Lots of interesting abstracts and cases were submitted for TCTAP 2024. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-038
Overcoming Left Main Bifurcation Lesion With Nodular Calcification Using Rota-Cut Strategy
By Akara Kijnithikul, Sakolwat Montrivade, Sukhum Tachasakunjaroen, Wasant Soonfuang, Anuruck Jeamanukoolkit
Presenter
Akara Kijnithikul
Authors
Akara Kijnithikul1, Sakolwat Montrivade1, Sukhum Tachasakunjaroen1, Wasant Soonfuang1, Anuruck Jeamanukoolkit1
Affiliation
Police General Hospital, Thailand1,
View Study Report
TCTAP C-038
Coronary - Complex PCI - Calcified Lesion
Overcoming Left Main Bifurcation Lesion With Nodular Calcification Using Rota-Cut Strategy
Akara Kijnithikul1, Sakolwat Montrivade1, Sukhum Tachasakunjaroen1, Wasant Soonfuang1, Anuruck Jeamanukoolkit1
Police General Hospital, Thailand1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
A 74-year-old man with history of prior MI, type 2 DM, HTN, DLP, and CKD presented with dyspnea on exertion and orthopnea for 3 days. Previous CAG at the time of MI in 2020 showed severe RCA disease and borderline distal LM lesion with nodular calcification. PCI of RCA was performed and FFR of LM-LAD at that time was negative. Physical examination revealed fine crepitation in both lower lungs and cardiovascular exam showed regular pulse, normal s1s2, no murmur.


Relevant Test Results Prior to Catheterization
EKG revealed sinus rhythm with diffuse ST depressed in V4-6,I,II, and aVL and ST elevated in aVR. Echocardiogram showed concentric LVH with normal LVEF of 53% without regional wall motion abnormalities and no significant valvular heart disease. Laboratory showed hs-Trop T of 2,350 ng/L. The diagnosis was NSTE-ACS with heart failure.
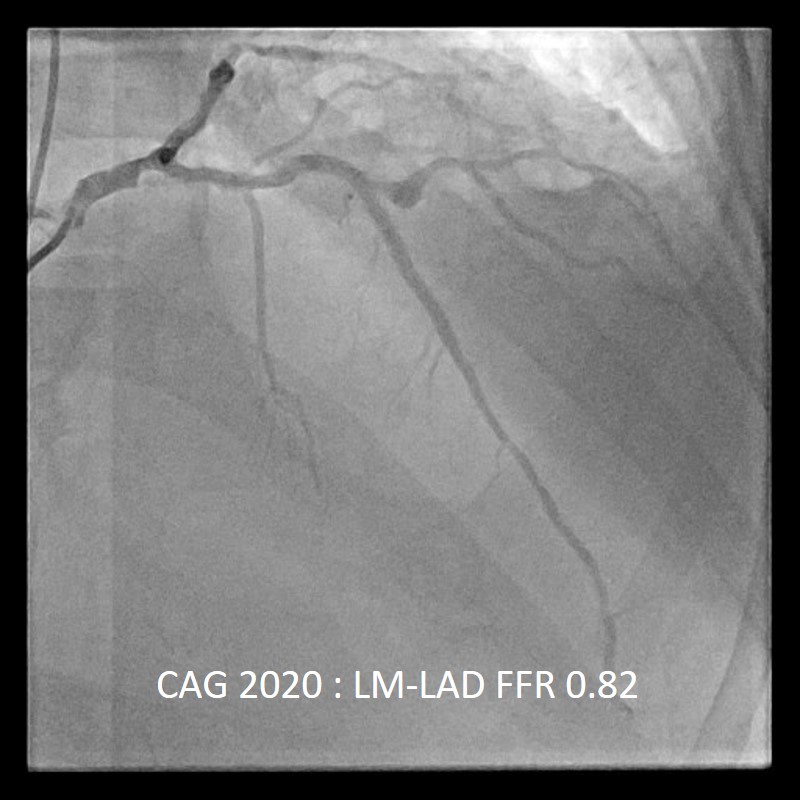


Relevant Catheterization Findings
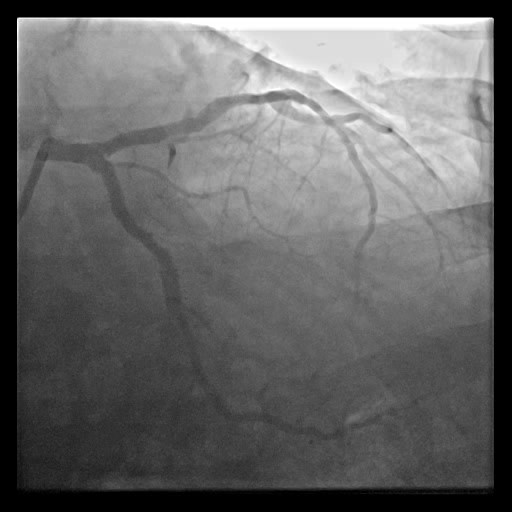
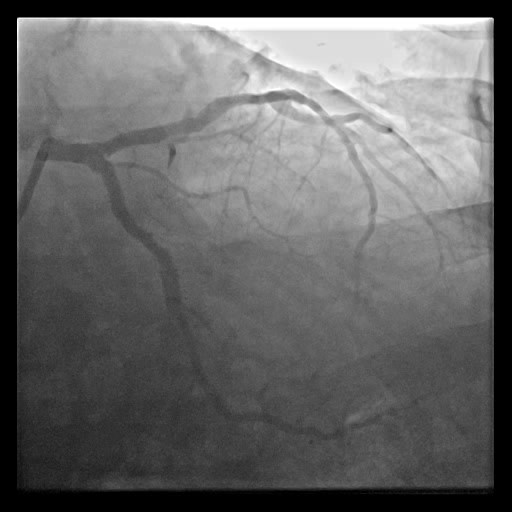
CAG showed three-vessel disease with LM.




Interventional Management
Procedural Step
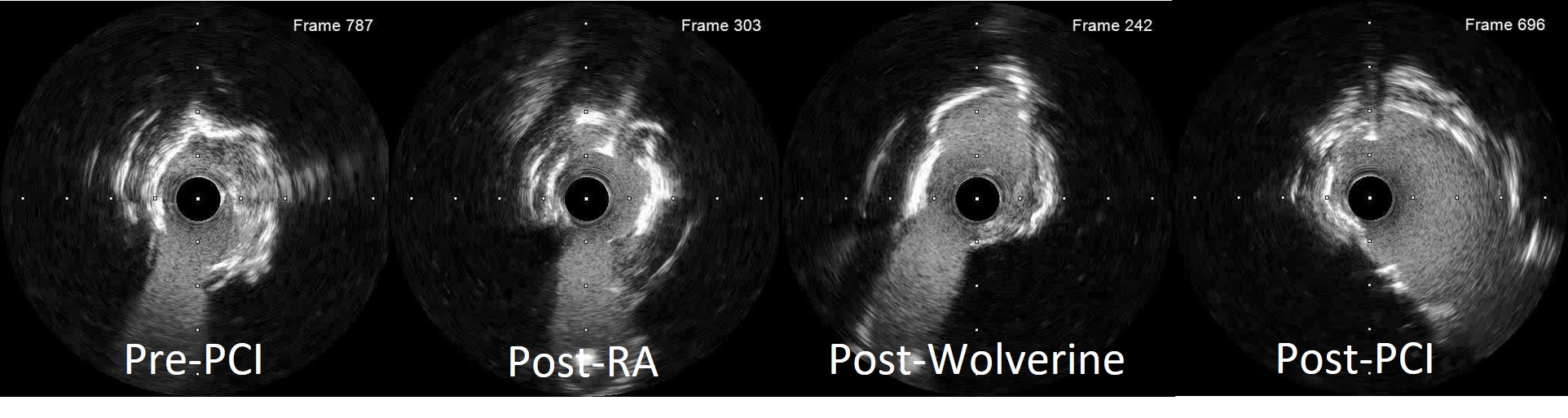
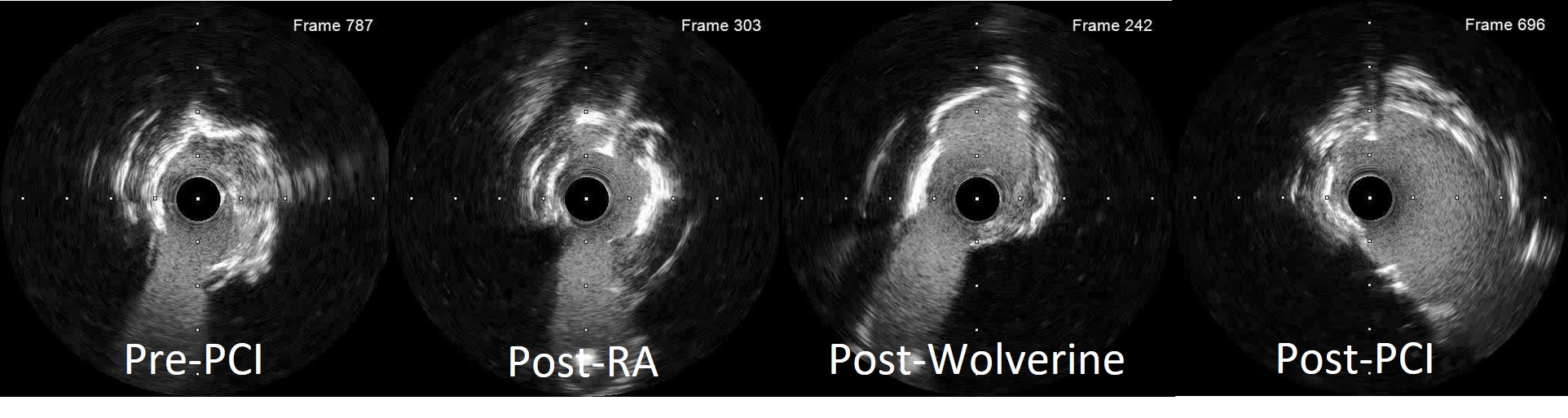
Right radial access was obtained with 7Fr sheath. LCA was engaged with EBU3.5, 7Fr catheter and Runthrough NS guidewire crossed LAD lesion in Finecross microcatheter. The IVUS catheter couldn’t pass through the mid LAD lesion. IVUS showed nodular calcification at distal LM and circumferential calcified plaque at proximal LAD. Given nodular calcification, we opted to perform rotational atherectomy at both LAD and LCx. Wire was exchanged to Rotawire Extra support. Rotational atherectomy was performed using Rota Burr 1.75 mm at 180,000 rpm for 2 rounds at proximal LAD. Proximal LCx was treated with Rota Burr 1.75 mm at 180,000 rpm for 4 rounds. IVUS post rotablation showed thinning of nodular calcification in the figure of 8 pattern but there was no evidence of calcium fracture. We then further treated the lesion with Wolverine cutting balloon 3.25 x 10 mm at both LM- ostial LAD and LM-ostial LCx. Repeated IVUS showed large luminal area with multiple calcium fractures and obliteration of LM nodular calcification.


Case Summary
PCI of the LM lesion with nodular calcification is very challenging as it causes inadequate lesion preparation and a very high risk of stent underexpansion. In our case, optimal calcium modification was obtained using the combination of:- Rotablation of both LAD and LCx using proper Burr size of 1.75 mm.- The use of rotawire extrasupport to achieve optimal wire bias for ablation.- Further treatment of Wolverine cutting balloon to crack the calcium and gain additional luminal area.- IVUS guidance to confirm adequate lesion preparation and the presence of calcium fracture.- Double Kissing Culotte technique as the final stenting strategy.

