Lots of interesting abstracts and cases were submitted for TCTAP 2024. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-153
Triple Troubles- Migrated Stent, Calcified Vessels and Thin Cap Fibroatheroma
By Chun Yu Fung, Ho Lam
Presenter
Chun Yu Fung
Authors
Chun Yu Fung1, Ho Lam1
Affiliation
Tuen Mun Hospital, Hong Kong, China1,
View Study Report
TCTAP C-153
Coronary - High-Risk Intervention (Diabetes, Heart Failure, Renal Failure, Shock, etc)
Triple Troubles- Migrated Stent, Calcified Vessels and Thin Cap Fibroatheroma
Chun Yu Fung1, Ho Lam1
Tuen Mun Hospital, Hong Kong, China1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
A 70-year-old gentleman presented to us for chest pain for around 12 hours.
ECG on admission show ST segment elevation over inferior leads.
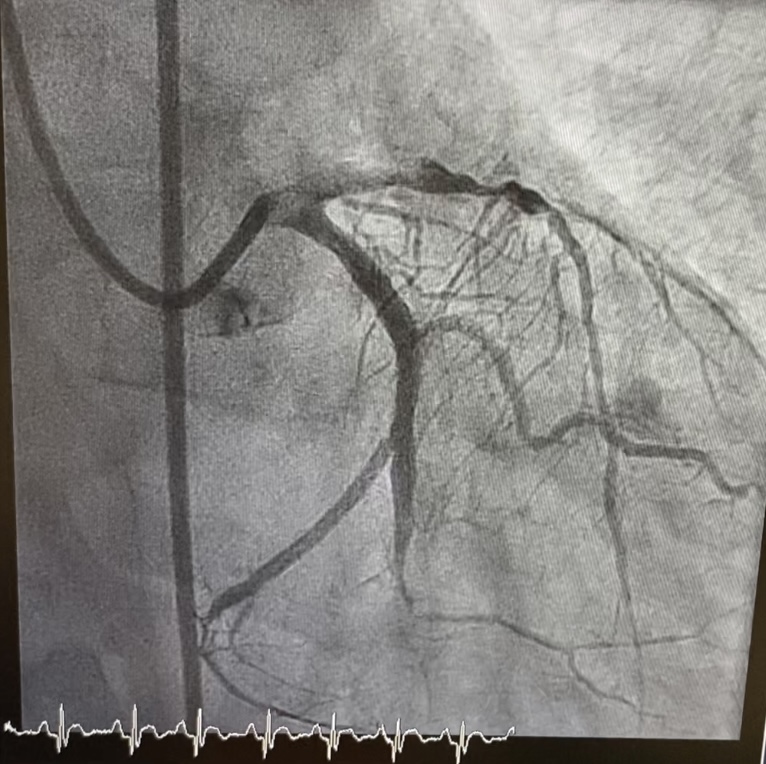
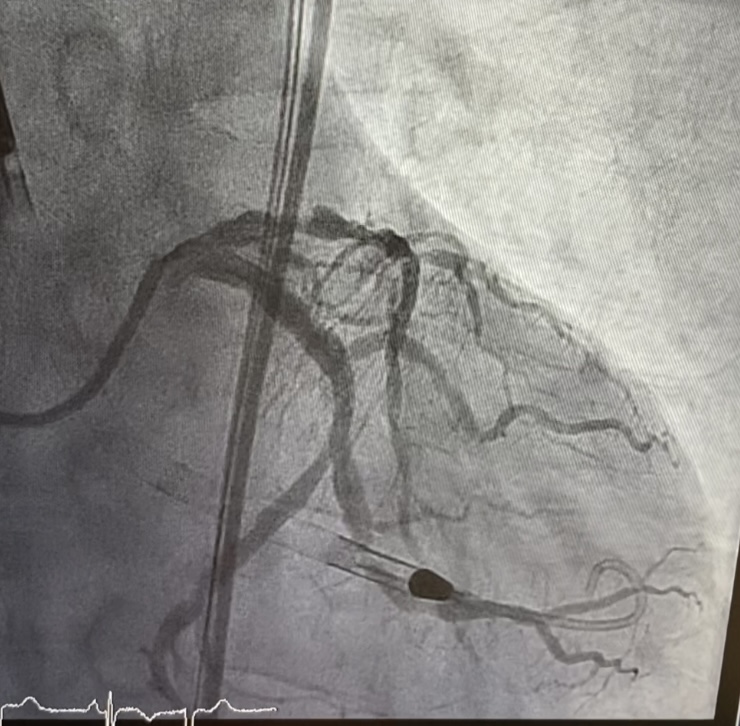
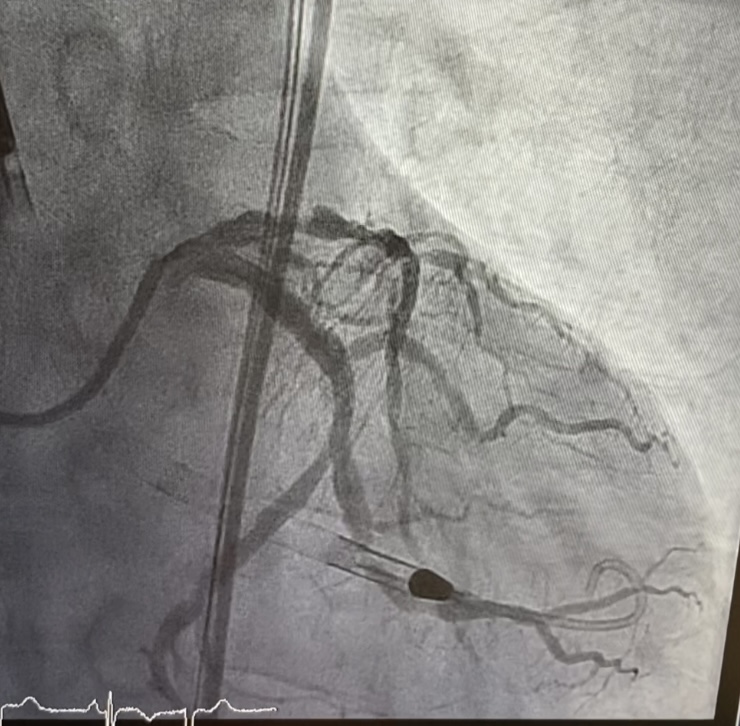
PPCI was done on admission, IRA=mLCx, PCI to m-dLCx/OM2 bifurcation was done
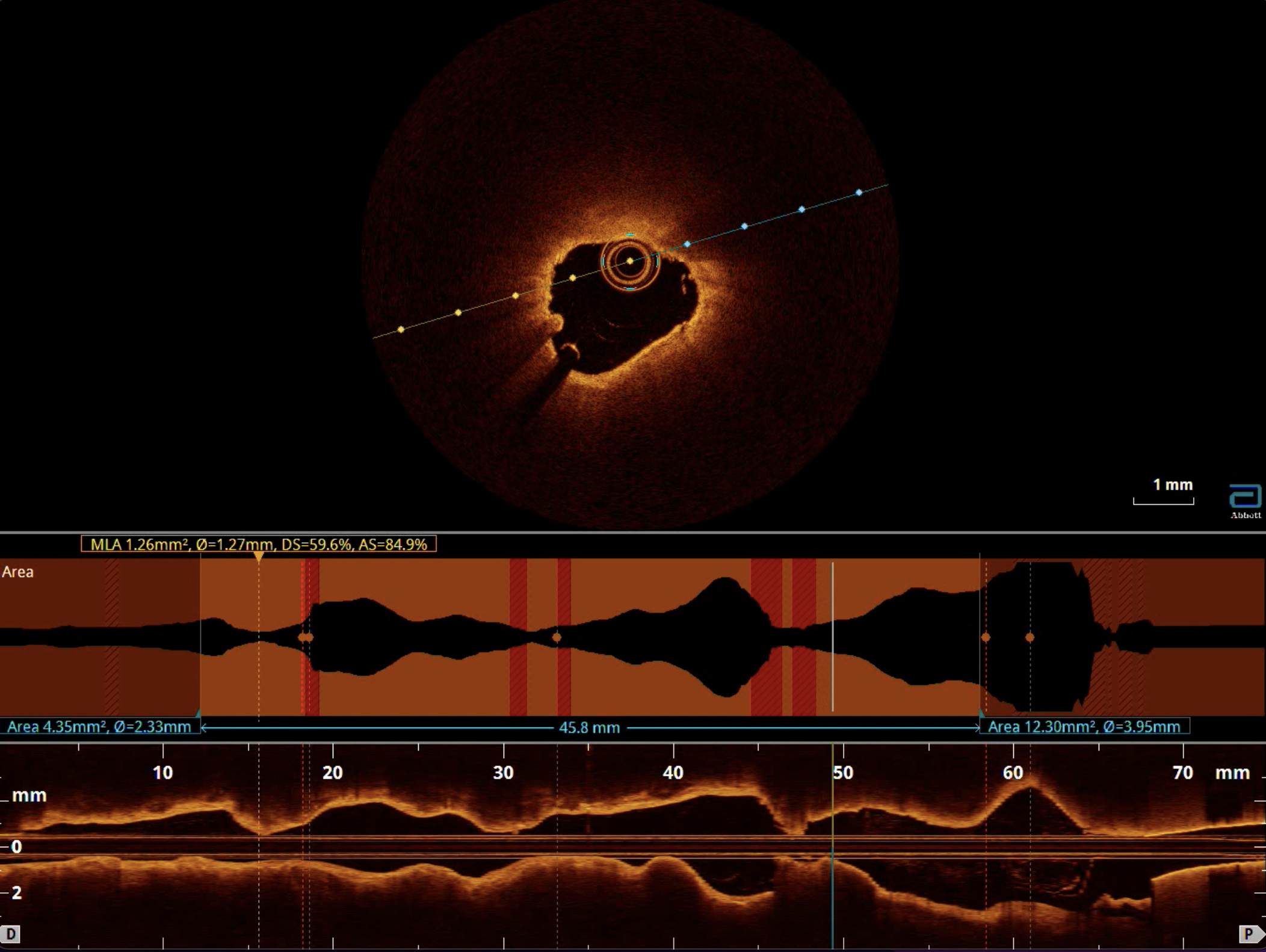
IVUS show good stent expansion and apposition
Cardiogenic shock and APO post PPCI, echo: LVEF 32.5%
stabilised with diuretics and inotropic support
arranged impella assisted stage PCI for diffuse calcified LAD lesion
Relevant Test Results Prior to Catheterization
Echo Dilated LVImpaired LV systolic function. LVEF 32.5% by Simpson's. Global hypokinesiaSatisfactory RV systolic function Mild AR/ MR/ TRNo pericardial effusion / LV thrombus
peak CK 800. TnI > 50000
peak CK 800. TnI > 50000
Relevant Catheterization Findings
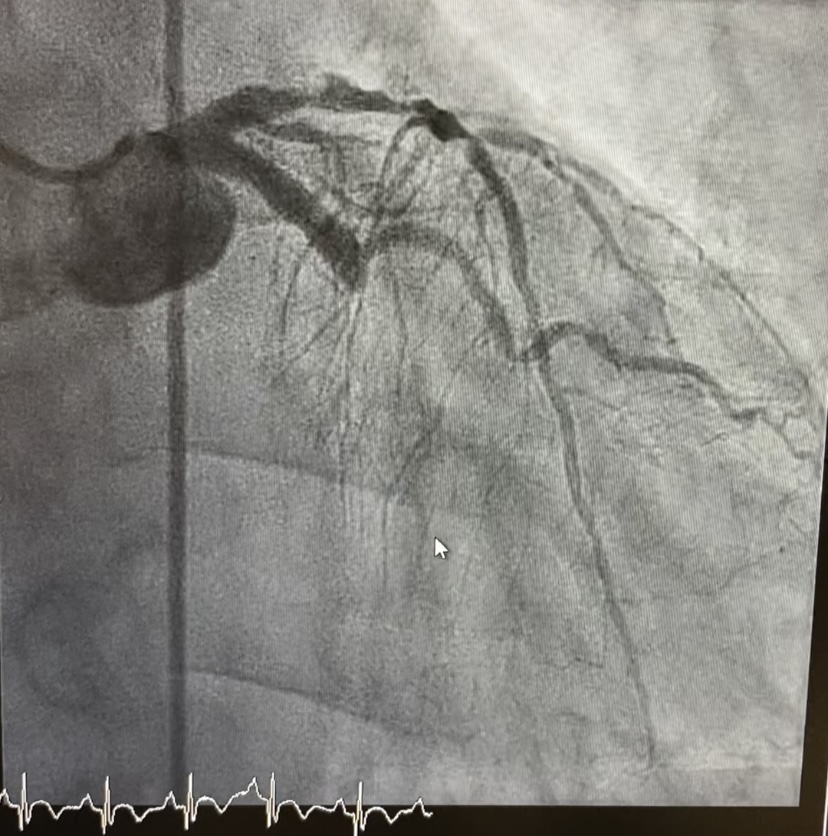
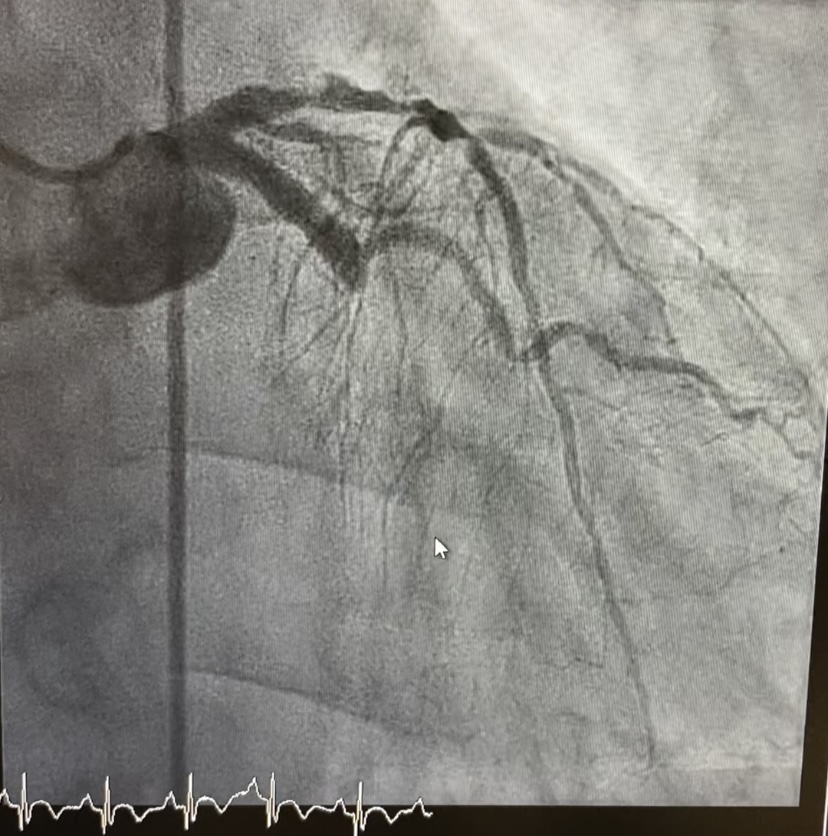
restudy Coro after 6 days LM normal LAD pLAD 80% disease followed by diffuse disease along whole LAD and another 90% lesion over mLAD, calcified vesselsignificant increase Lcx vessel size compared with previous Coro


Interventional Management
Procedural Step
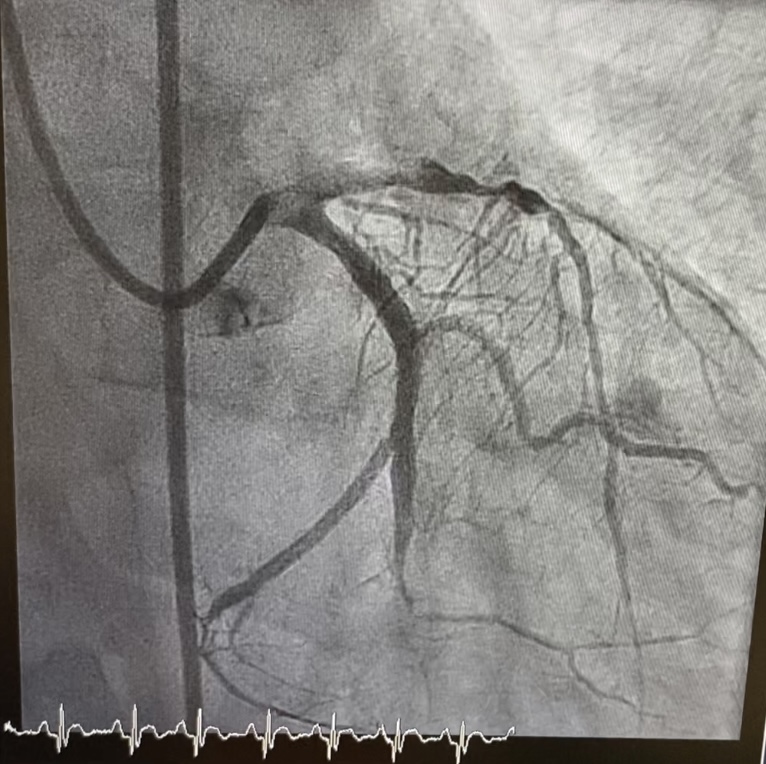
Decided for optimisation of LCx/ OM2 bifurcation first
PCI to p-mLAD
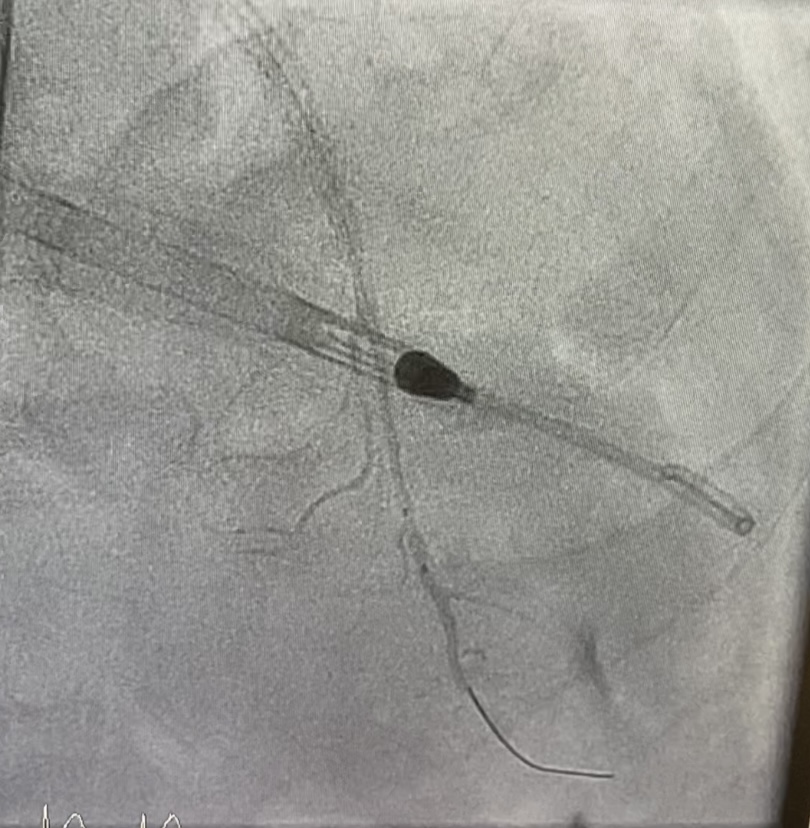
rotational atherectomy done at p-mLAD
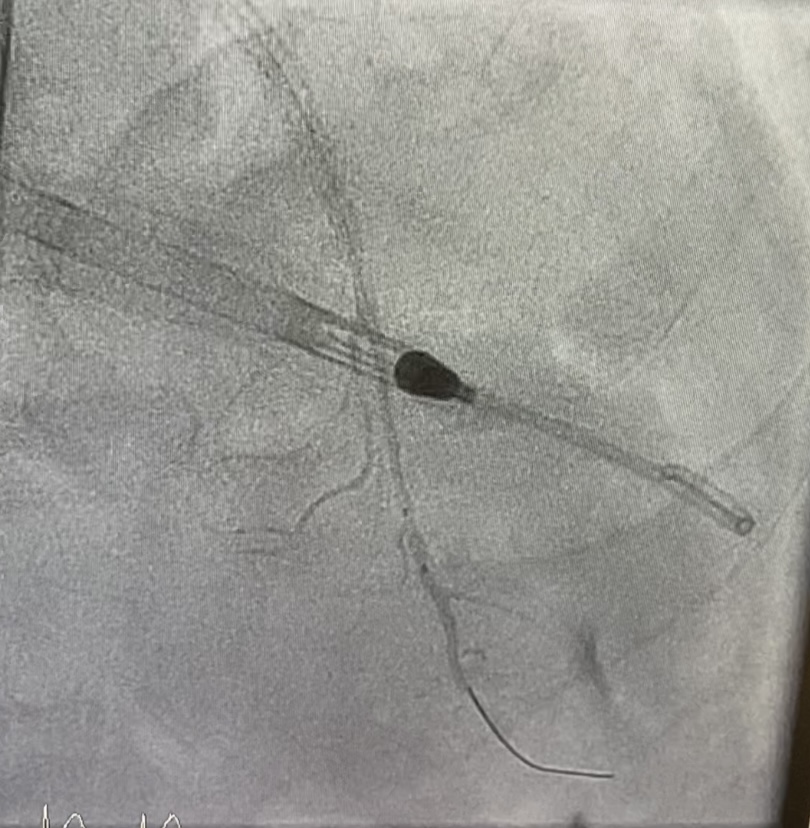

PCI to p-mLAD
rotational atherectomy done at p-mLAD

Case Summary
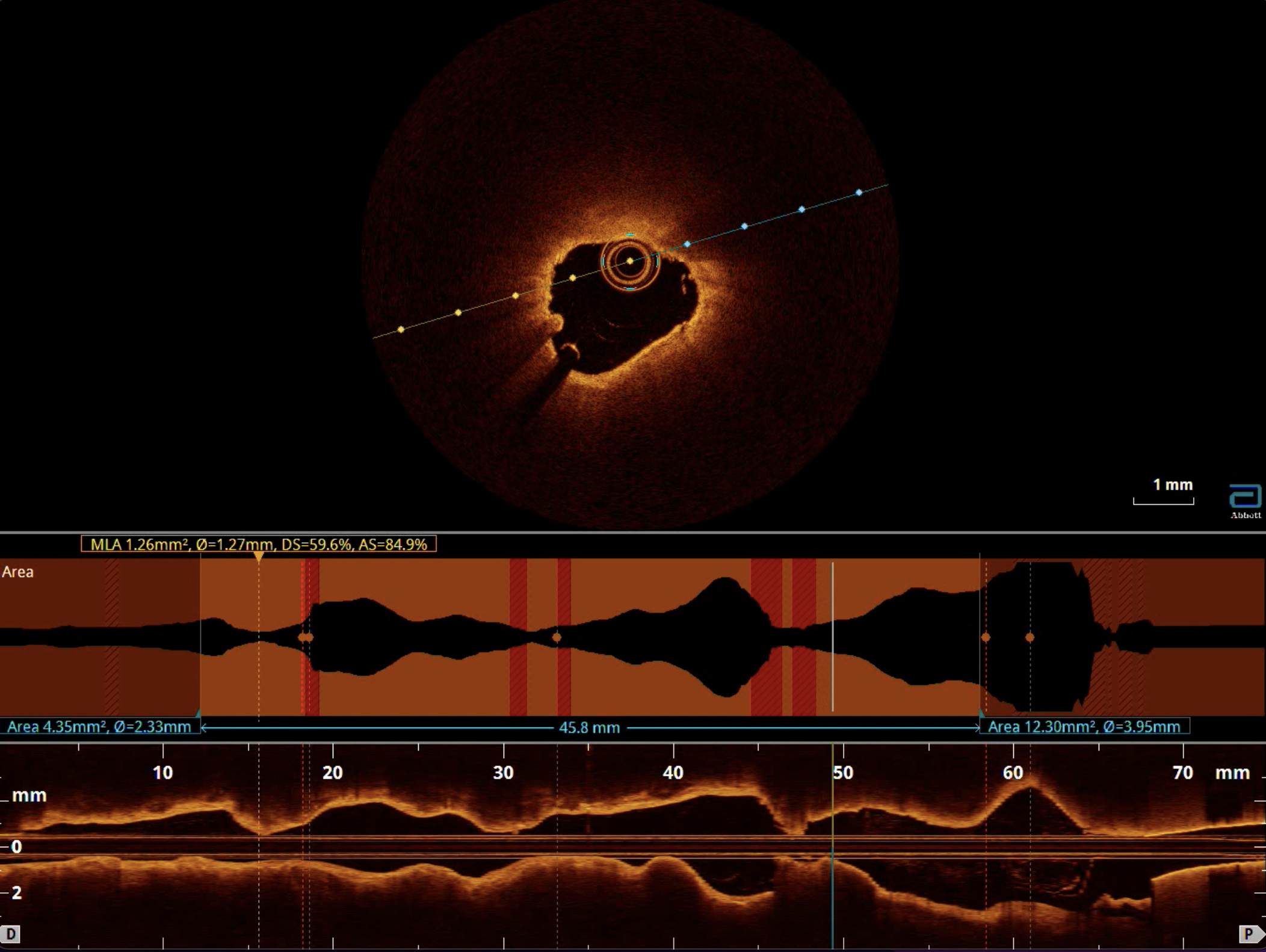
TCFA/ lipid rich plaque represent vulnerable lesion, high risk of no reflow of stenting due to lipid emboli
DDx of no reflow post-stenting
DDx of no reflow post-stenting
rotational atherectomy at p-mLAD calcified lesion is crucial to ensure successful delivery of the thrombectomy system and management of lipid embolisation

