Lots of interesting abstracts and cases were submitted for TCTAP 2024. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-061
Application of Intracoronary Rendezvous Technique as a Tunnel for Chronic Total Occlusion
By En-Shao Liu, Feng Yu Kuo
Presenter
En-Shao Liu
Authors
En-Shao Liu1, Feng Yu Kuo1
Affiliation
Kaohsiung Veterans General Hospital, Taiwan1,
View Study Report
TCTAP C-061
Coronary - Complex PCI - CTO
Application of Intracoronary Rendezvous Technique as a Tunnel for Chronic Total Occlusion
En-Shao Liu1, Feng Yu Kuo1
Kaohsiung Veterans General Hospital, Taiwan1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
A 56-year-old man with dyslipidemia presented with intermittent chest tightness for months. He was an ex-smoker of 1 pack/day for 15 years and has quitted for 25 years. The LDL level was poorly controlled with 170 mg/dL. No cardiovascular diseases were running in his family. The chest tightness was described as a constriction sensation, especially attacked during exertion. He reported no other discomforts, such as shortness of breath, cold sweating, or radiating pain.
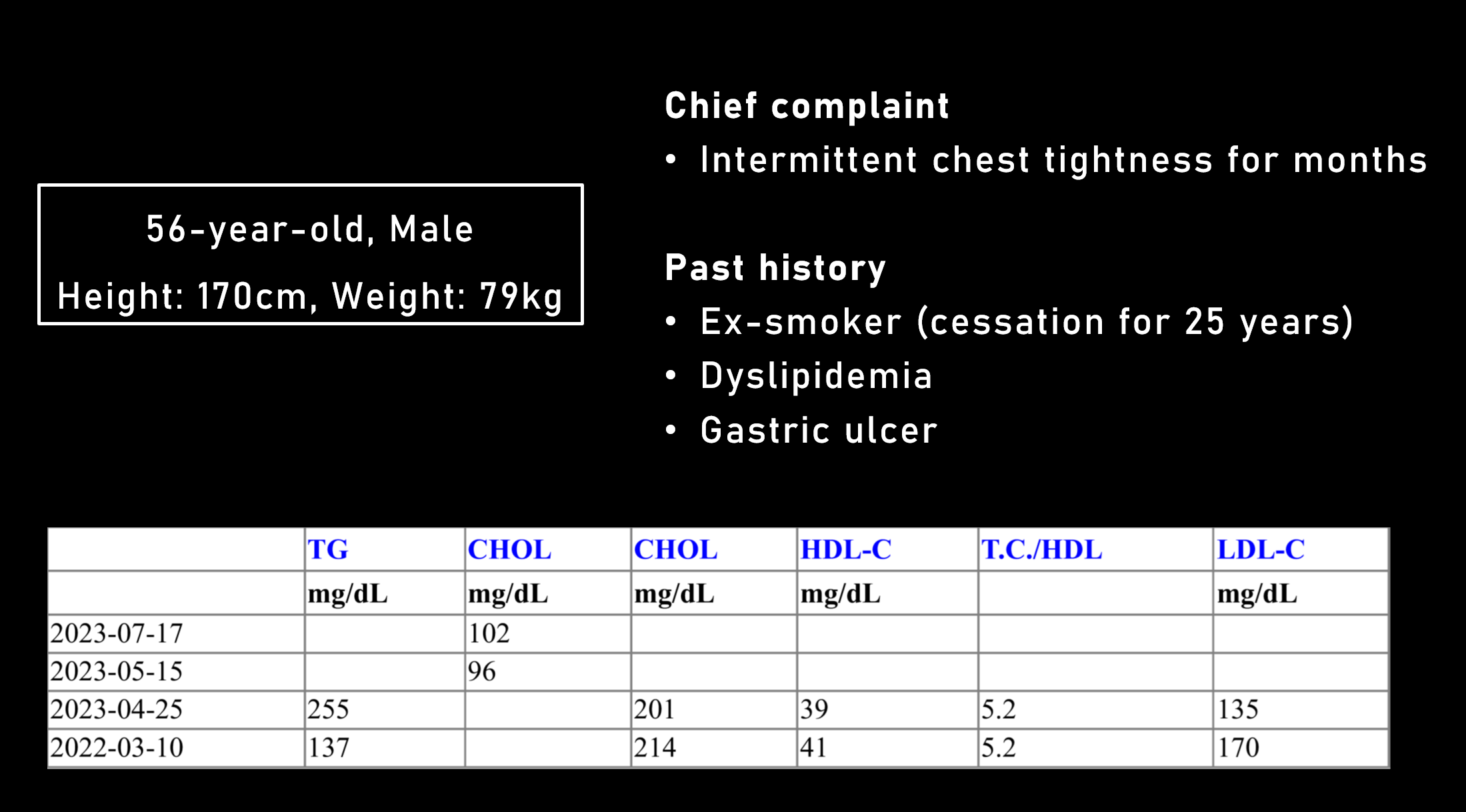
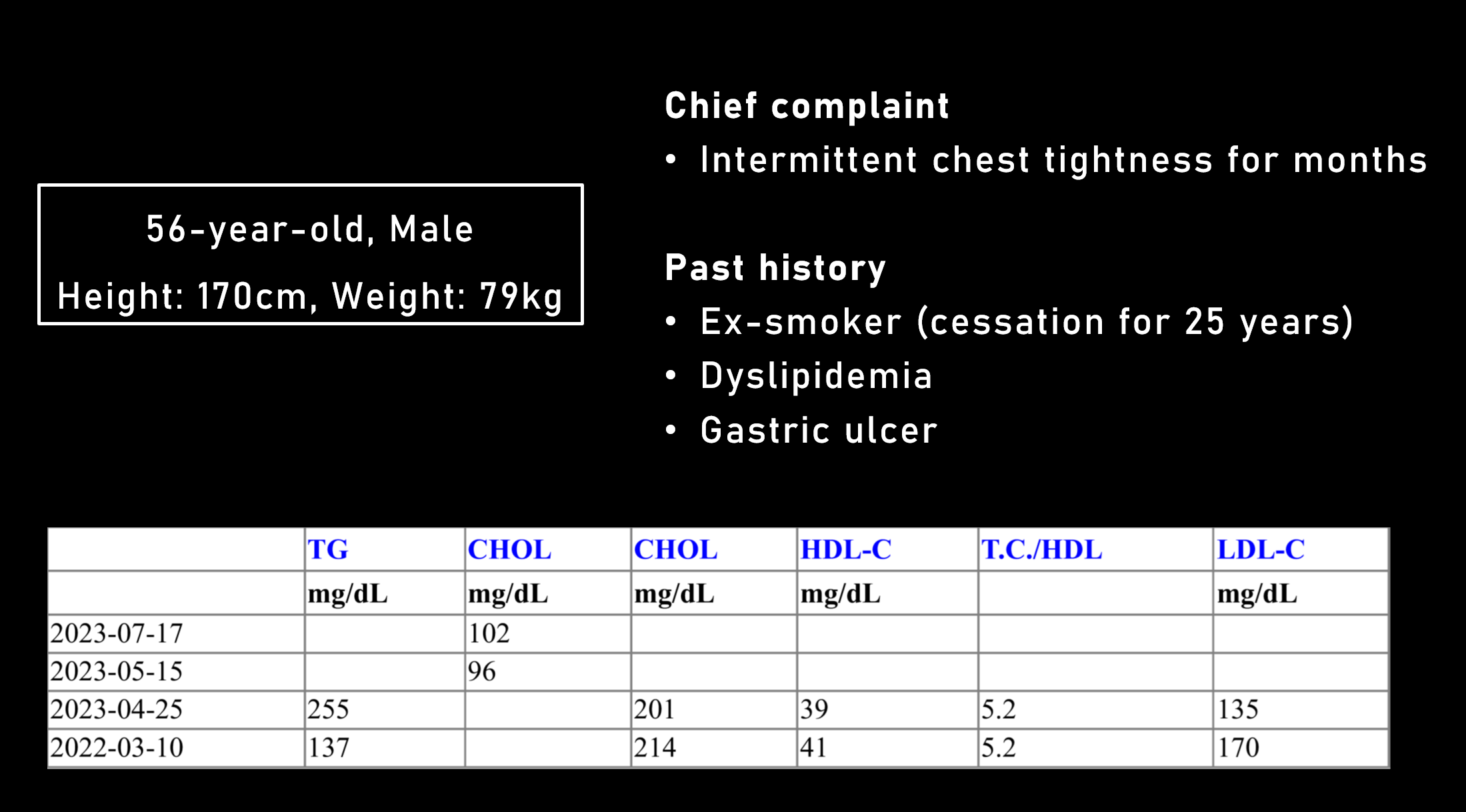
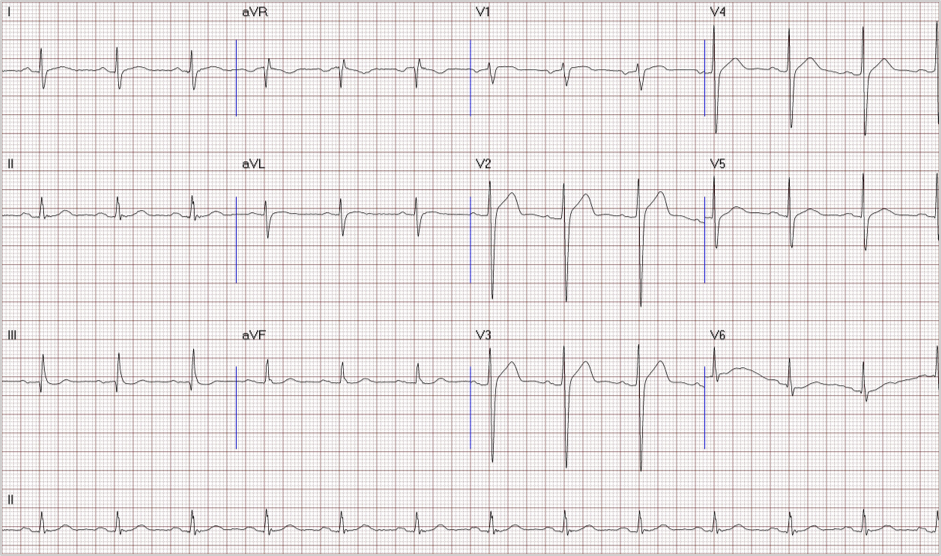
Relevant Test Results Prior to Catheterization
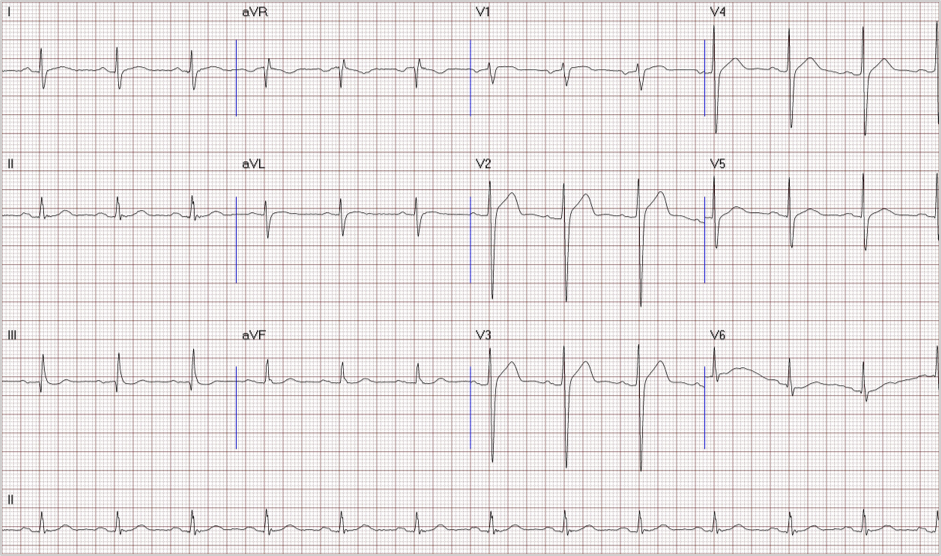
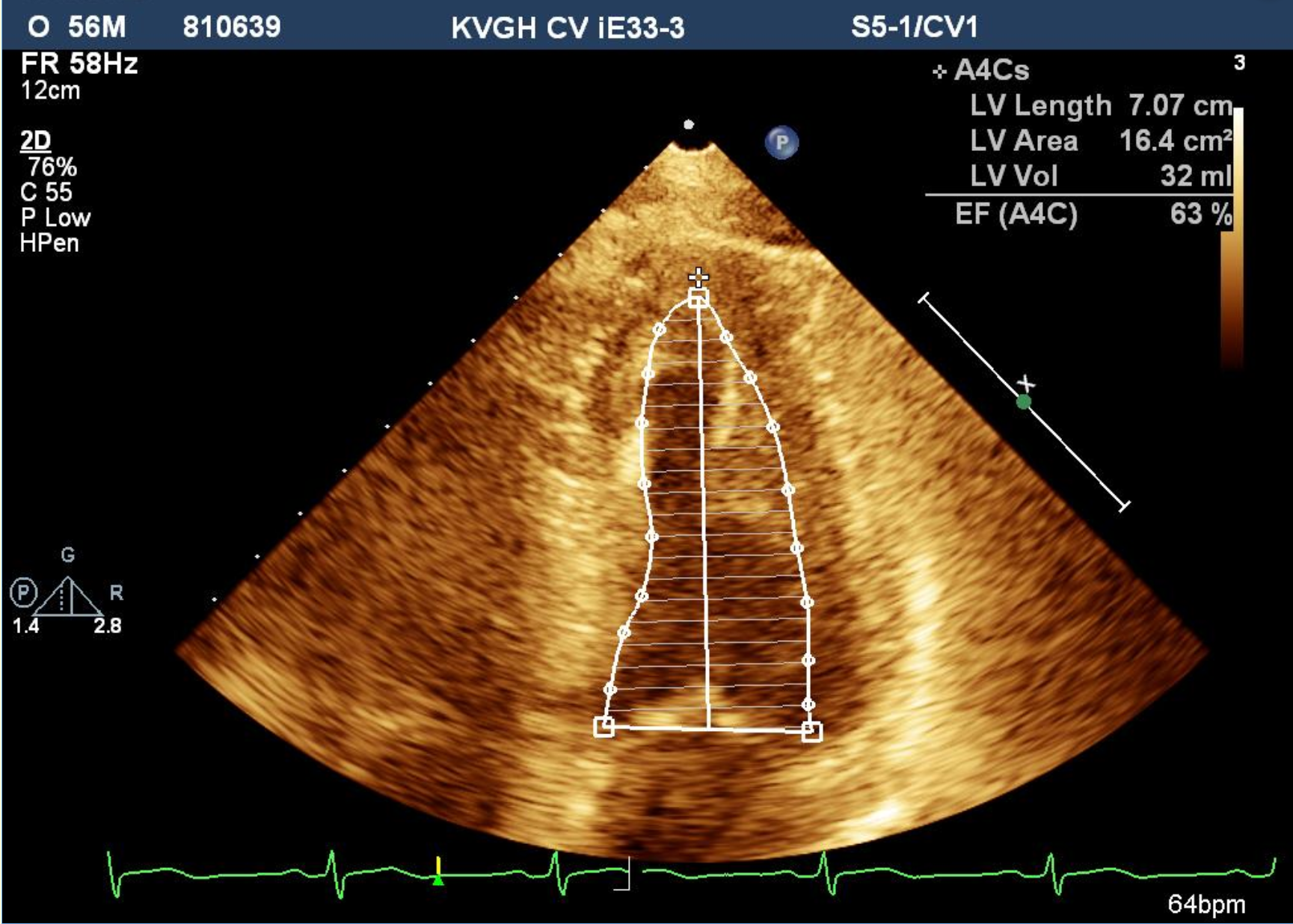
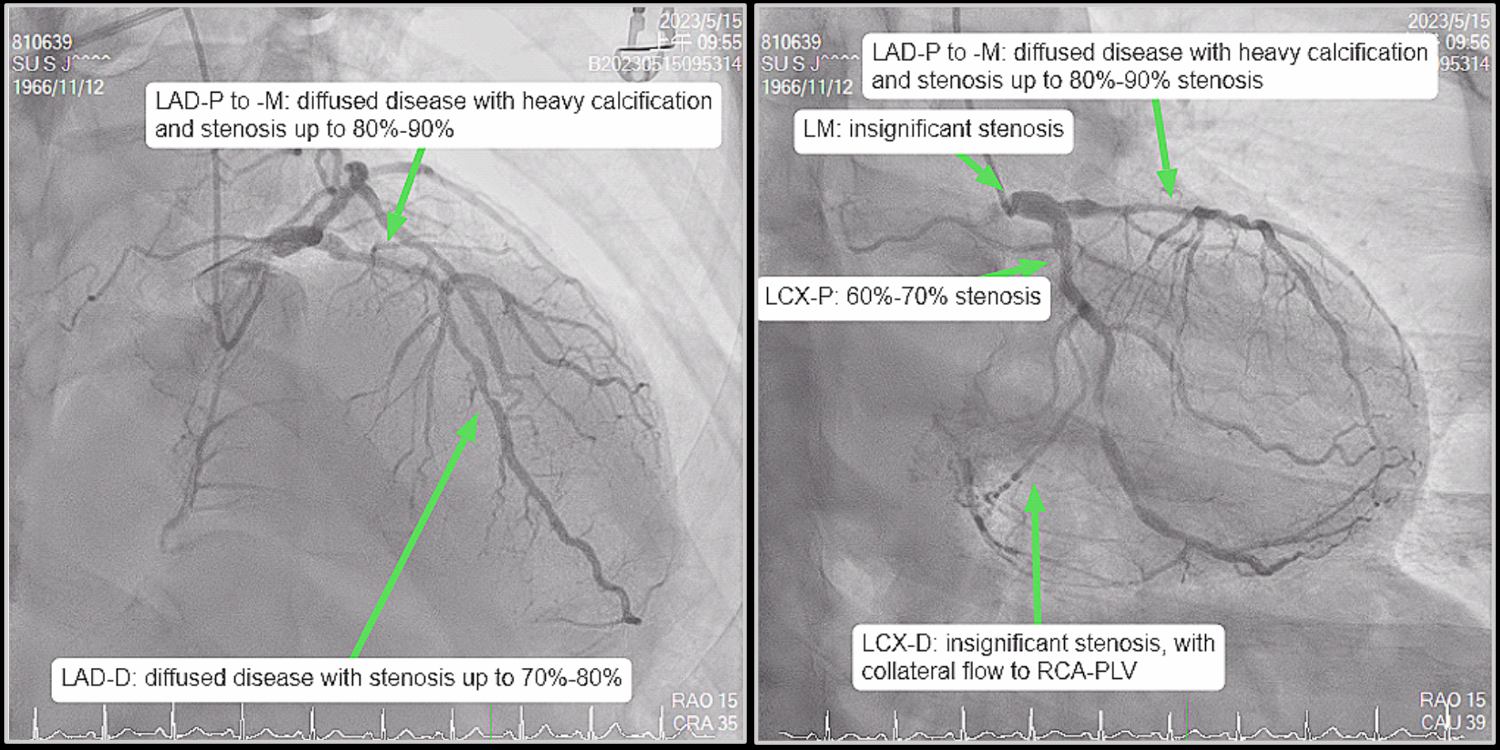
Electrocardiography and echocardiography revealed no significant abnormalities. Coronary computed tomography (CT) angiography disclosed severe stenoses of triple vessels, and Agatston's score progressed to 1079 compared with 625 on a low-dose lung CT scan five years ago. A total occlusion over RCA proximal to the middle segment was noted, and both LAD and LCx had stenoses over 70%.
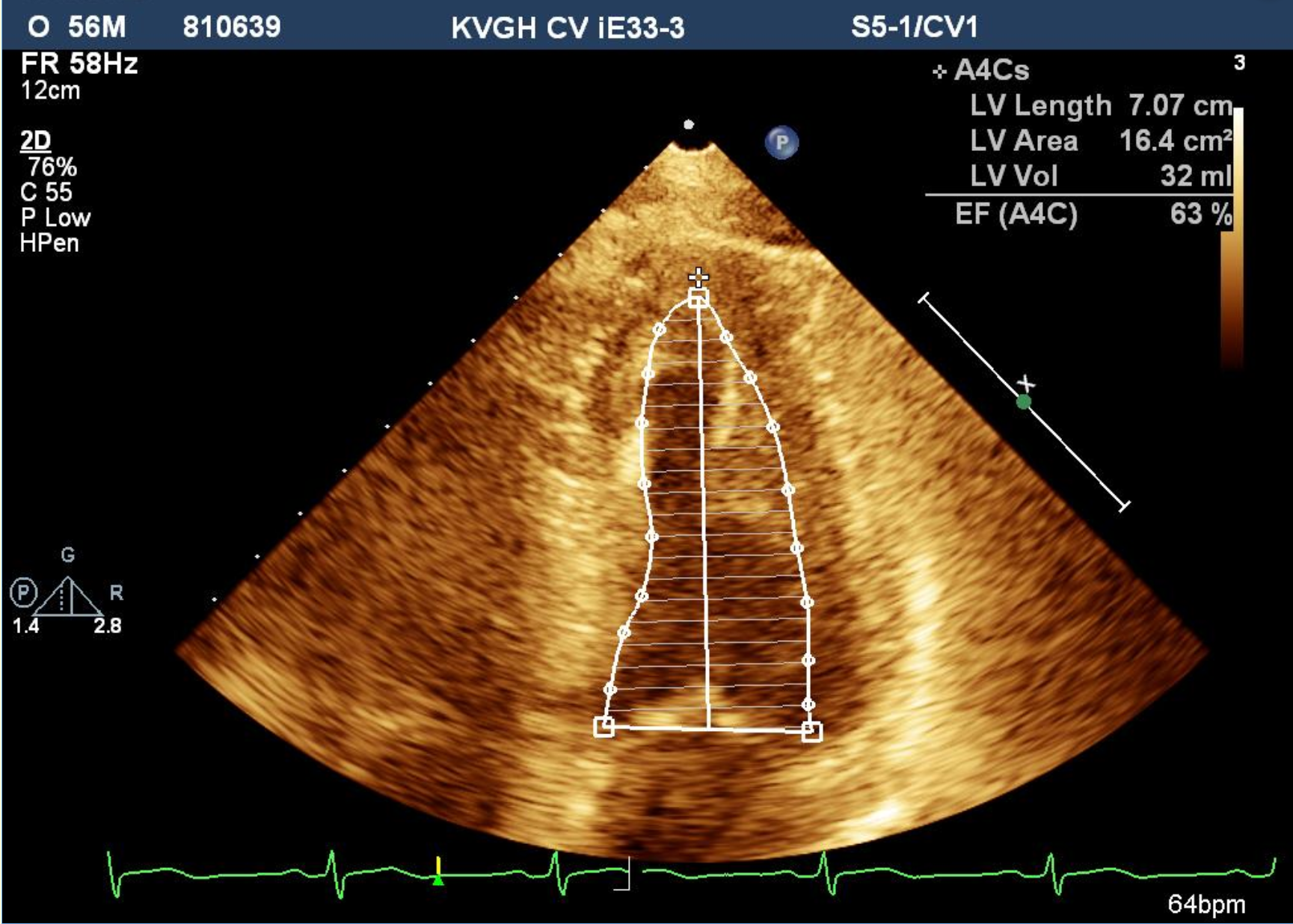
Relevant Catheterization Findings
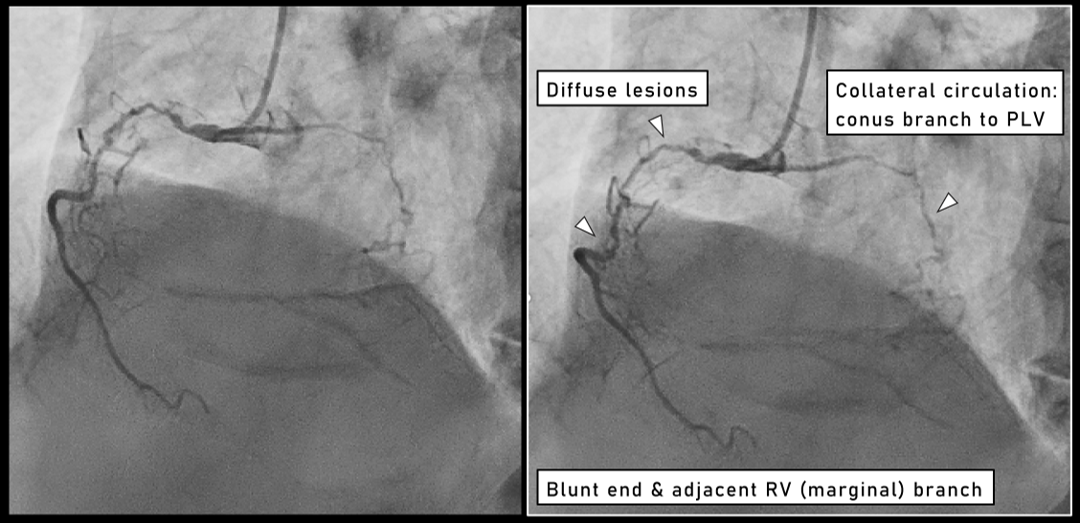
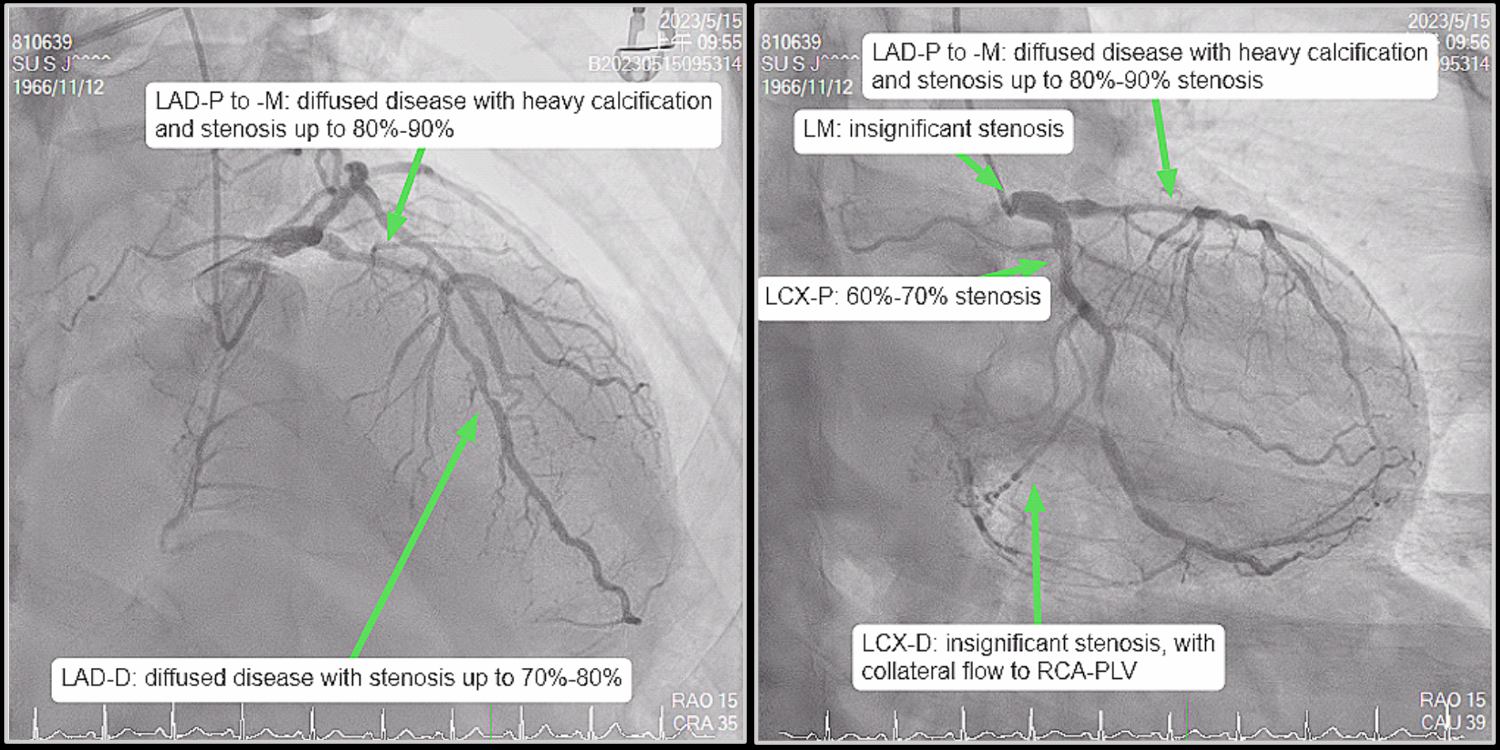
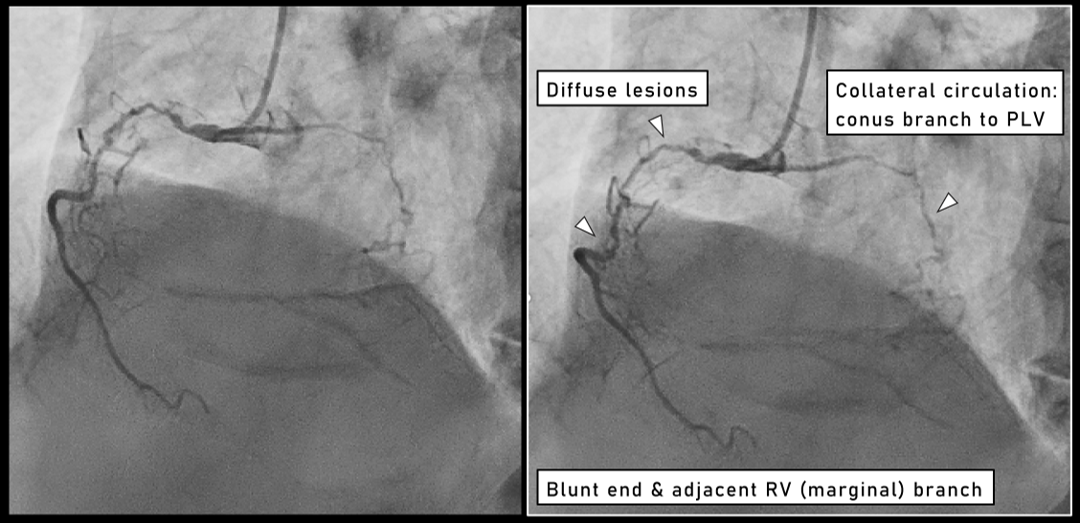
A chronic total occlusion (CTO) lesion was noted in RCA-M, with diffuse stenoses in the proximal part. The RCA-CTO lesion was characterized as a blunt end, with an RV branch by side. The occlusion length was over 20 mm, and the bending angulation was 45 degrees in the route, suggesting a J-CTO score of 3. The conus branch provided a self-collateral flow to RCA-PLV. LAD-P to -D had diffuse lesions without septal collateral flows. LCx had a focal lesion and supplied collateral flows to RCA-PLV.


Interventional Management
Procedural Step
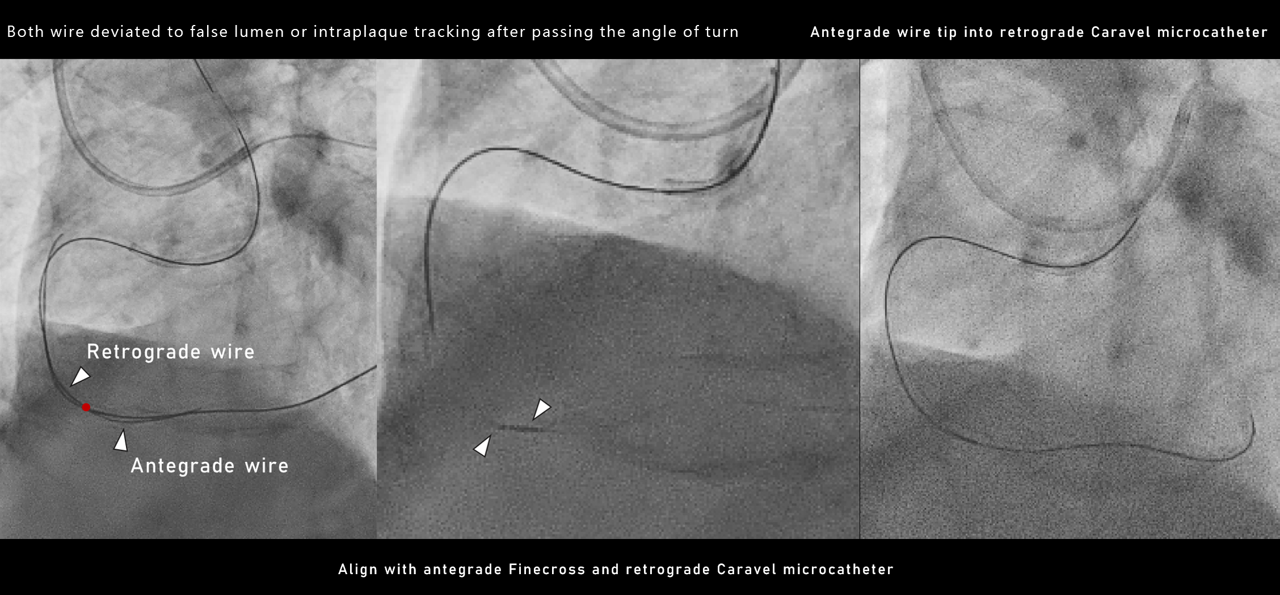
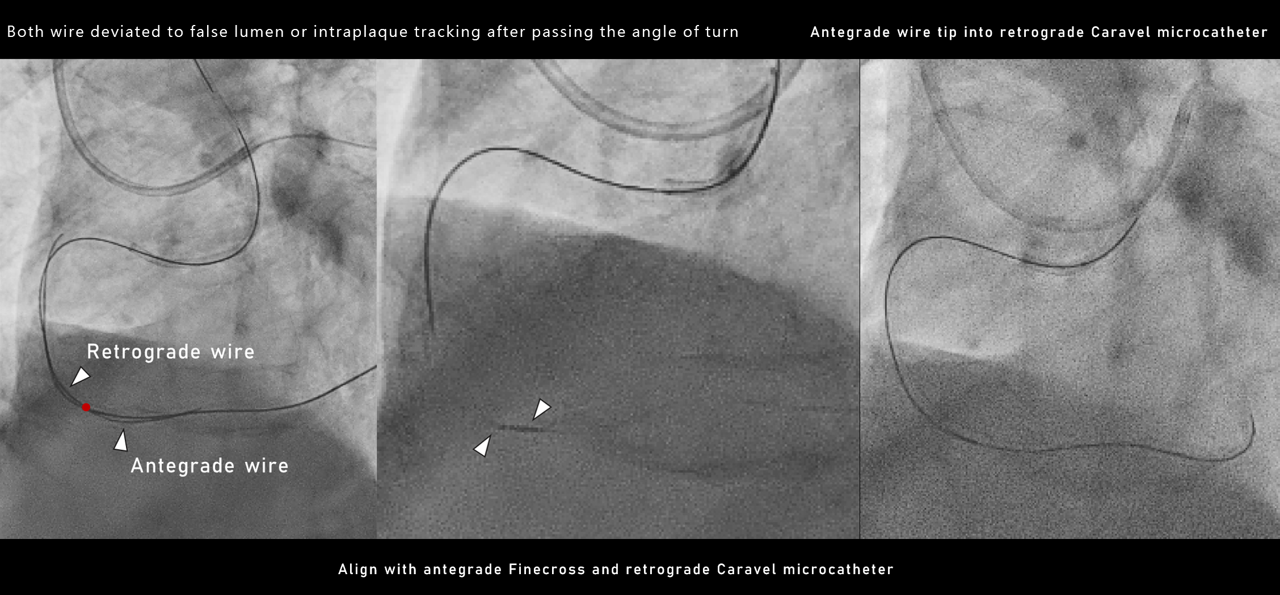
Consideringthe lesion complexity, we approached retrogradely using a Sion wire with abroken tip over a Caravel microcatheter, which crossed the collateral channelto distal RCA. Ultimate bros 3 wire for retrograde entry was challenging as itdeviated outside the true lumen after passing the transition of middle todistal segment, likely due to a suspected calcified nodule. Leaving anantegrade Fielder FC wire as a marker in the RV branch, we escalated theretrograde wire gradually. The Gaia 2 wire crossed the calcified noduled,followed by the Gaia 3 wire, achieving proximal RCA. Reverse CART was done, butthe retrograde wire could not reach the antegrade extension catheter.Therefore, we withdrew the retrograde wire distal to the RV branch, maintainingit as a marker, and transitioned to an antegrade approach using the Gaia 3 wirewith a Sasuke dual-lumen microcatheter on the Fielder FC wire. The Gaia 3 wiresucceeded in penetrating into RCA-PLV. However, intra-plaque tracking at theturning point was suspected because of the failure of the advancing balloon andthe wiring into the PDA. By aligning the antegrade Finecross microcatheter withthe retrograde Caravel microcatheter as closely as possible, we successfullyenabled the wire to cross into the retrograde microcatheter using the tip-inmethod. IVUS revealed the wire was entirely within the true lumen, and stentswere deployed from the ostium to the PDA. Both IVUS and angiographydemonstrated a good final result.

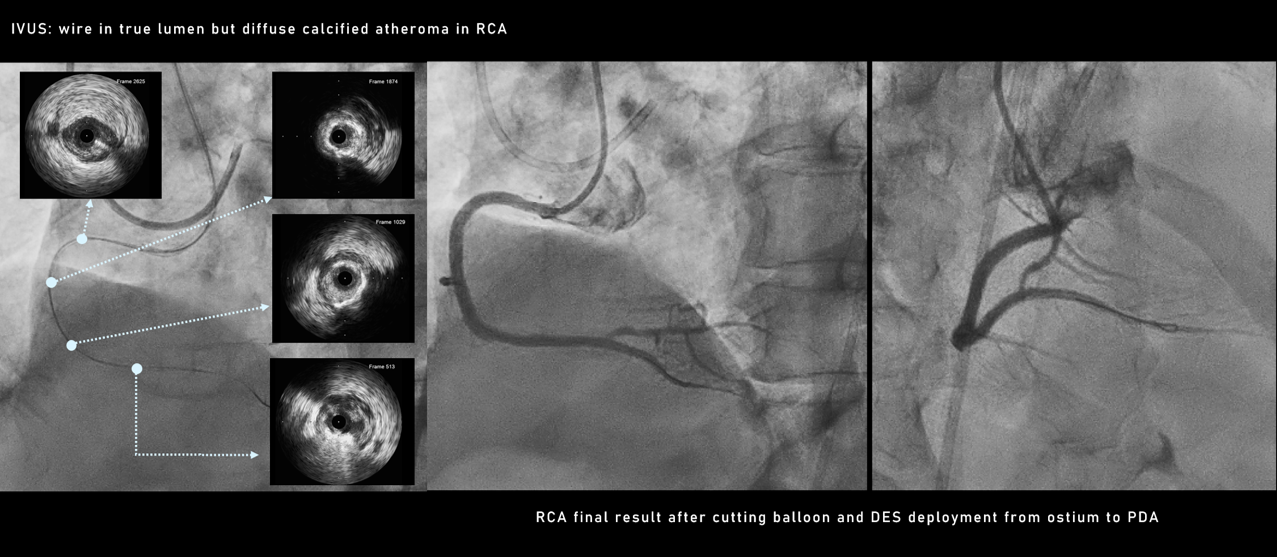

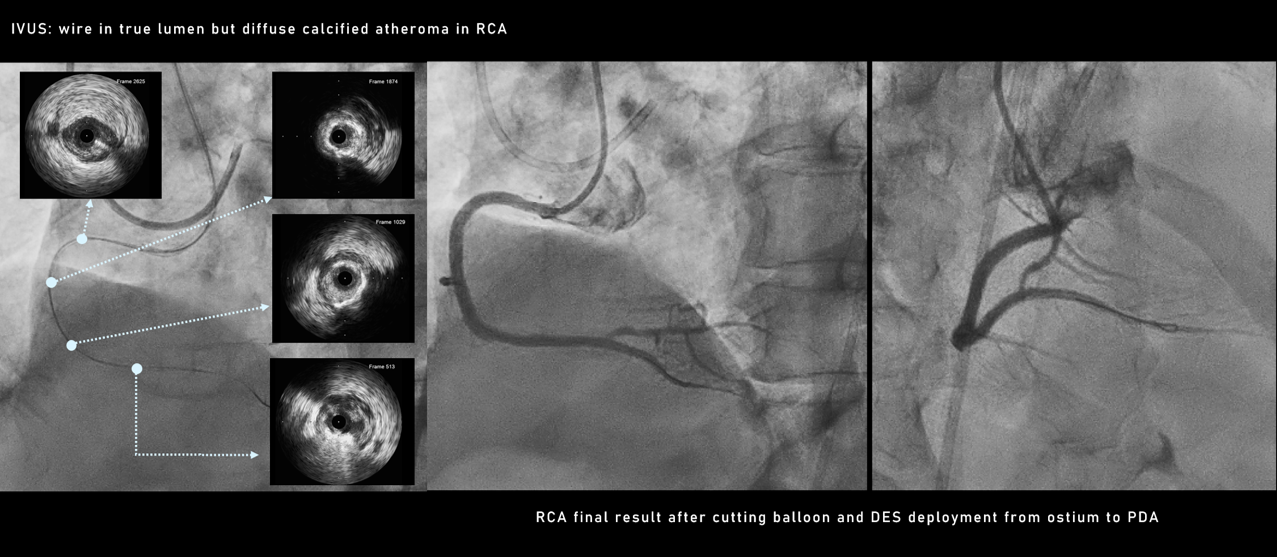
Case Summary
The original tip-in method was used as retrograde wiring to the antegrade microcatheter crossing and regarded as a modification of the Rendezvous method. Our case demonstrated the tip-in method could not only be an effective measure for bailing out of stagnation to a successful recanalization but also provide a strategy to overcome the calcification at the angulation that frequently leads to wire deviation into the false lumen during the CTO intervention.

