Lots of interesting abstracts and cases were submitted for TCTAP 2024. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-151
A Patient With Triple Vessel Disease and Cardiogenic Shock
By Koon Wee Koay, Kuo Ting Lee, Shahul Hamid K A Ahmadsah, Poi Keong Kong, Mohamed Jahangir Abdul Wahab
Presenter
Koon Wee Koay
Authors
Koon Wee Koay1, Kuo Ting Lee2, Shahul Hamid K A Ahmadsah3, Poi Keong Kong1, Mohamed Jahangir Abdul Wahab1
Affiliation
Penang General Hospital, Malaysia1, Sultanah Bahiyah Hospital, Malaysia2, Hospital Pulau Pinang, Malaysia3,
View Study Report
TCTAP C-151
Coronary - High-Risk Intervention (Diabetes, Heart Failure, Renal Failure, Shock, etc)
A Patient With Triple Vessel Disease and Cardiogenic Shock
Koon Wee Koay1, Kuo Ting Lee2, Shahul Hamid K A Ahmadsah3, Poi Keong Kong1, Mohamed Jahangir Abdul Wahab1
Penang General Hospital, Malaysia1, Sultanah Bahiyah Hospital, Malaysia2, Hospital Pulau Pinang, Malaysia3,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
Mr M is a 58 years old gentleman who has underlying diabetes mellitus and chronic smoker. He presented with stable angina for 1 month. Coronary angiogram showed triple vessel disease and he was referred to surgeon for early coronary artery bypass grafting. Unfortunately, he presented with acute coronary syndrome complicated with acute pulmonary oedema before surgery date. Blood pressure was 90/60 mmHg, pulse rate 101 bpm, oxygen saturation 92% on air. He was intubated and started on inotrope.
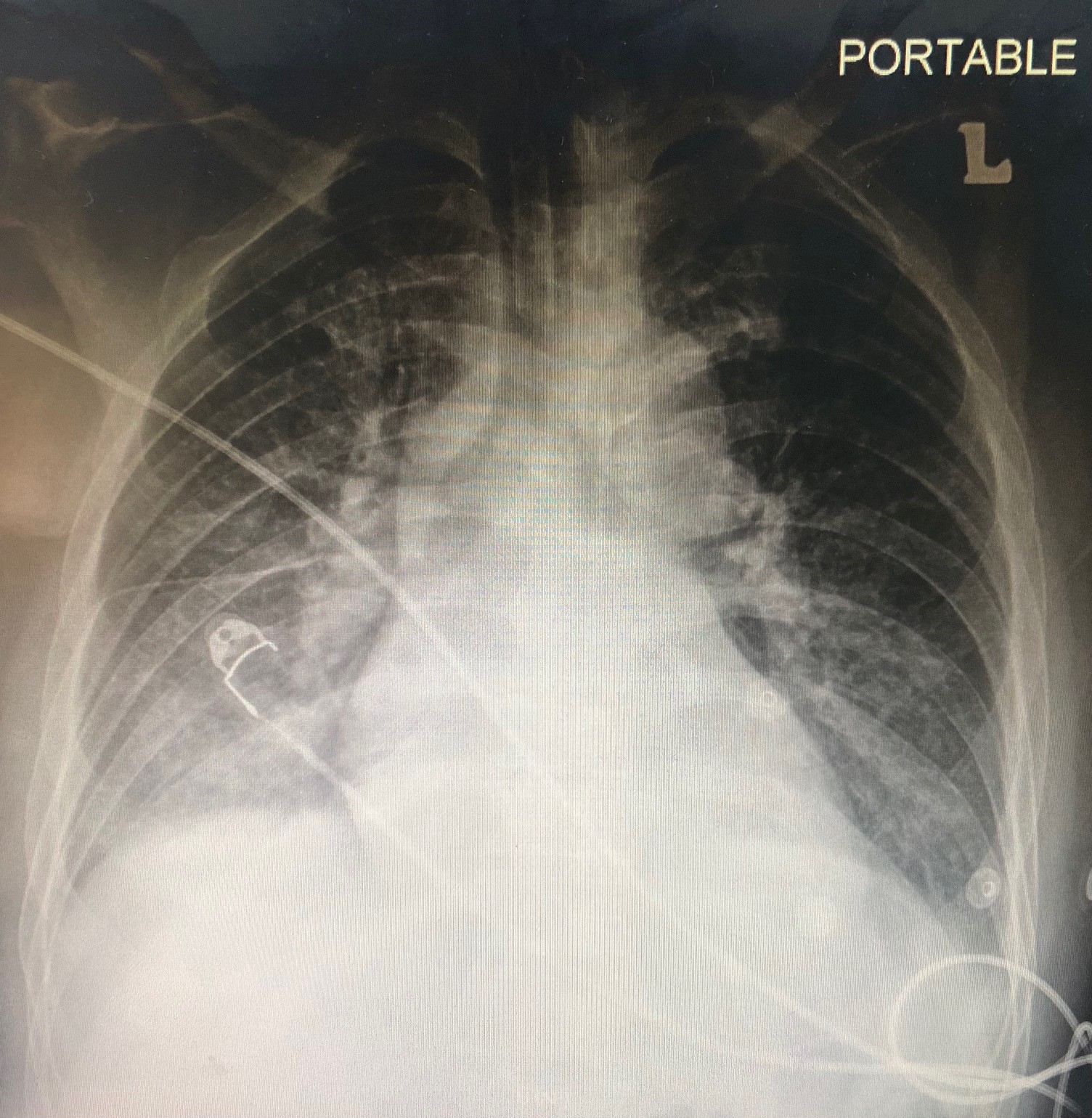
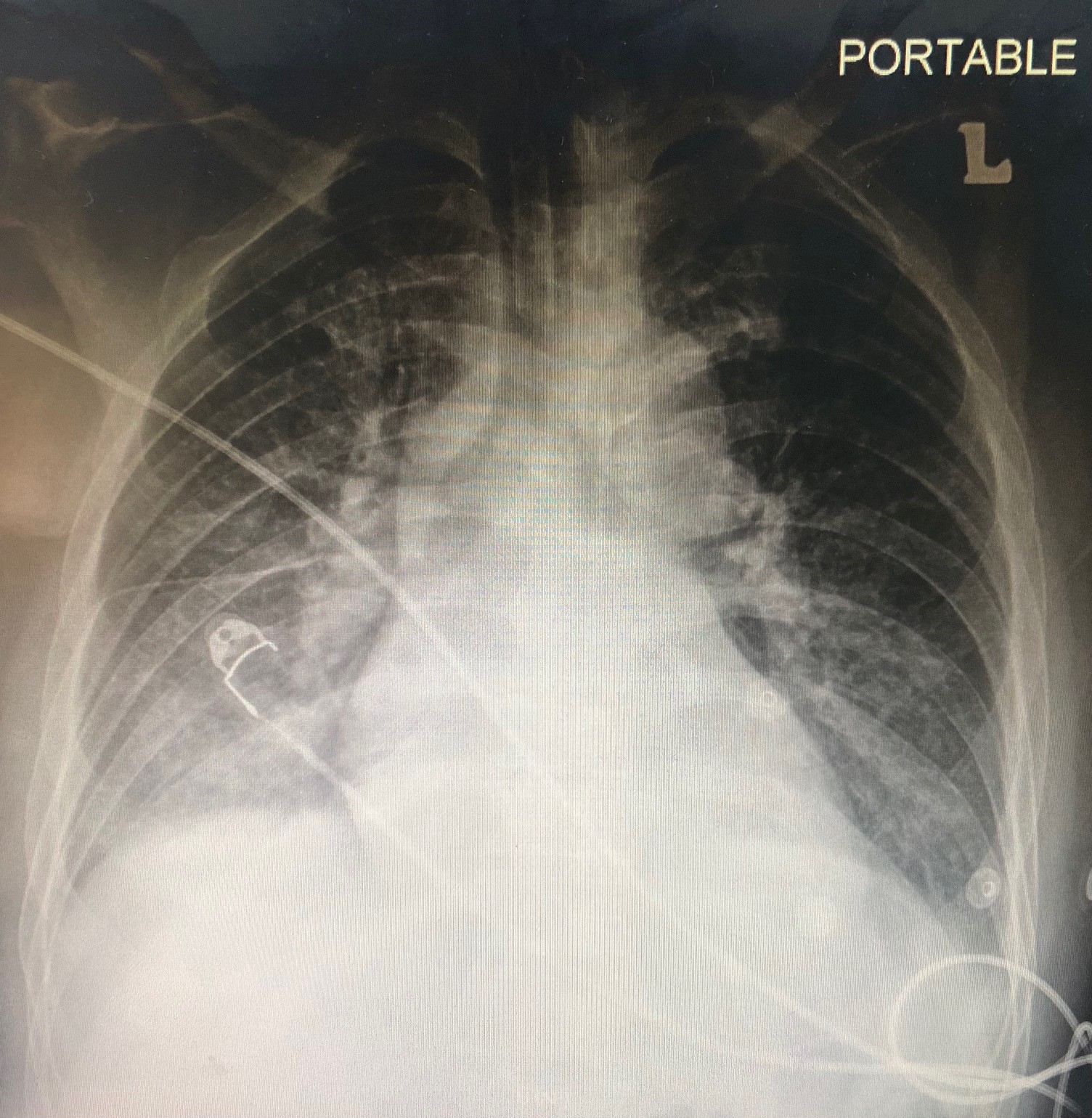
Relevant Test Results Prior to Catheterization
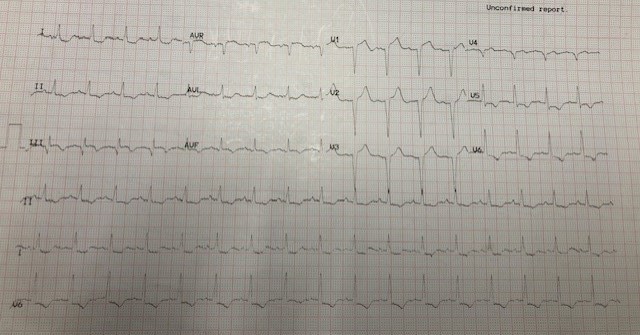
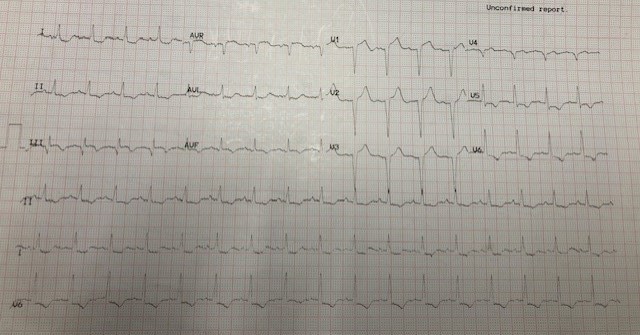
ECG showed sinus rhythm with Q wave at V2 to V4 and ST depression at II, III, aVF and V5 to V6. Echocardiogram showed a left ventricular ejection fraction of 20% and global hypokinesia. His Troponin T was raised at 1054 ng/L.
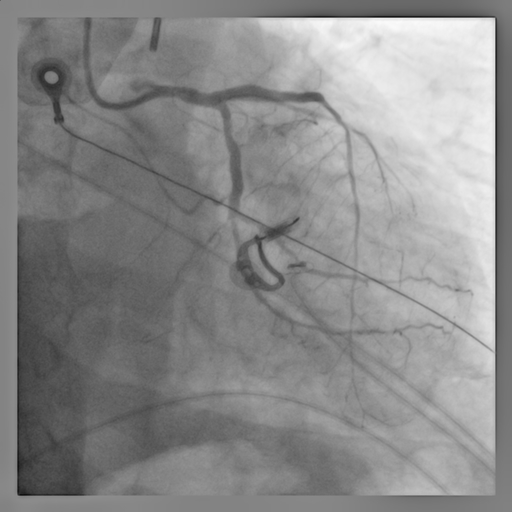
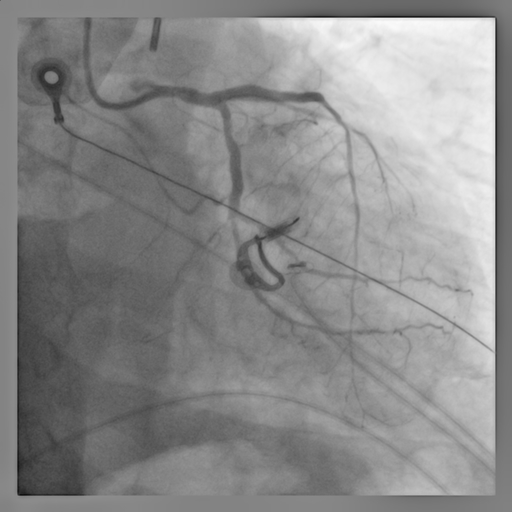
Relevant Catheterization Findings
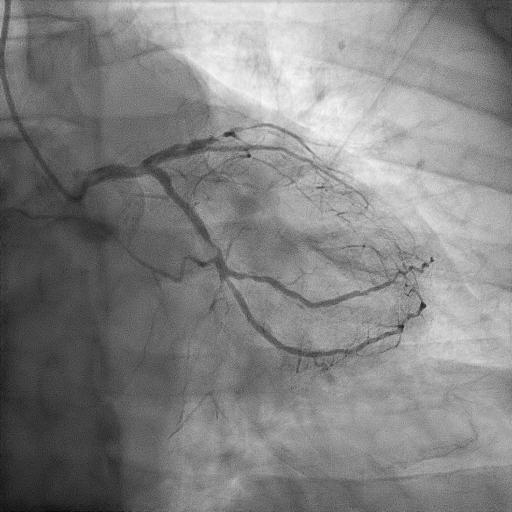
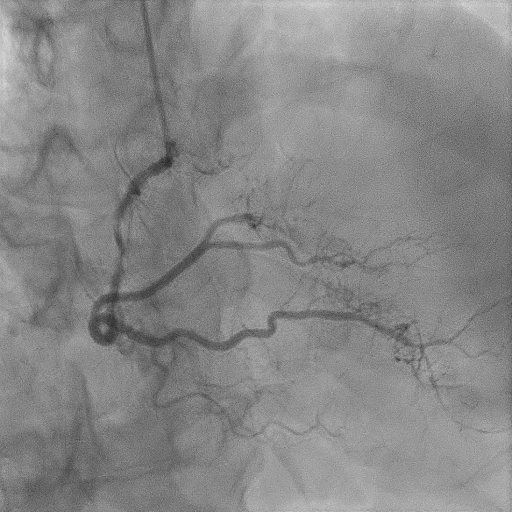
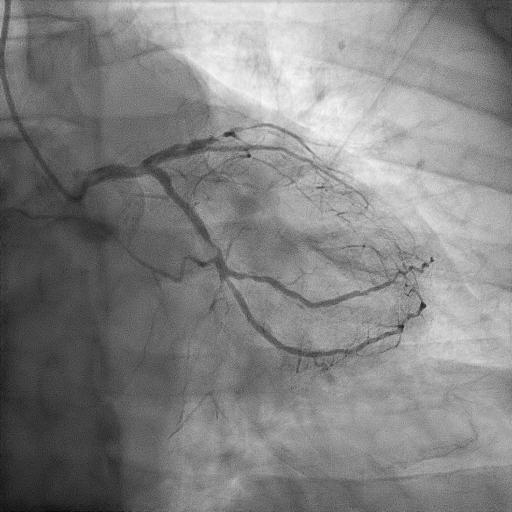
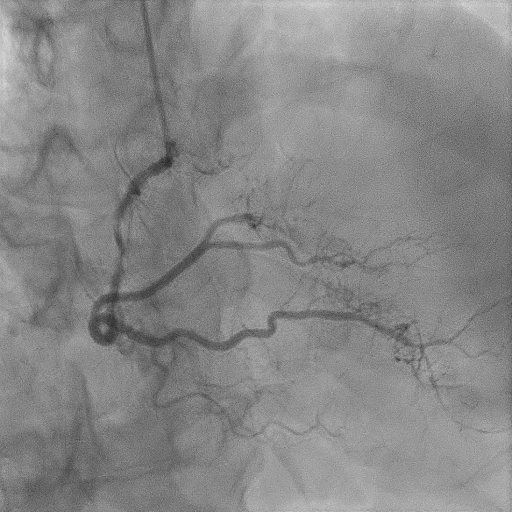
Coronary angiography showed minor disease at distal left main (LM), diffuse disease from ostial left anterior descending (LAD) artery and a critical 99% stenosis at mid-LAD, 90% stenosis at mid segment of left circumflex (LCX) artery and 70% stenosis at mid-right coronary artery (RCA).


Interventional Management
Procedural Step
Heart team discussion was done and he was planned for high risk percutaneous coronary intervention (PCI) under intra-aortic balloon pump (IABP) support. IABP was inserted via left femoral artery upfront and started at full augmentation. Right radial puncture was done with 6Fr radial sheath. The mid-LAD subtotal occlusion was crossed with Fielder FC wire and predilated with SC 2.0 mm balloon and SC 2.5 mm balloon. LCX was wired with Runthrough Floppy wire and mid-LCX was predilated with SC 2.5 mm balloon and was stented with Resolute Onyx 3.0 x 18 mm stent. We opted for provisional stenting at the distal LM bifurcation lesion. Mid-LAD was stented with Resolute Onyx 3.0 x 26 mm stent and another Resolute Onyx 3.5 x 26 mm was stented from body of LM till proximal LAD, overlapped with the mid-LAD stent. The mid till proximal LAD stent was postdilated with NC 3.0 mm and NC 3.5 mm balloon respectively. Proximal optimisation technique (POT) was done to LM with NC 4.0 mm balloon. The LCX was then re-wired at distal stent strut and ostial LCX was dilated with NC 3.0 mm balloon. Final kissing balloon inflation was done to both ostial LAD and ostial LCX with NC 3.5 mm and NC 3.0 mm balloon at 10 atm with simultaneous balloon deflation. Final POT was done to LM with NC 4.0 mm balloon. TIMI 3 flow was achieved at both LAD and LCX. IABP was weaned off on day 2 and he was extubated after 1 week. PCI to RCA was done successfully after 2 weeks from the index procedure.




Case Summary
This case demonstrated the use of IABP as the mechanical circulatory support system during emergency PCI for a patient with cardiogenic shock. Even though IABP-SHOCK II trial concluded that IABP did not significantly reduce the mortality rate for patient with cardiogenic shock, it is still beneficial in certain cases especially when percutaneous left ventricular assist devices are not available. Early revascularization to culprit vessel is crucial and certainly improved the prognosis of this patient. Provisional stenting of the distal left main lesion also simplify the procedure and shortened the procedure time during this emergency setting.

