Lots of interesting abstracts and cases were submitted for TCTAP 2024. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-182
Intravascular Ultrasound in Cardioembolic Myocardial Infarction - Seeing Is Believing
By Wee Meng Ng, Ki Fung Cliff Li
Presenter
Wee Meng Ng
Authors
Wee Meng Ng1, Ki Fung Cliff Li1
Affiliation
Tan Tock Seng Hospital, Singapore1,
View Study Report
TCTAP C-182
Coronary - Imaging & Physiology - Invasive Imaging (IVUS, OCT, NIRS, VH, etc)
Intravascular Ultrasound in Cardioembolic Myocardial Infarction - Seeing Is Believing
Wee Meng Ng1, Ki Fung Cliff Li1
Tan Tock Seng Hospital, Singapore1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
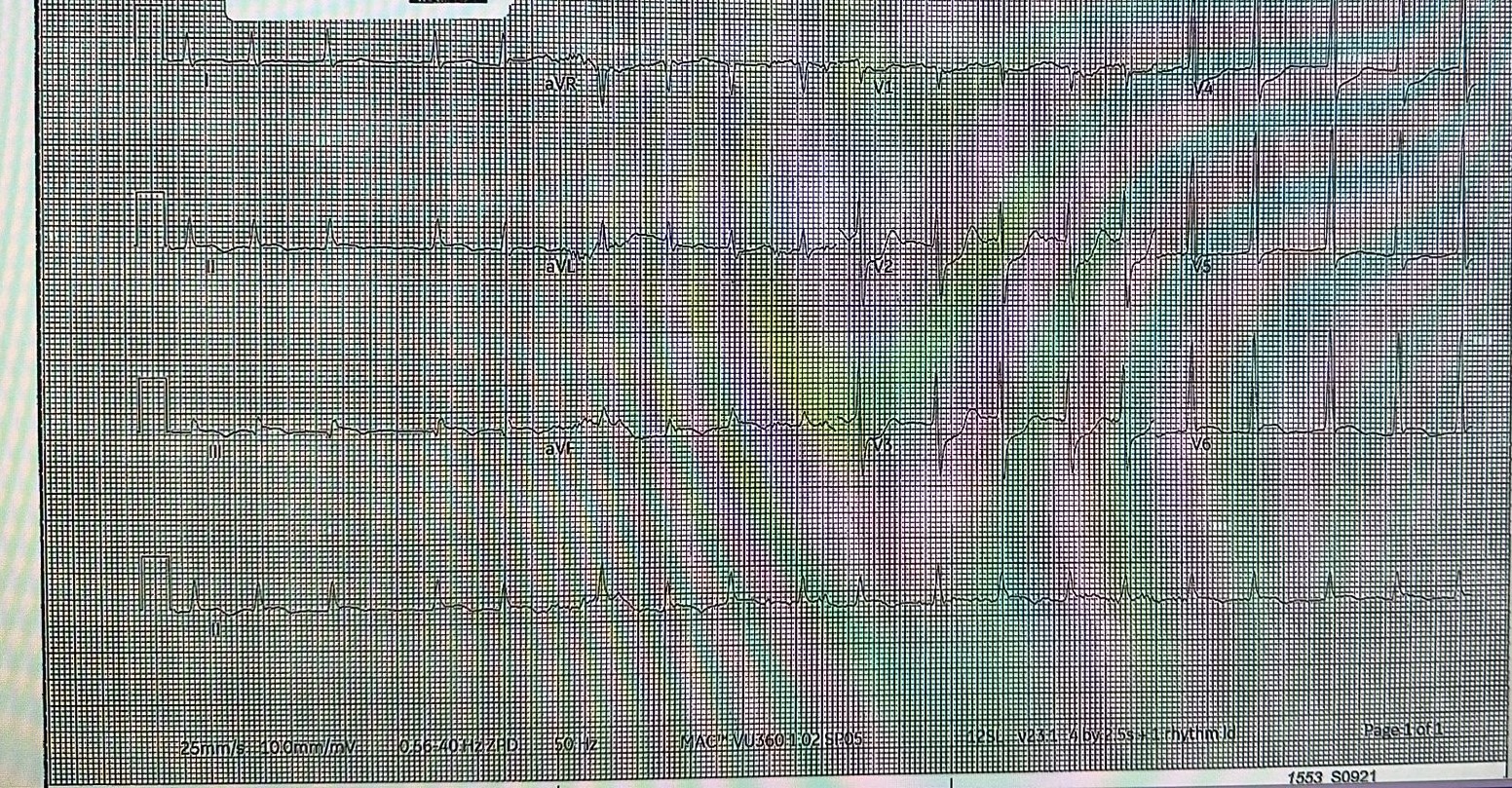
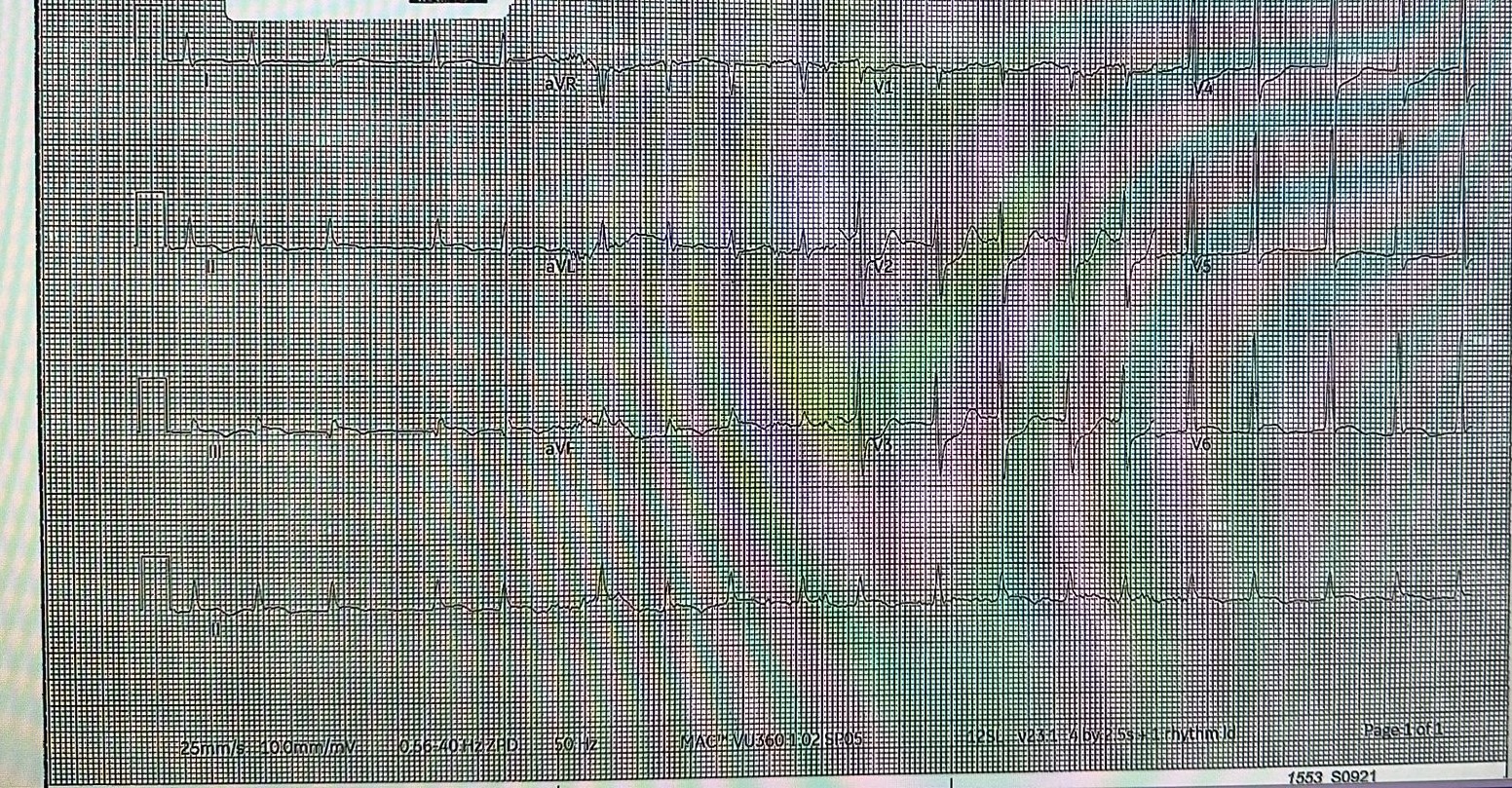
An 80 year old male presented with acute onset chest pain. His past medical history included atrial fibrillation - anticoagulated with Apixaban. A previous echocardiogram done in 2015 showed normal left ventricular function, with moderately dilated right and left atrium. Electrocardiogram done upon arrival to the Emergency Room showed inferoposterior ST-elevation myocardial infarction.
Relevant Test Results Prior to Catheterization
Initial blood tests including renal function and complete blood count were unremarkable.
Relevant Catheterization Findings
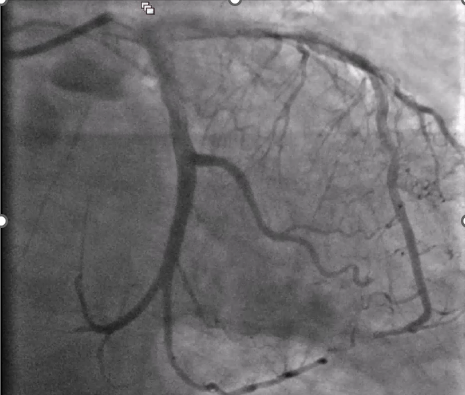
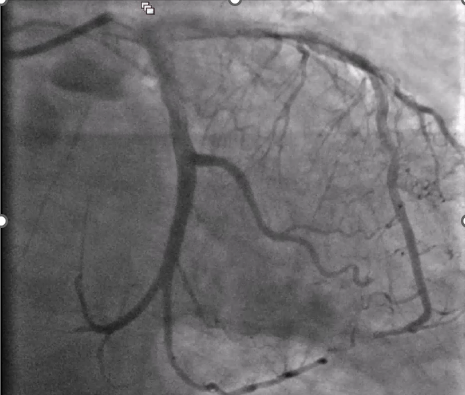
Coronary angiogram demonstrated a co-dominant system. The Left Main was free of significant disease. The Left Anterior Descending (LAD) artery had minor disease, with a clot in the apical LAD. There was a distal first diagonal artery (D1) clot. The Left Circumflex artery (LCx) showed a distal 100% acute thrombotic occlusion. More clots were also noted in the distal OM1 and OM2.
The Right Coronary Artery (RCA) was free of significant disease.


The Right Coronary Artery (RCA) was free of significant disease.


Interventional Management
Procedural Step
Given the multiple clots noted in both the LAD and LCx systems - the overall impression was Cardioembolic Myocardial Infarction. Via the same right radial access, we engaged the left system with a 6Fr XB 3.5 guide, and wired the distal LCx with a Sion blue guidewire.
We opted to start with a manual aspiration catheter. 2 runs were performed which yielded small clots, restoring partial flow in the distal LCx. We also delivered intra-coronary boluses of Integrillin.
We then decided to switch to mechanical aspiration - with the Penumbra CAT Rx system. Here, we opted for a prolonged dwell time of 90 seconds. Under continuous aspiration, the catheter was withdrawn and yielded a massive clot.
We proceeded for a 2nd run with the aspiration catheter - this time advancing more distally. Following this, an angiogram shot now showed restoration of TIMI3 flow.
We then proceeded to perform an IVUS run with the Opticross HD catheter - which demonstrated no significant plaque or plaque rupture/dissection within the culprit segment. The minimal lumen area was also measured to be 4.5mm2. The intravascular imaging findings gave us the confidence to perform Thrombectomy-only PCI and avoid unnecessary ballooning/stenting.
A repeat electrocardiogram now demonstrated improvement in ST-segment changes, and the patient was sent back to the Cardiology High Dependency unit for monitoring


We opted to start with a manual aspiration catheter. 2 runs were performed which yielded small clots, restoring partial flow in the distal LCx. We also delivered intra-coronary boluses of Integrillin.
We then decided to switch to mechanical aspiration - with the Penumbra CAT Rx system. Here, we opted for a prolonged dwell time of 90 seconds. Under continuous aspiration, the catheter was withdrawn and yielded a massive clot.
We proceeded for a 2nd run with the aspiration catheter - this time advancing more distally. Following this, an angiogram shot now showed restoration of TIMI3 flow.
We then proceeded to perform an IVUS run with the Opticross HD catheter - which demonstrated no significant plaque or plaque rupture/dissection within the culprit segment. The minimal lumen area was also measured to be 4.5mm2. The intravascular imaging findings gave us the confidence to perform Thrombectomy-only PCI and avoid unnecessary ballooning/stenting.
A repeat electrocardiogram now demonstrated improvement in ST-segment changes, and the patient was sent back to the Cardiology High Dependency unit for monitoring


Case Summary
Given the patient's history of Atrial Fibrillation, as well as angiographic findings of multiple clots in different coronary arteries, this raised suspicion of a cardioembolic MI.
As such, the operator's diligence in performing Intravascular Ultrasound (IVUS) directly demonstrated no plaque/plaque rupture/dissection within the culprit segment - providing the team confidence in performing Thrombectomy-only PCI and to defer ballooning/stenting, which allowed us to avoid the much feared distal embolisation/no re-flow phenomenon.
In conclusion, the use of intravascular imaging techniques such as IVUS is of great importance in the management of suspected cardioembolic myocardial infarction.
As such, the operator's diligence in performing Intravascular Ultrasound (IVUS) directly demonstrated no plaque/plaque rupture/dissection within the culprit segment - providing the team confidence in performing Thrombectomy-only PCI and to defer ballooning/stenting, which allowed us to avoid the much feared distal embolisation/no re-flow phenomenon.
In conclusion, the use of intravascular imaging techniques such as IVUS is of great importance in the management of suspected cardioembolic myocardial infarction.

