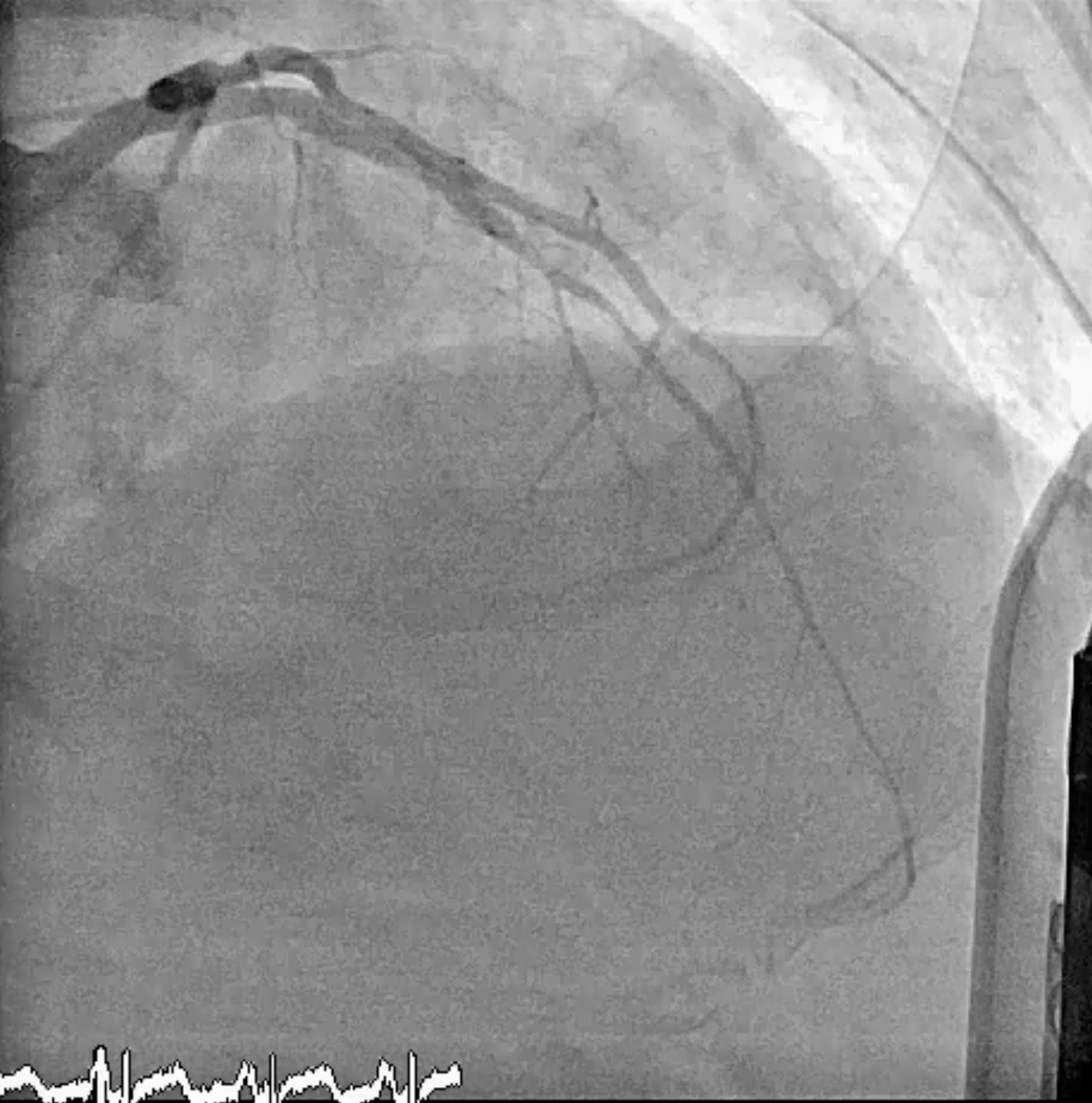


Case Summary
It is possible to complete revascularization of double CTOs in one stage procedure if well planned. There are some areas to be improved such as how to treat LAD-D1 no reflow situation, how to improved LAD post stenting underexpansion. The patient not followed at our out patient clinic regularly.

