Lots of interesting abstracts and cases were submitted for TCTAP 2024. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-135
Unexpected Left Main Coronary Occlusion in the Course of Routine Coronary Angiography
By Dimas Rio Balti
Presenter
Dimas Rio Balti
Authors
Dimas Rio Balti1
Affiliation
Ubaya Hospital, Indonesia1,
View Study Report
TCTAP C-135
Coronary - Complication Management
Unexpected Left Main Coronary Occlusion in the Course of Routine Coronary Angiography
Dimas Rio Balti1
Ubaya Hospital, Indonesia1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
Mr. M, 58 years old, has been experiencing chest pain and shortness of breath for the past seven months. The symptoms improve with the rest and worsen during heavy physical activites. His medical story includes TIA (Transcient Ischemic Attack) and the risk factors are smoking and dyslipidemia. Blood pressure 116/70 mmHg, heart rate 71 bpm, respiration rate 18 breaths pre minute.




Relevant Test Results Prior to Catheterization
ECG: Sinus rhythm at 71 bpm with extensive anterior ischemia.
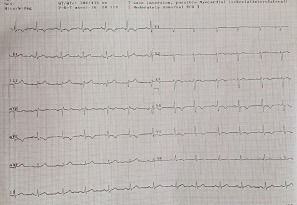
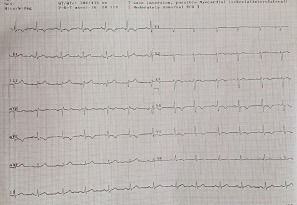
Relevant Catheterization Findings
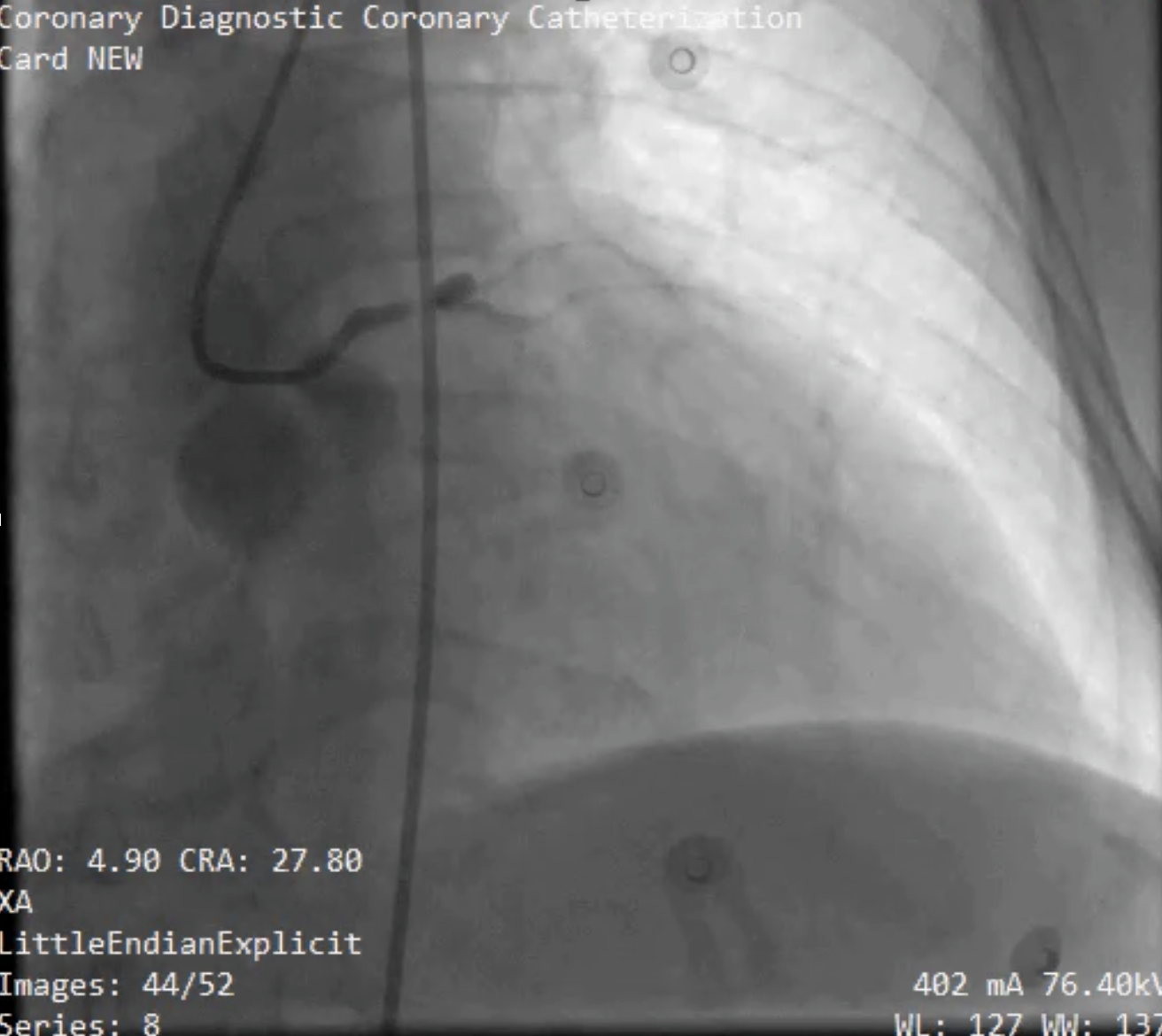
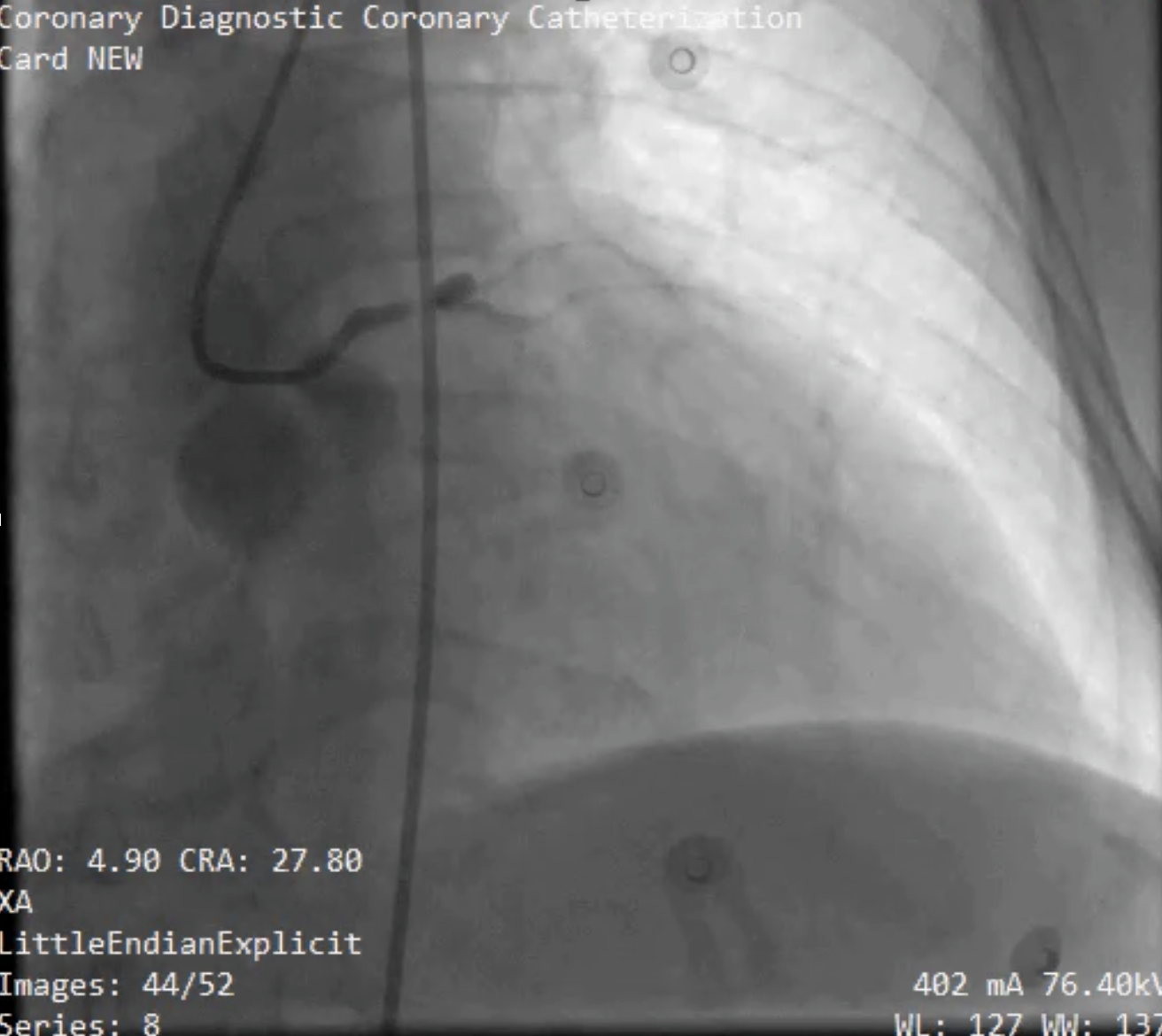
Stenosis of up to 50% at the mid-right coronary artery (RCA) and 75% at the distal RCA. During the left coronary angiography, regrettably, a complication arose, as a 99% stenosis was identified at the distal left main (LM) artery, accompanied by proximal LAD no-flow. To address these complications, revascularization was performed by wiring to the distal LAD, balloon angioplasty, rotablator treatment, and the placement of a stent extending from the distal LM to the distal LAD.






Interventional Management
Procedural Step
When complications arose, the patient exhibited restlessness, chest pain, and developed arrhythmias in the form of ventricular tachycardia (VT) and ventricular fibrillation (VF). Cardiopulmonary resuscitation was initiated while left coronary cannulation was achieved using an EBU 3.5 6 Fr catheter. Subsequently, successful wiring with a Runthrough hypercoat was performed, extending to the diagonal 1 branch. Ballooning was attempted in the distal left main (LM), but no flow was still observed. Consequently, a stent was placed from the distal LM to the proximal left anterior descending (LAD) artery, resulting in improved flow up to the mid LAD.
Efforts were made to advance the wire to the distal LAD using the same wire, but this was unsuccessful. A microcatheter with a Miracle 3 wire was then attempted, which also proved unsuccessful. Finally, the Conquest Pro wire was employed, successfully advancing to the distal LAD. Preparatory procedures with a balloon were attempted without success, leading to the decision to utilize a Rotablator with a burr size of 1.25. Subsequent ballooning and the placement of an additional stent from the mid to the distal LAD were carried out.


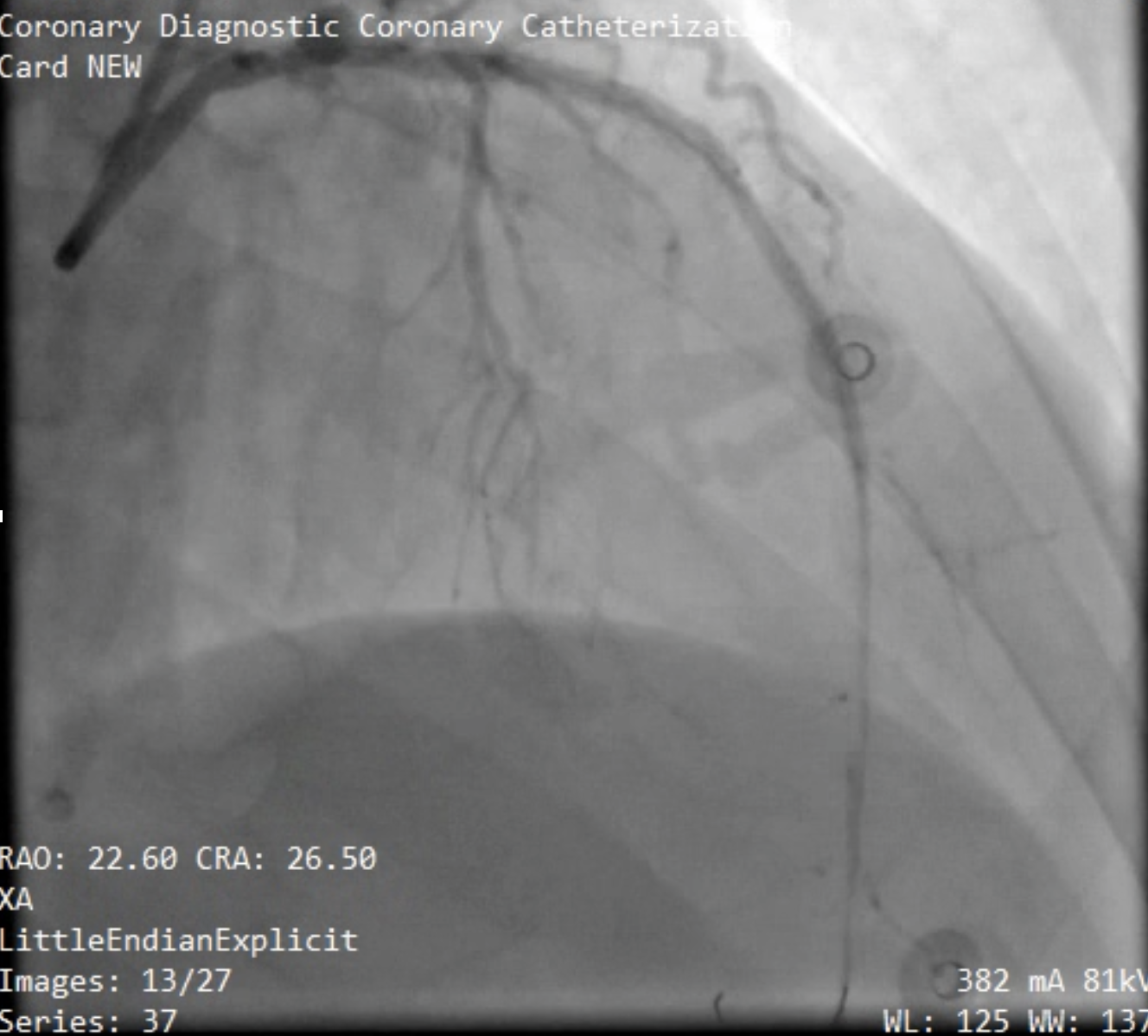
Efforts were made to advance the wire to the distal LAD using the same wire, but this was unsuccessful. A microcatheter with a Miracle 3 wire was then attempted, which also proved unsuccessful. Finally, the Conquest Pro wire was employed, successfully advancing to the distal LAD. Preparatory procedures with a balloon were attempted without success, leading to the decision to utilize a Rotablator with a burr size of 1.25. Subsequent ballooning and the placement of an additional stent from the mid to the distal LAD were carried out.


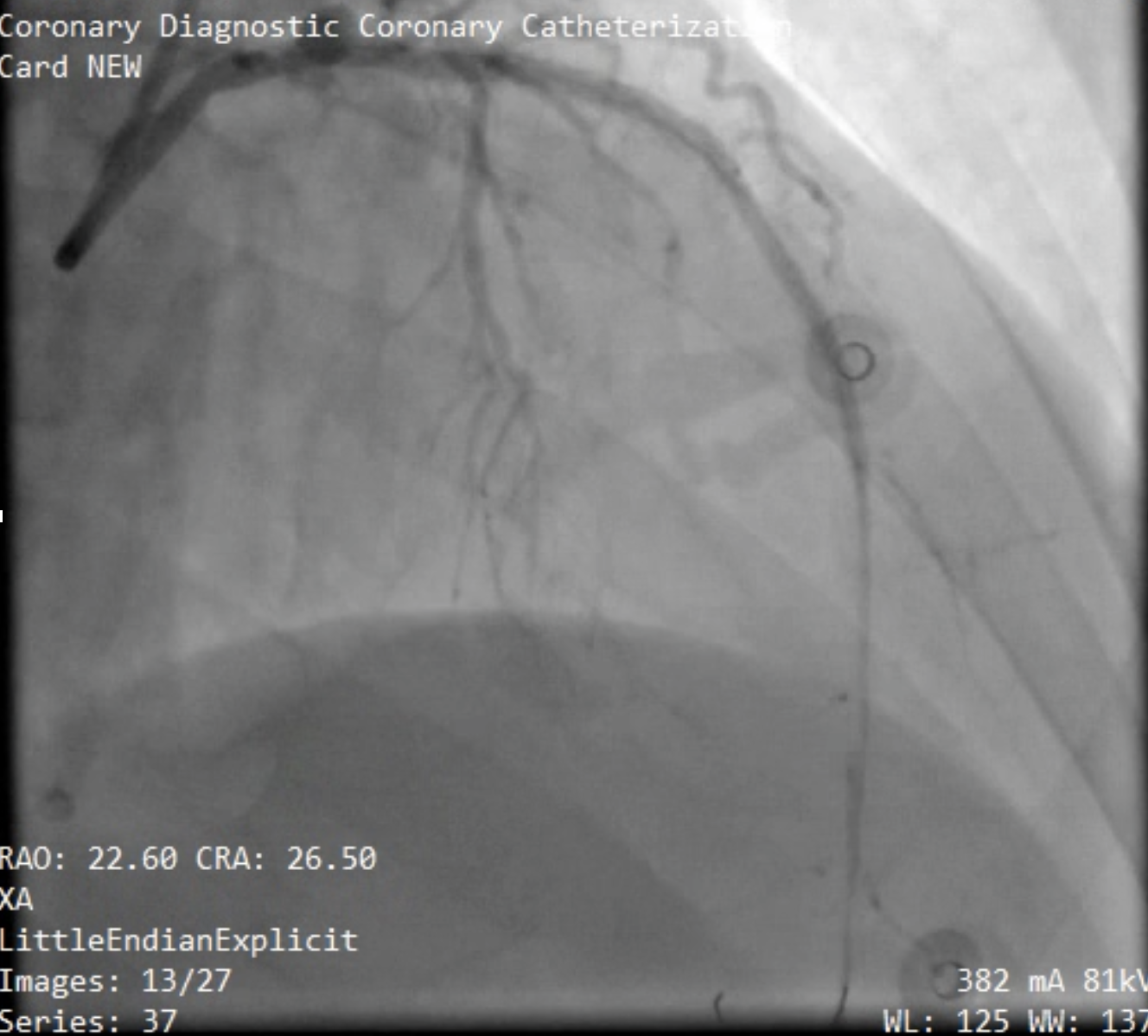
Case Summary
A no-flow condition was identified, extending from the distal left main (LM) to the proximal left anterior descending (LAD) artery. Advancing the wire to the distal LAD presented challenges. However, upon successfully reaching the D1 branch, attempts at balloon angioplasty proved ineffective. Subsequently, a stent was placed from the distal LM to the proximal LAD, restoring blood flow from the LM to the mid LAD. The improvement in blood flow coincided with the alleviation of the patient's symptoms, allowing the operator to further advance the wire to the distal LAD and enhance preparations using rotablation and balloon angioplasty. Stent placement was successful, TIMI III flow to distal LAD.

