Lots of interesting abstracts and cases were submitted for TCTAP 2024. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-001
A Challenging Case Report: Non-ST Elevation Acute Coronary Syndrome With Critical Stenosis of Distal Left Main Bifurcation Caused by Eruptive Calcified Nodules
By Piyoros Lertsanguansinchai, Anuruck Jeamanukoolkit, Piyanart Preeyanont, Tanyarat Aramsareewong, Worawut Tassanawiwat
Presenter
Piyoros Lertsanguansinchai
Authors
Piyoros Lertsanguansinchai1, Anuruck Jeamanukoolkit2, Piyanart Preeyanont3, Tanyarat Aramsareewong4, Worawut Tassanawiwat5
Affiliation
King Chulalongkorn Memorial Hospital, Thailand1, Chulabhorn Hospital, Thailand2, Cardiac Center, Thailand3, Phramongkutklao Hospital, Thailand4, Sunpasitthiprasong, Thailand5,
View Study Report
TCTAP C-001
Coronary - ACS/AMI
A Challenging Case Report: Non-ST Elevation Acute Coronary Syndrome With Critical Stenosis of Distal Left Main Bifurcation Caused by Eruptive Calcified Nodules
Piyoros Lertsanguansinchai1, Anuruck Jeamanukoolkit2, Piyanart Preeyanont3, Tanyarat Aramsareewong4, Worawut Tassanawiwat5
King Chulalongkorn Memorial Hospital, Thailand1, Chulabhorn Hospital, Thailand2, Cardiac Center, Thailand3, Phramongkutklao Hospital, Thailand4, Sunpasitthiprasong, Thailand5,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
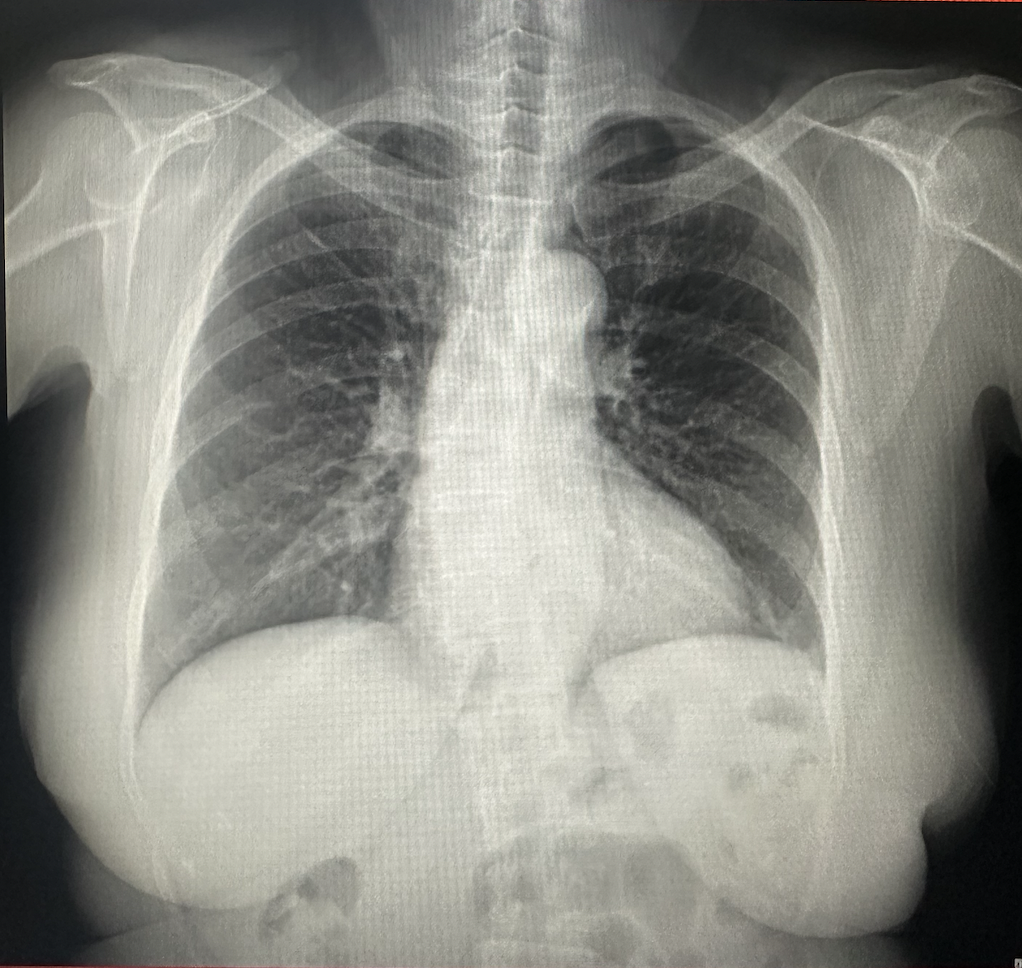
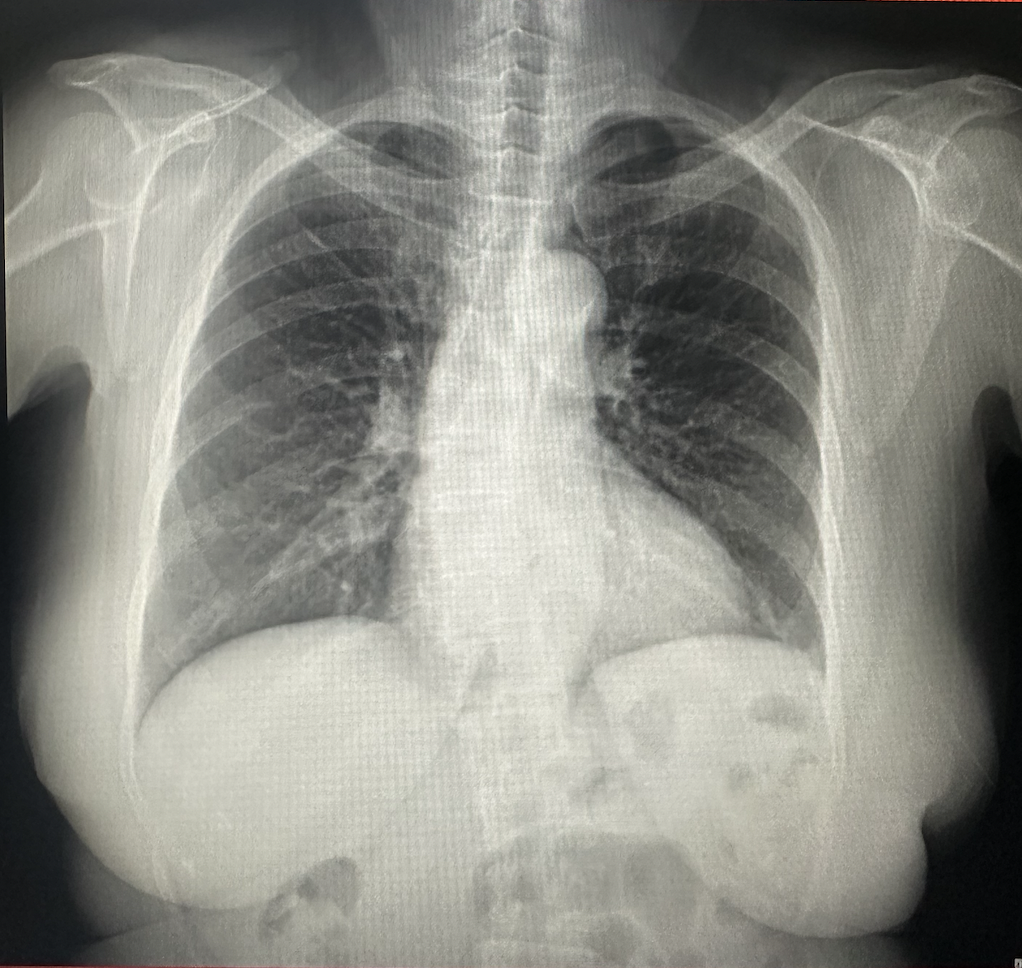
A 70-year-old female with a history of hypertension and dyslipidemia was admitted with non-ST elevation acute coronary syndrome (NSTE-ACS) to the provincial hospital. Her blood pressure was 135/85 mmHg, her heart rate was 70 beats per minute, her respiration rate was 22 breaths per minute, and her temperature was 36.5 oC. The angiography at the provincial hospital showed TVD with LM. The patient was advised to undergo CABG, but she strongly refused. She was referred for PCI at our institution.






Relevant Test Results Prior to Catheterization
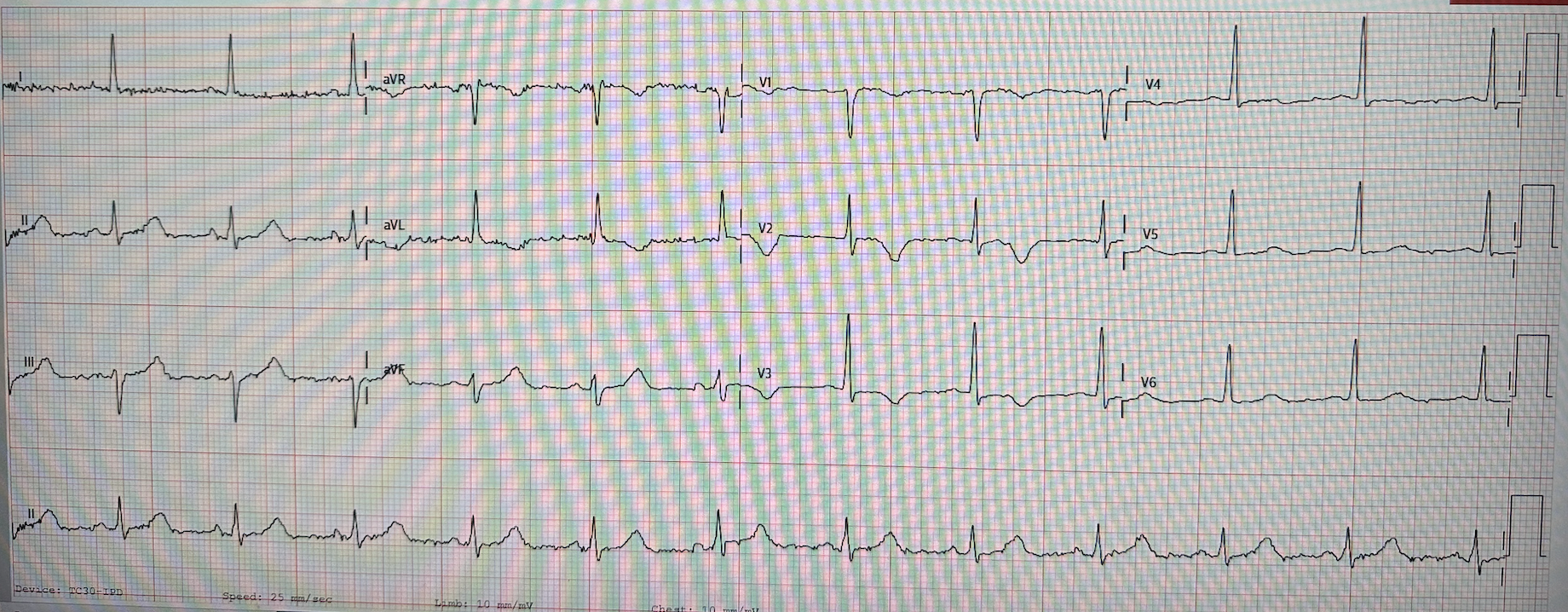
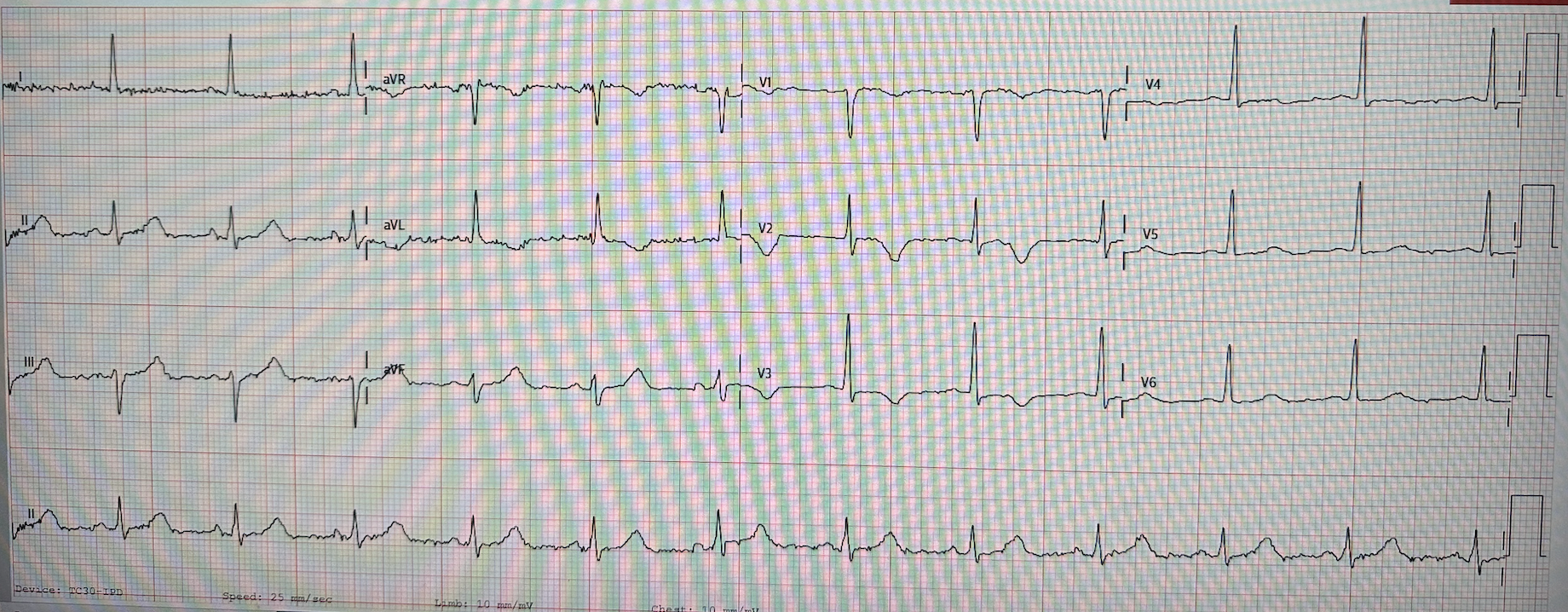
The initial electrocardiogram showed a sinus rhythm rate of 70 bpm with symmetrical T wave inversion in V1 to V3, suggestive of NSTE-ACS. The transthoracic echocardiography revealed a left ventricular ejection fraction (LVEF) of 45% with anterior and anteroseptal wall hypokinesia from mid to apex and no significant valvular abnormalities. The high-sensitivity troponin T at the emergency department was elevated at 1,750 ng/mL (normal range:<13.9 ng/mL). Other laboratory results were normal.
Relevant Catheterization Findings
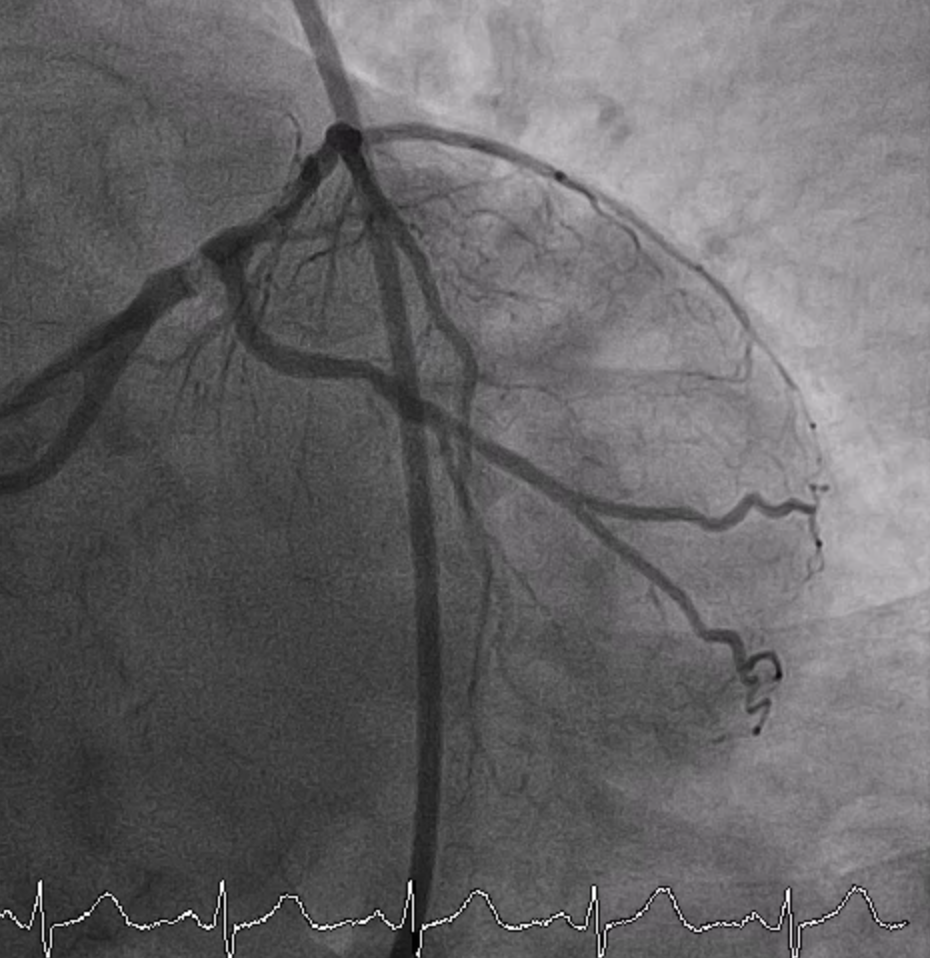
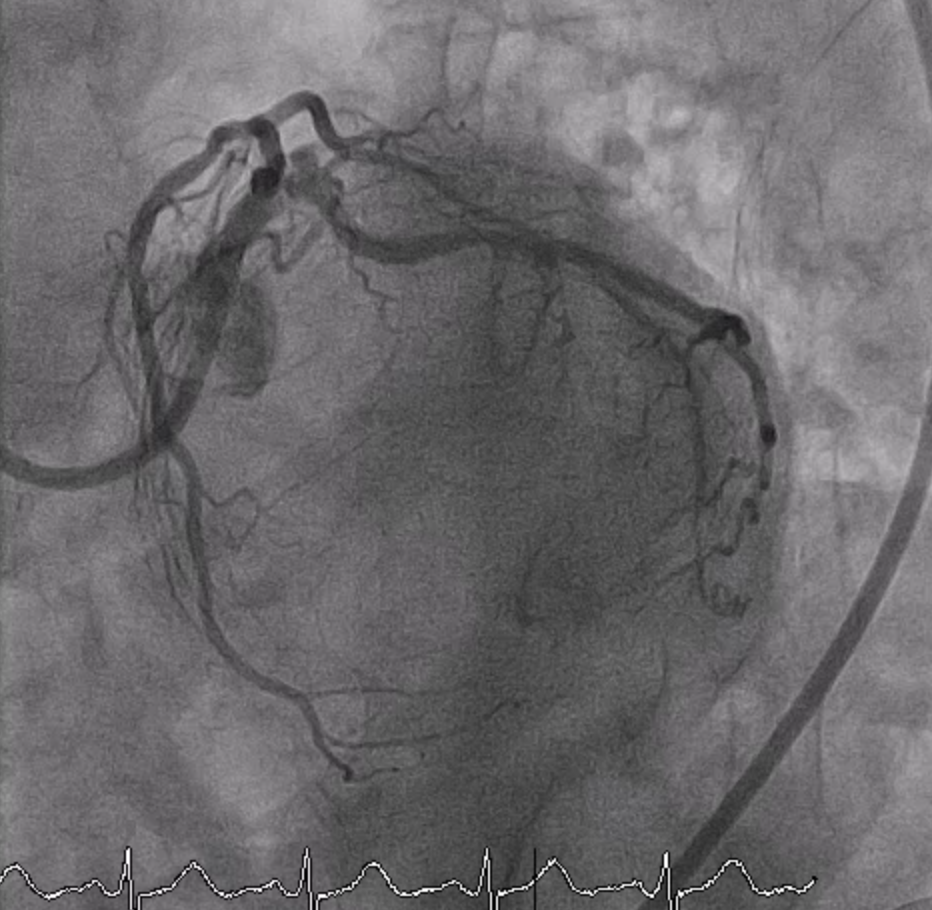
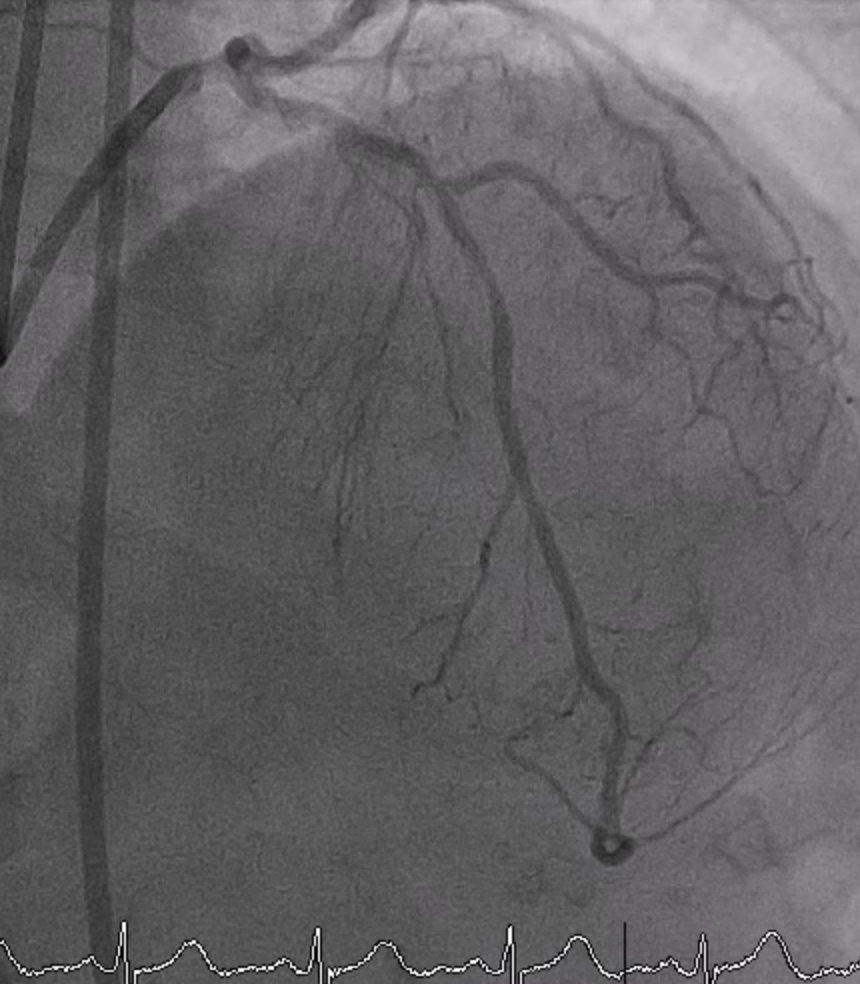
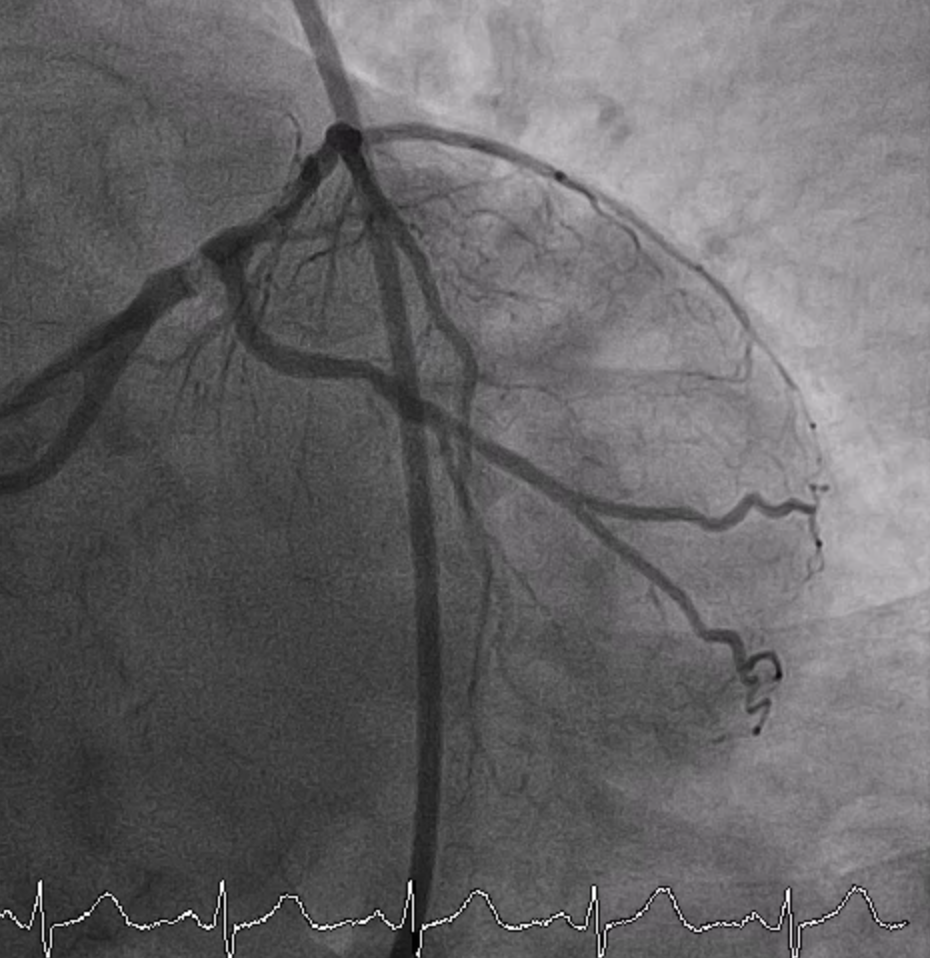
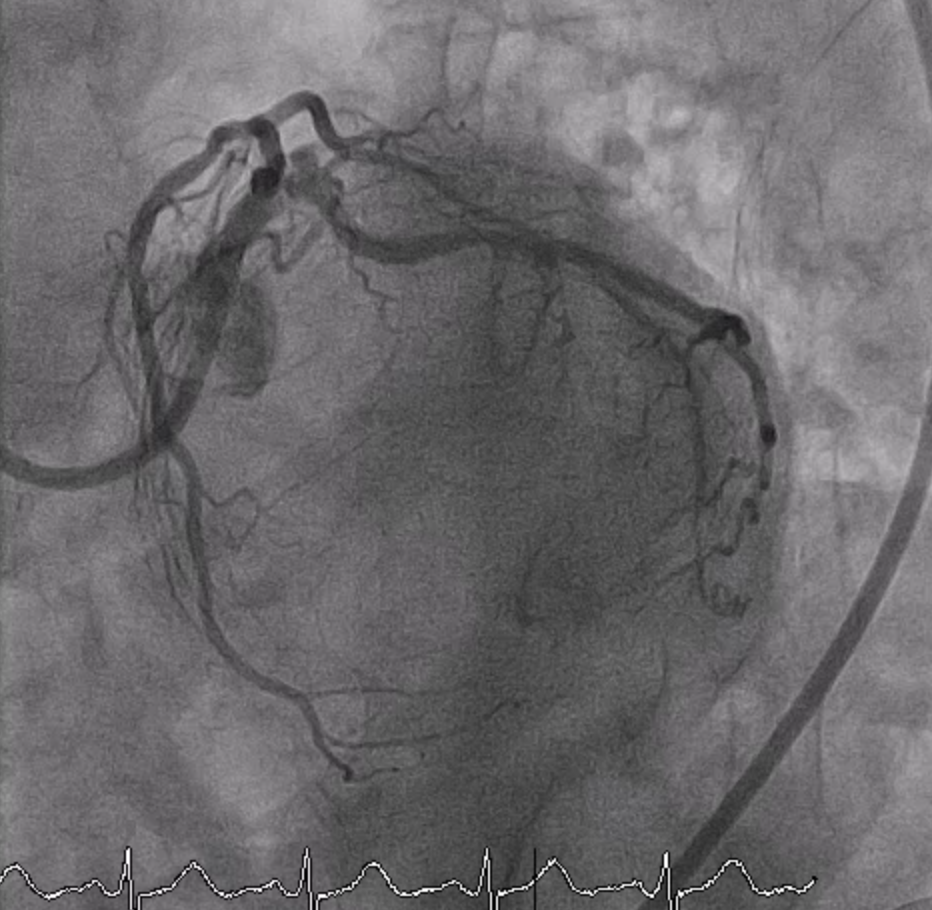
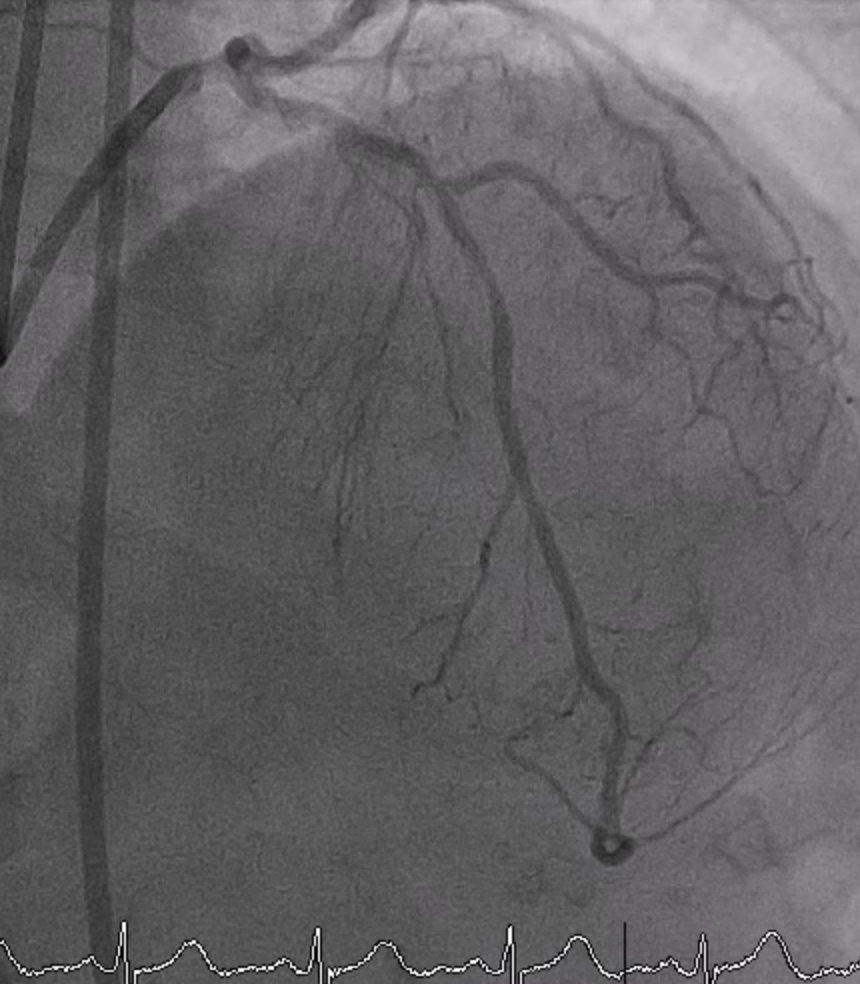
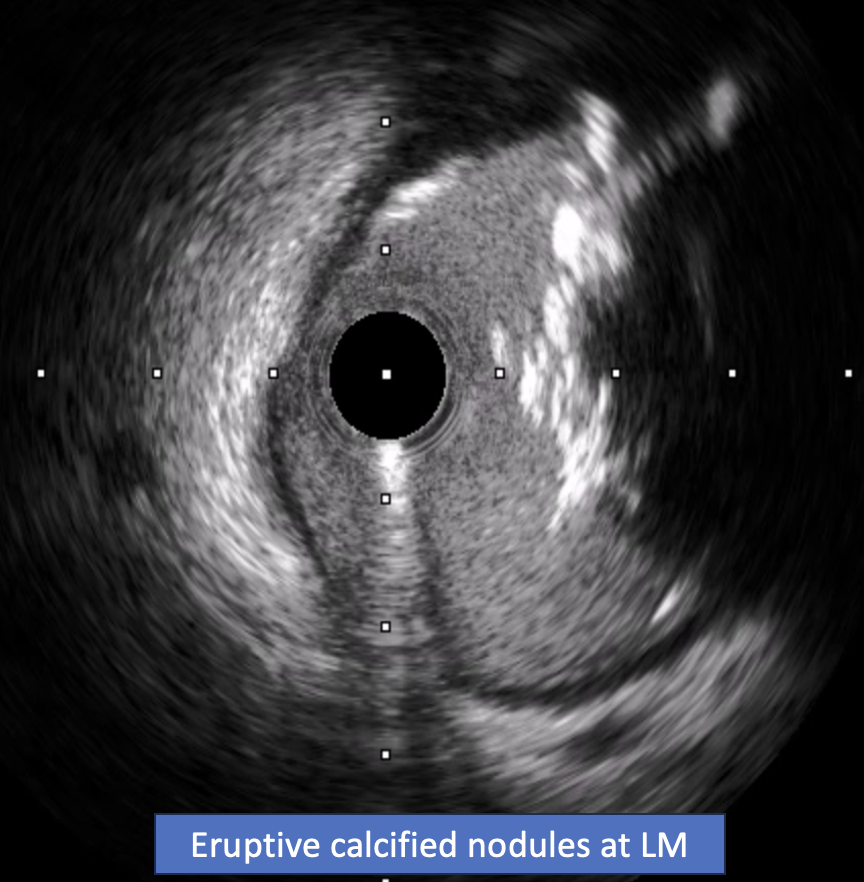
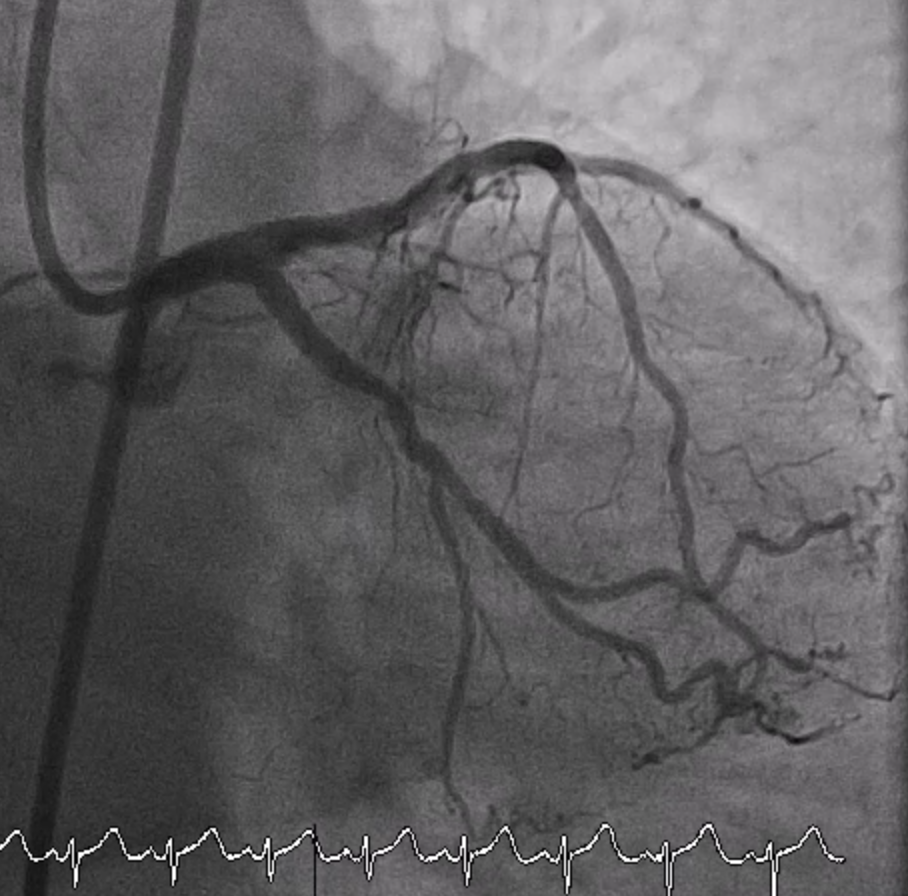
Urgent coronary angiography at the provincial hospital revealed critical stenosis of the distal LM, which is suspicious of a calcified nodule, significant stenosis at the proximal to midLAD, 50% stenosis at the mid LCx, and borderline stenosis at the proximal to mid RCA. Multiple angiogram views were injected to determine the severity of stenosis at the ostial LCx. However, the severity of stenosis at the ostial LCx could not be determined by the multiple angiogram views.
Interventional Management
Procedural Step

Case Summary
This is a case of ACS caused by the eruptive calcified nodules at LM. CABG is the treatment of choice for revascularization in this patient; however, she denied CABG. The DK culotte technique with IVUS guidance for LM bifurcation PCI was successfully performed.In high-risk complex cases, IVUS is useful in the definitive diagnosis of ambiguous lesions, determining the most suitable technique for plaque modification prior to stenting, and determining the optimal strategy for LM bifurcation angioplasty. Some of the eruptive calcified nodules can be deformed by a balloon-based strategy. However, the incidence rate of target lesion failure is higher than that of non-eruptive calcified nodules.

