Lots of interesting abstracts and cases were submitted for TCTAP 2024. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-169
Worse Than Being Blind Is Having Sight but No Vision. A Challenging Situation: Left Main PCI in Patient With Severe Contrast Media Reaction.
By Korakoth Towashiraporn, Nattawut Wongpraparut, Songpop Chongthaveepol, Wisakha Anusorn
Presenter
Korakoth Towashiraporn
Authors
Korakoth Towashiraporn1, Nattawut Wongpraparut2, Songpop Chongthaveepol3, Wisakha Anusorn1
Affiliation
Her Majesty Cardiac Center Faculty of Medicine Siriraj Hospital, Mahidol University, Thailand1, Siriraj Hospital, Mahidol University, Thailand2, Golden Jubilee Medical Center, Mahidol University, Thailand3,
View Study Report
TCTAP C-169
Coronary - Imaging & Physiology - Invasive Imaging (IVUS, OCT, NIRS, VH, etc)
Worse Than Being Blind Is Having Sight but No Vision. A Challenging Situation: Left Main PCI in Patient With Severe Contrast Media Reaction.
Korakoth Towashiraporn1, Nattawut Wongpraparut2, Songpop Chongthaveepol3, Wisakha Anusorn1
Her Majesty Cardiac Center Faculty of Medicine Siriraj Hospital, Mahidol University, Thailand1, Siriraj Hospital, Mahidol University, Thailand2, Golden Jubilee Medical Center, Mahidol University, Thailand3,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
A 75-year-old female with hypertension, dyslipidemia, and paroxysmal atrial fibrillation presented with angina on exertion Canadian Cardiovascular Society grade 2. Her physical examination was within normal limits. She underwent an exercise stress test that demonstrated positive for ischemia at 7.0 METs (figure 1).


Relevant Test Results Prior to Catheterization
She had normal left ventricular contraction with normal wall motion on transthoracic echocardiogram. Her blood chemistry results were as follows: hemoglobin 12.5 g/dl, hematocrit 39.2%, and serum creatinine 0.79 mg/dl. She was transferred to our institution for coronary angiography.
Relevant Catheterization Findings
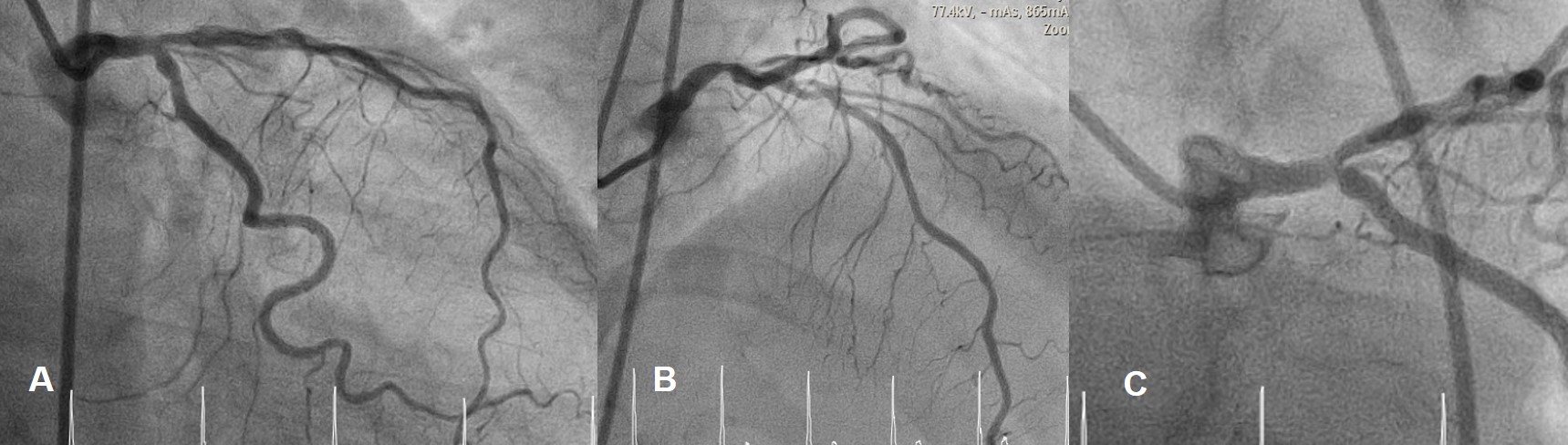
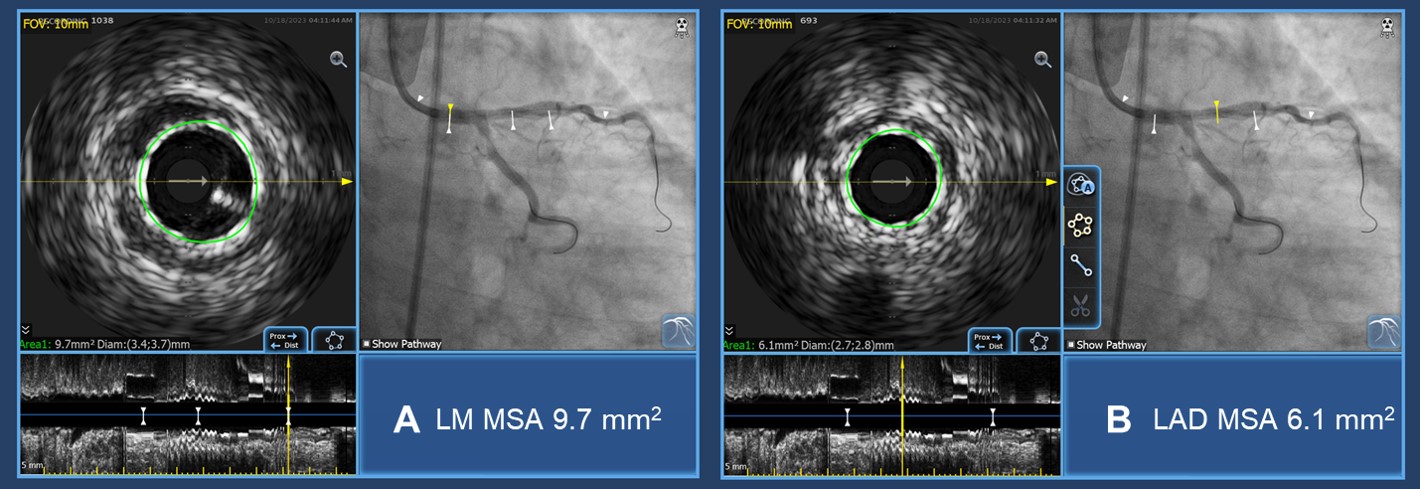
Her coronary angiography revealed significant stenosis at distal left main (LM) and ostial to proximal left anterior descending (LAD) artery. She had borderline stenosis of ostial left circumflex (LCX) artery (Figure 2 A-C). We planned to perform intravascular (IVUS) guided percutaneous coronary intervention (PCI).
Interventional Management
Procedural Step
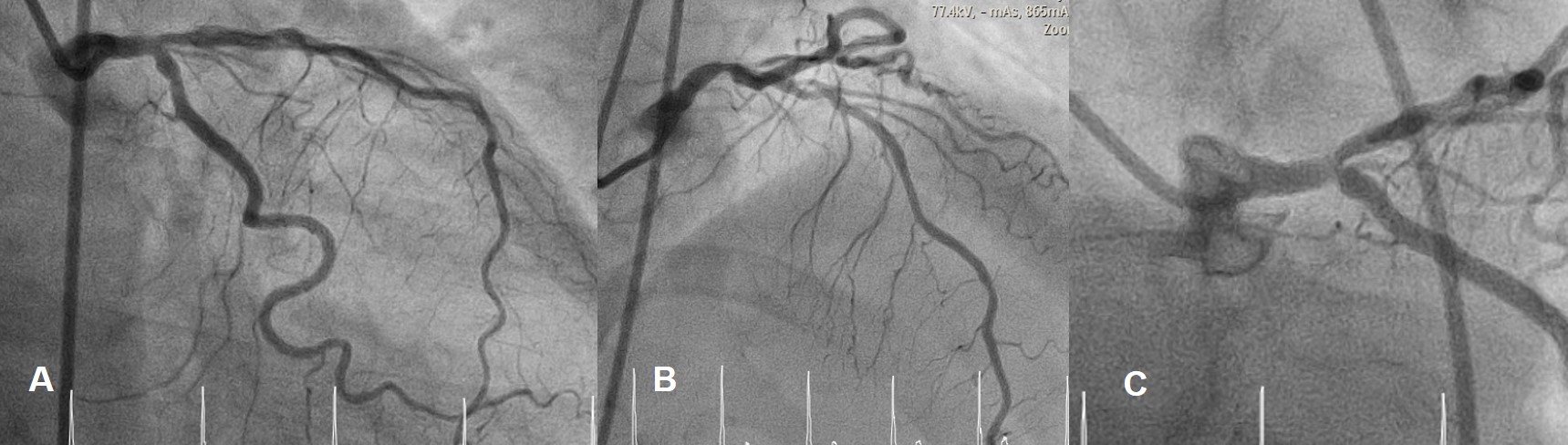
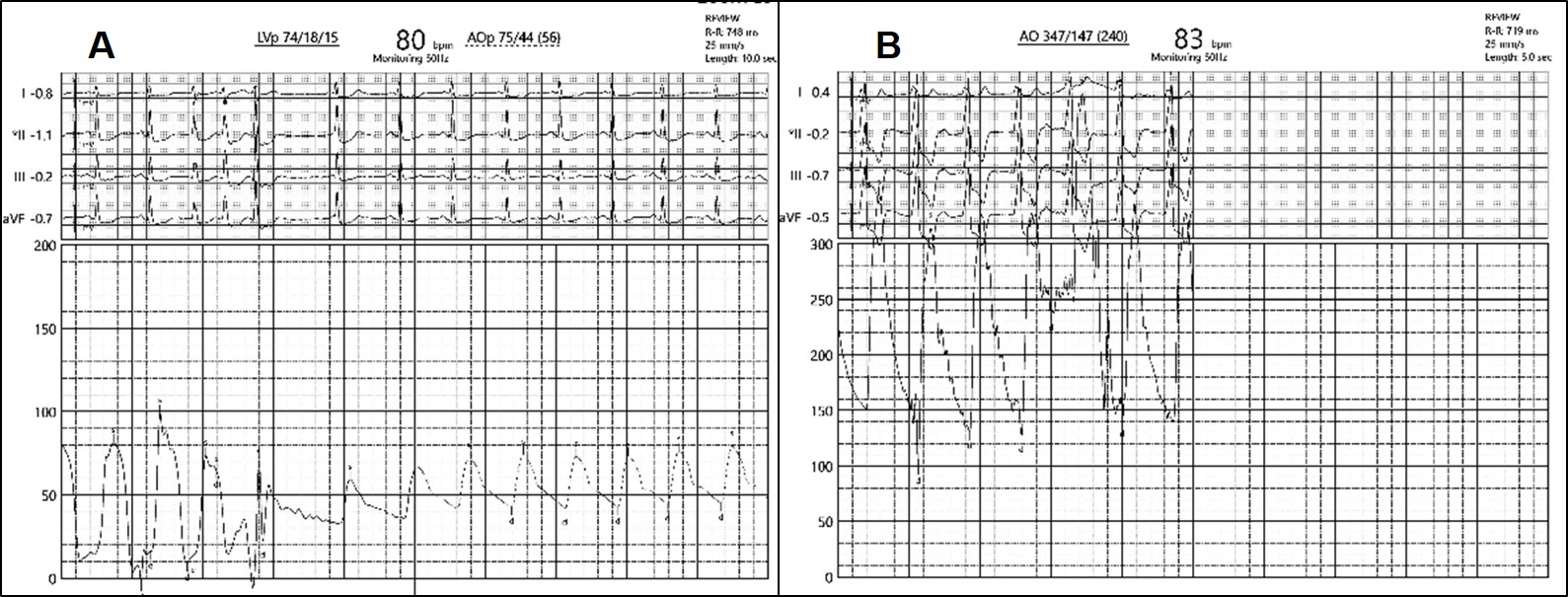
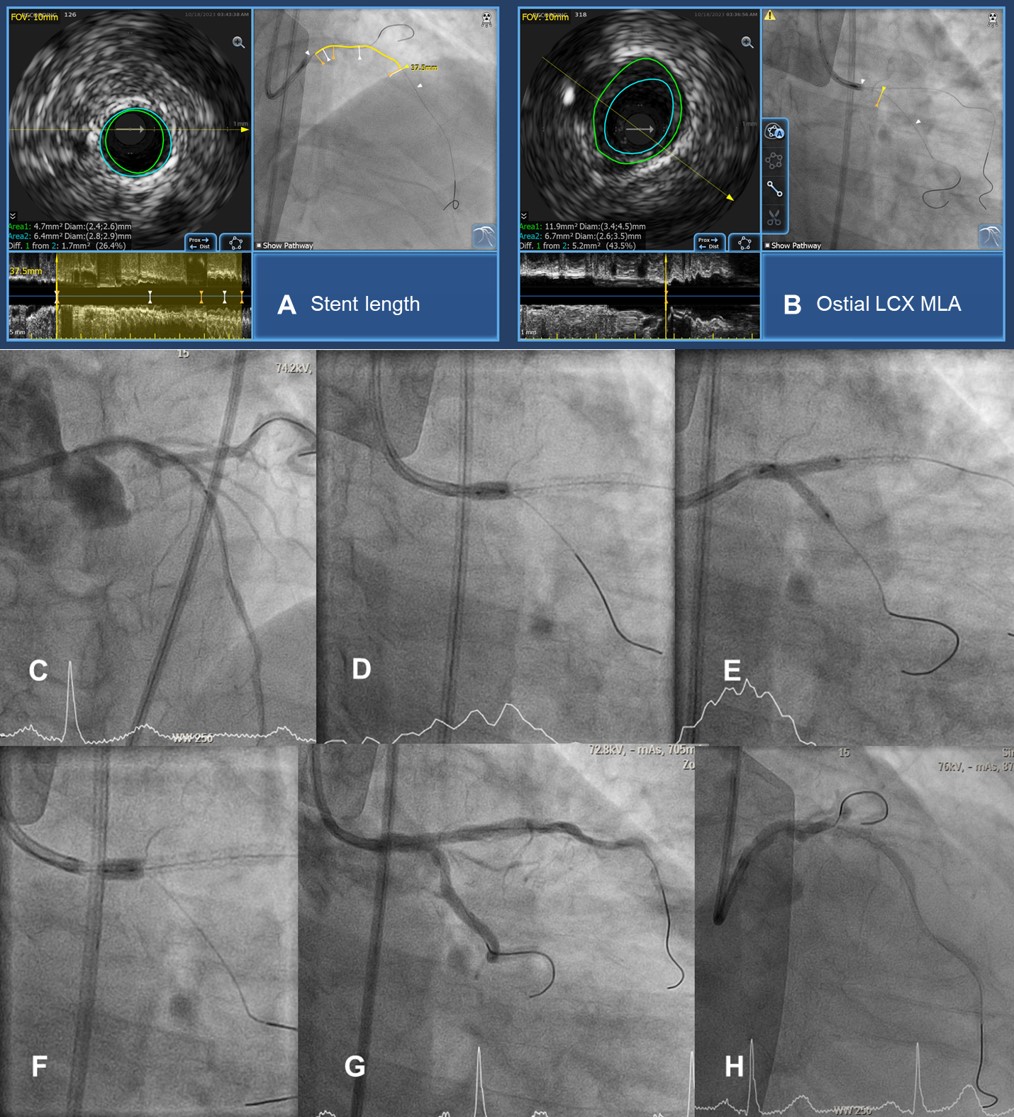
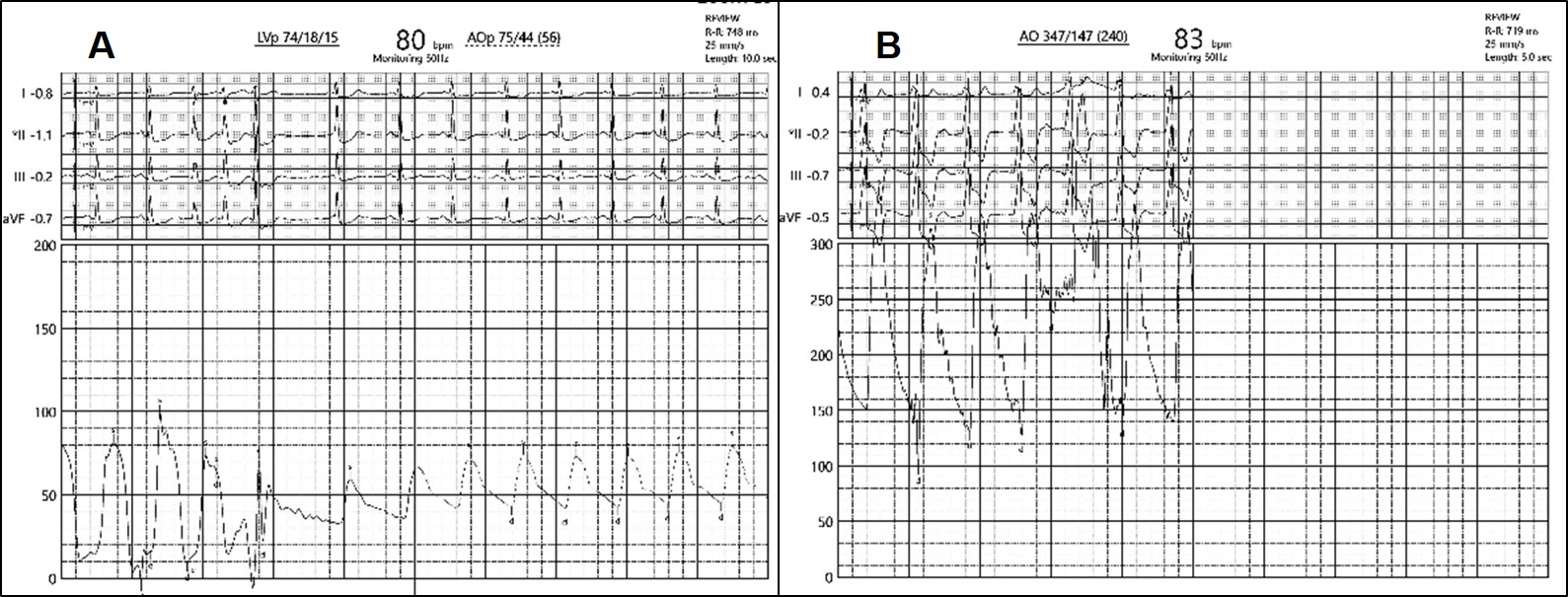
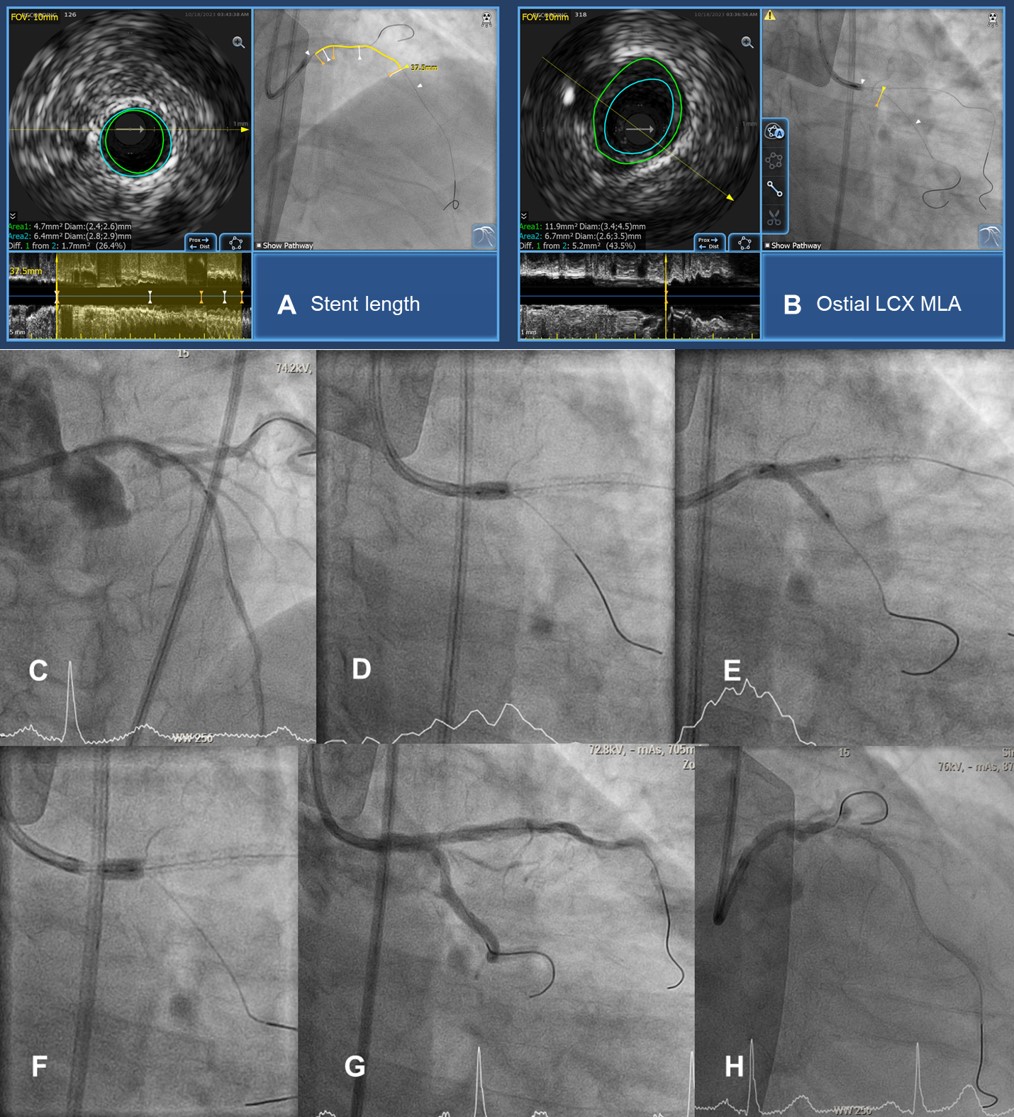
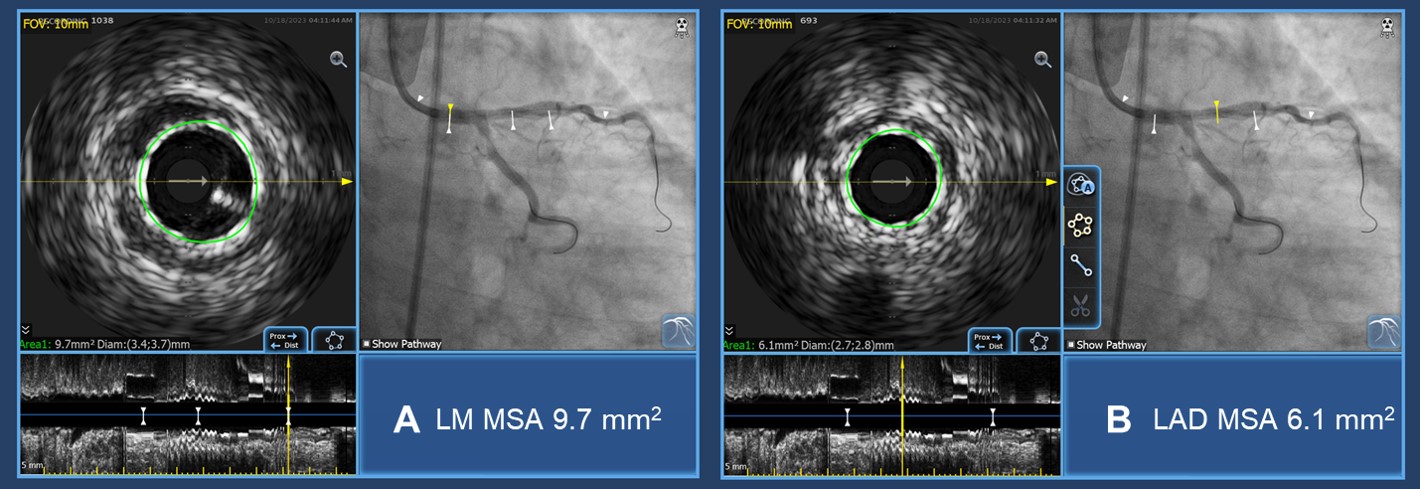
Before PCI, the patient developed severe hypotension. Left ventricular end-diastolic pressure (LVEDP) was immediately recorded (figure 3A). After brief resuscitation, her blood pressure was rising to 347/147 mmHg (figure 3B). As a result, the procedure was terminated. After immunologic testing, the diagnosis was non-IgE mediated hypersensitivity from iopromide. Therefore, we planned to defer PCI. Unfortunately, during the follow-up period, she developed acute decompensated heart failure. After a discussion with the patient and our immunologist, we agreed to perform PCI with pre-medication to prevent contrast media reactions. Using the ultralow-contrast (ULC) -PCI strategy, we use IVUS for planning the stenting strategy. IVUS demonstrated the distal reference vessel size was 2.8x2.9 mm and the total stent length from the distal landing zone to ostial LM was 37.5 mm (figure 4A). As there was non-significant stenosis at ostial LCX (figure 4B), we planned to perform a provisional stenting technique for distal left main bifurcation (figure 4C-F). A 2.5x38 mm drug-eluting stent was deployed from ostial LM to mid-LAD. Proximal optimization technique (POT) was done using a 4.0 mm balloon. Kissing balloon inflation and final POT was done, respectively. Final angiography showed good results (figure 4G-H). Final IVUS demonstrated good stent expansion and opposition (figure 5A, B). The total amount of contrast (iodixanol) was 7 cc. We could discharge the patient the day after, uneventful.
Case Summary
1. Severe contrast media reaction should be one of the differential diagnoses of intraprocedural hypotension. This reaction could lead to morbidity and mortality of the patient. Therefore, it requires immediate appropriate management.2. Not only hypotension but also hypertensive crisis could be a manifestation of severe contrast media reaction.3. The ULC-PCI strategy does not mean only using "ultra-low" contrast media during PCI. Nevertheless, this strategy also uses multimodality equipment such as fluoroscopic findings, intravascular imaging, and physiologic studies to guide the procedure. Accordingly, the ULC-PCI strategy can be performed in selected complex PCI cases.

