Lots of interesting abstracts and cases were submitted for TCTAP 2024. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-082
Out With the Old, in With the New: Previous Stent Rotablation With Intravascular Lithotripsy
By Mohd Asyiq Al-Fard Bin Mohd Raffali, Boon Cong Beh, Noor Diyana Binti Mohamad Farouk, Shawal Faizal Mohamad, Muhamad Ali SK Abdul Kader, Hamat Hamdi Che Hassan
Presenter
Mohd Asyiq Al-Fard Bin Mohd Raffali
Authors
Mohd Asyiq Al-Fard Bin Mohd Raffali1, Boon Cong Beh1, Noor Diyana Binti Mohamad Farouk1, Shawal Faizal Mohamad1, Muhamad Ali SK Abdul Kader2, Hamat Hamdi Che Hassan1
Affiliation
Hospital Canselor Tuanku Muhriz UKM, Malaysia1, Sultan Idris Shah Serdang Hospital, Malaysia2,
View Study Report
TCTAP C-082
Coronary - Complex PCI - In-Stent Restenosis
Out With the Old, in With the New: Previous Stent Rotablation With Intravascular Lithotripsy
Mohd Asyiq Al-Fard Bin Mohd Raffali1, Boon Cong Beh1, Noor Diyana Binti Mohamad Farouk1, Shawal Faizal Mohamad1, Muhamad Ali SK Abdul Kader2, Hamat Hamdi Che Hassan1
Hospital Canselor Tuanku Muhriz UKM, Malaysia1, Sultan Idris Shah Serdang Hospital, Malaysia2,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
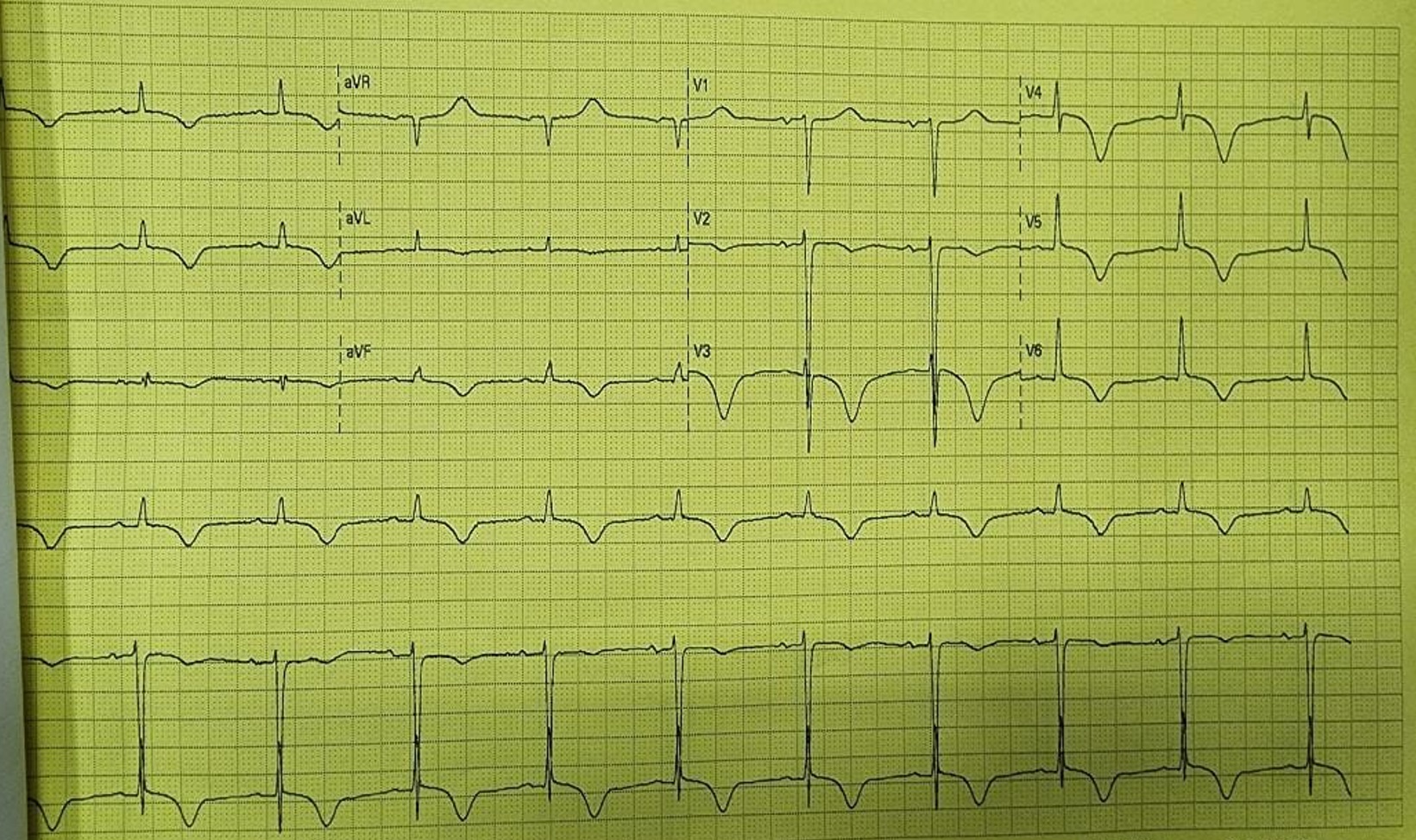
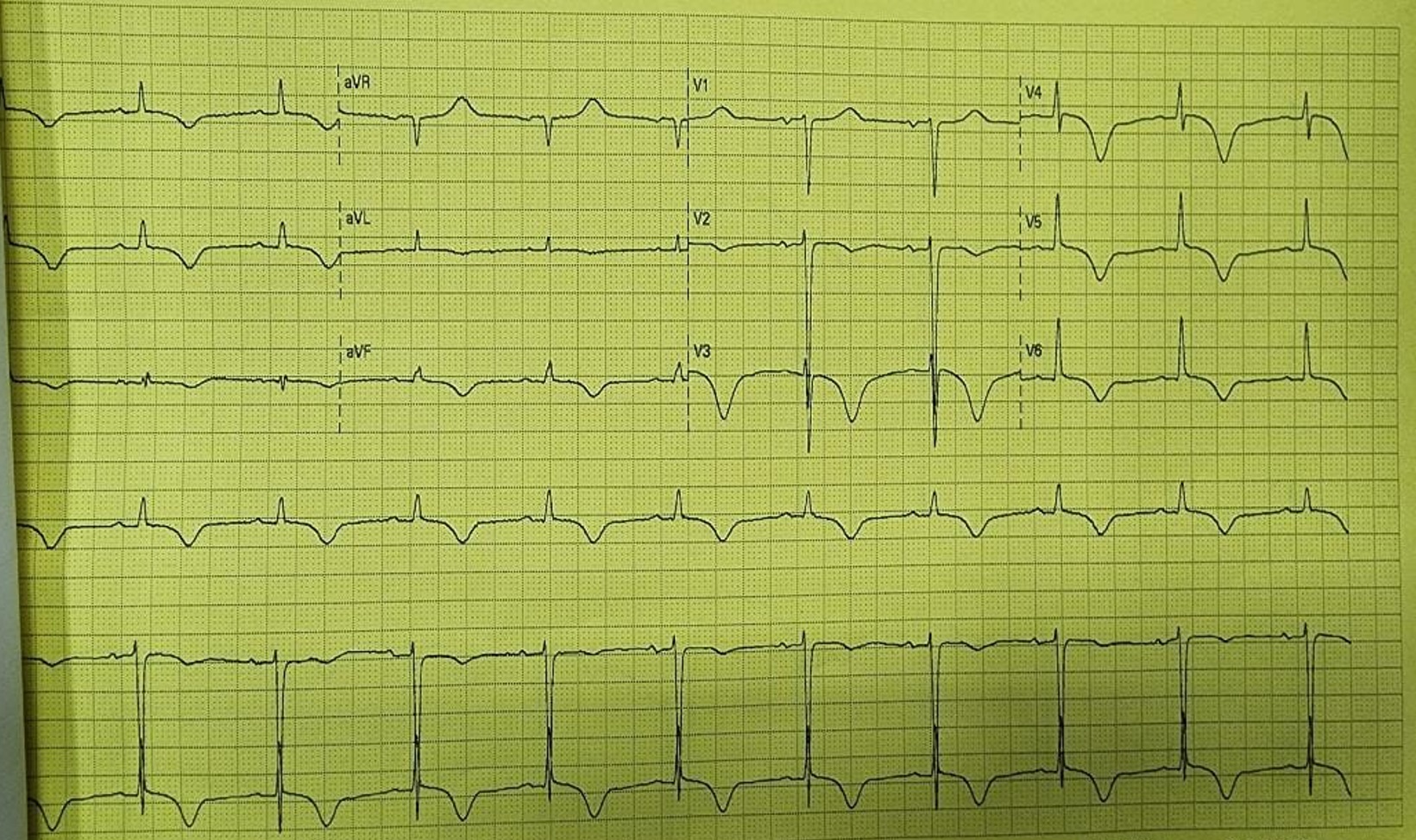
A 67 years old gentleman with hypertension, type II diabetes, dyslipidemia, and history of PCI to LAD in 2016 presents to the emergency department for severe chest pain. He was well previously, compliant to his medications, and stopped smoking since PCI was done. Upon arrival to the ED, his vitals signs were stable. His ECG showed Wellens changes (Figure 1), and bedside echocardiography showed subtle anterior hypokinesia.
Relevant Test Results Prior to Catheterization
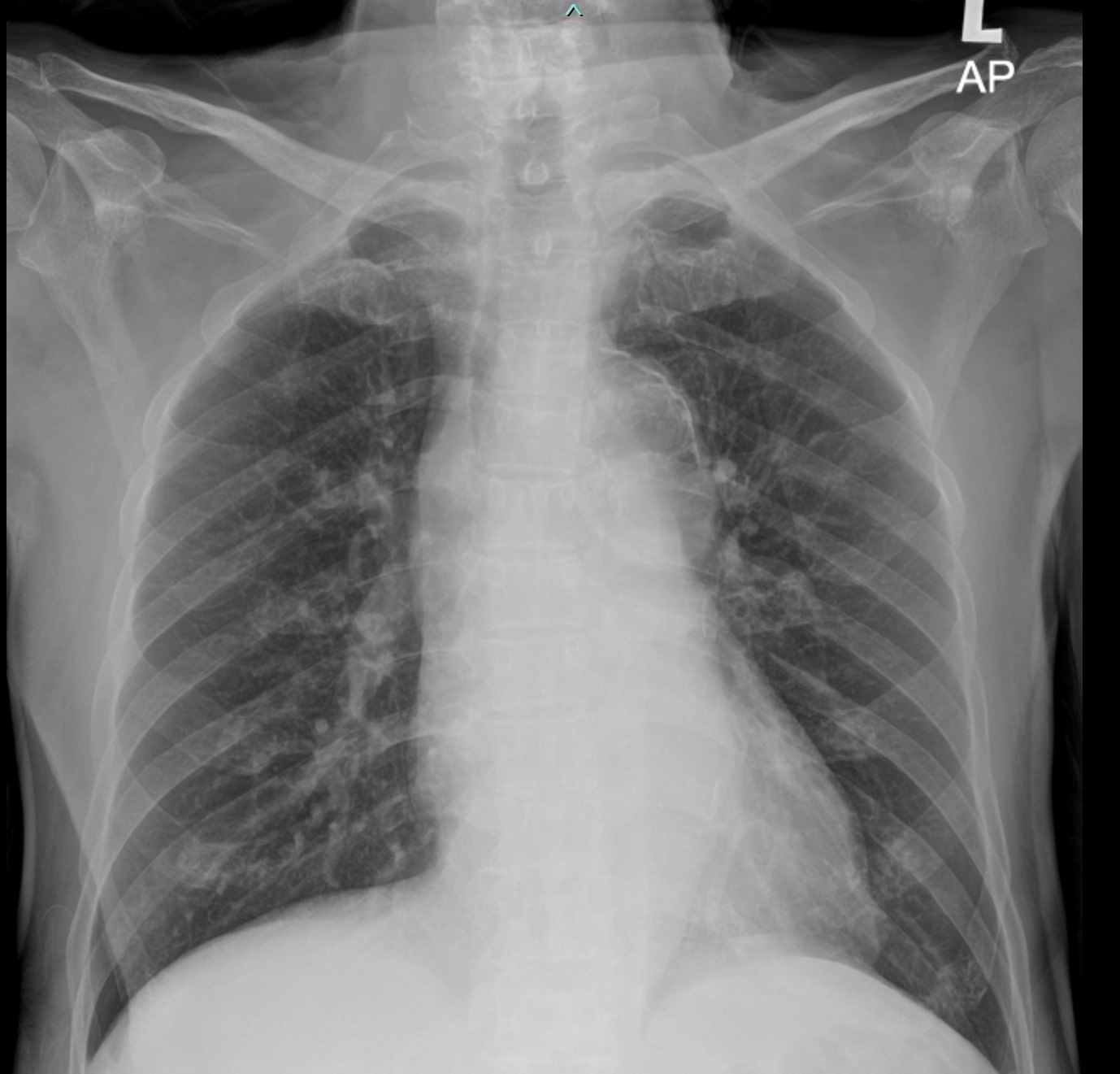
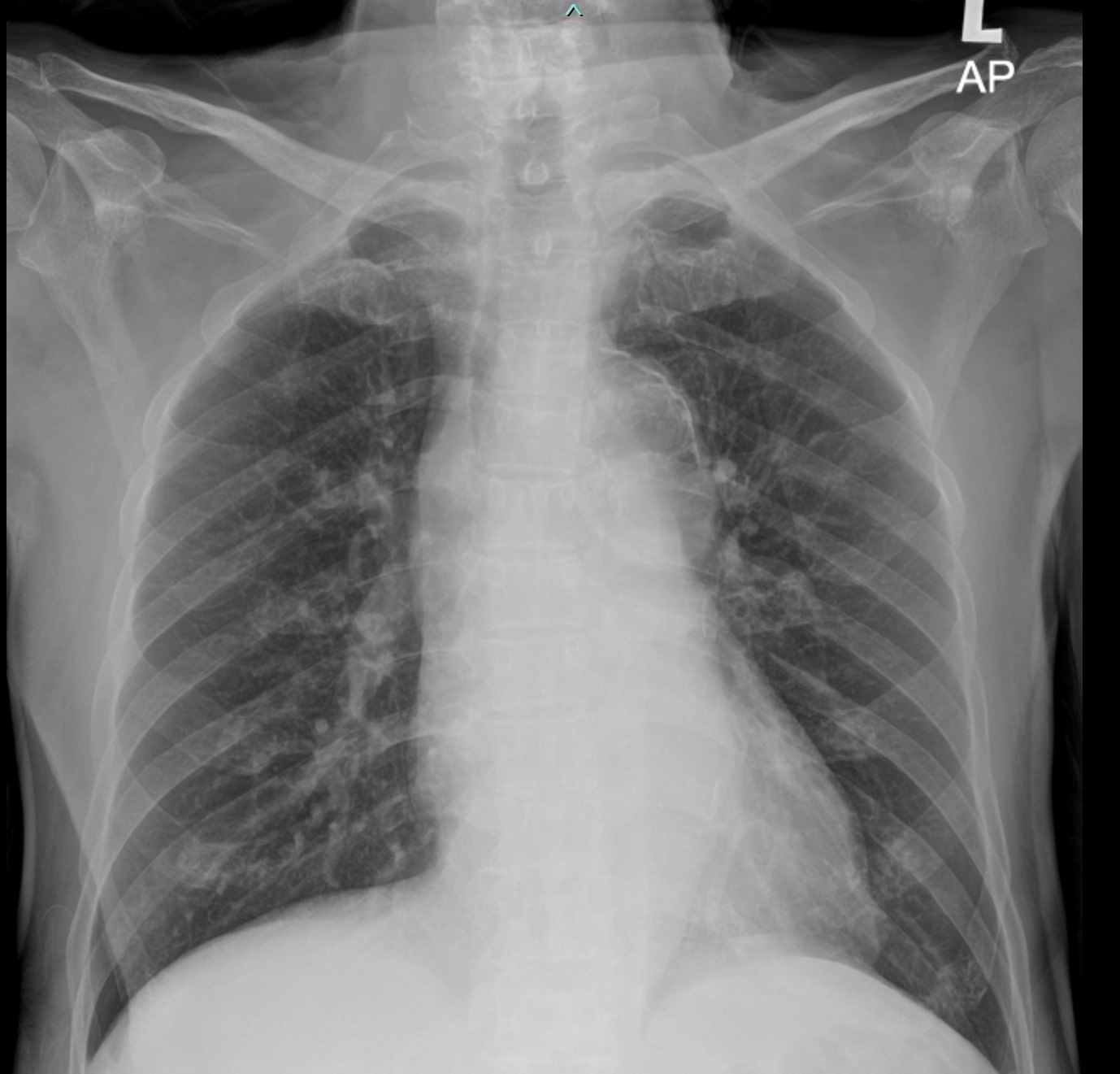
Further workup was done, his troponin levels were elevated. Chest radiography was clear with no widened mediastinum (Figure 2). At the time, the provisional diagnosis was NSTEMI, and patient agreed to proceed with cardiac catheterization.
Relevant Catheterization Findings
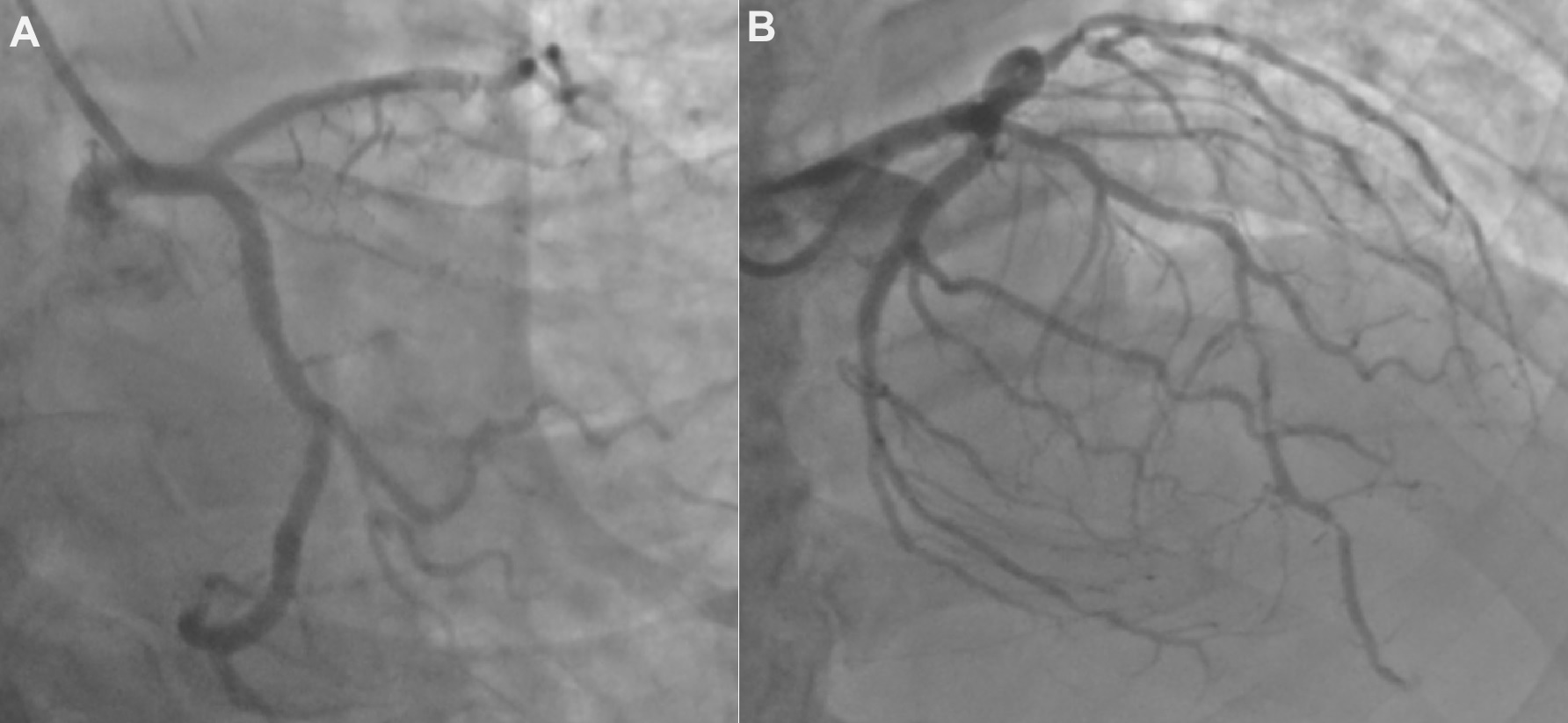
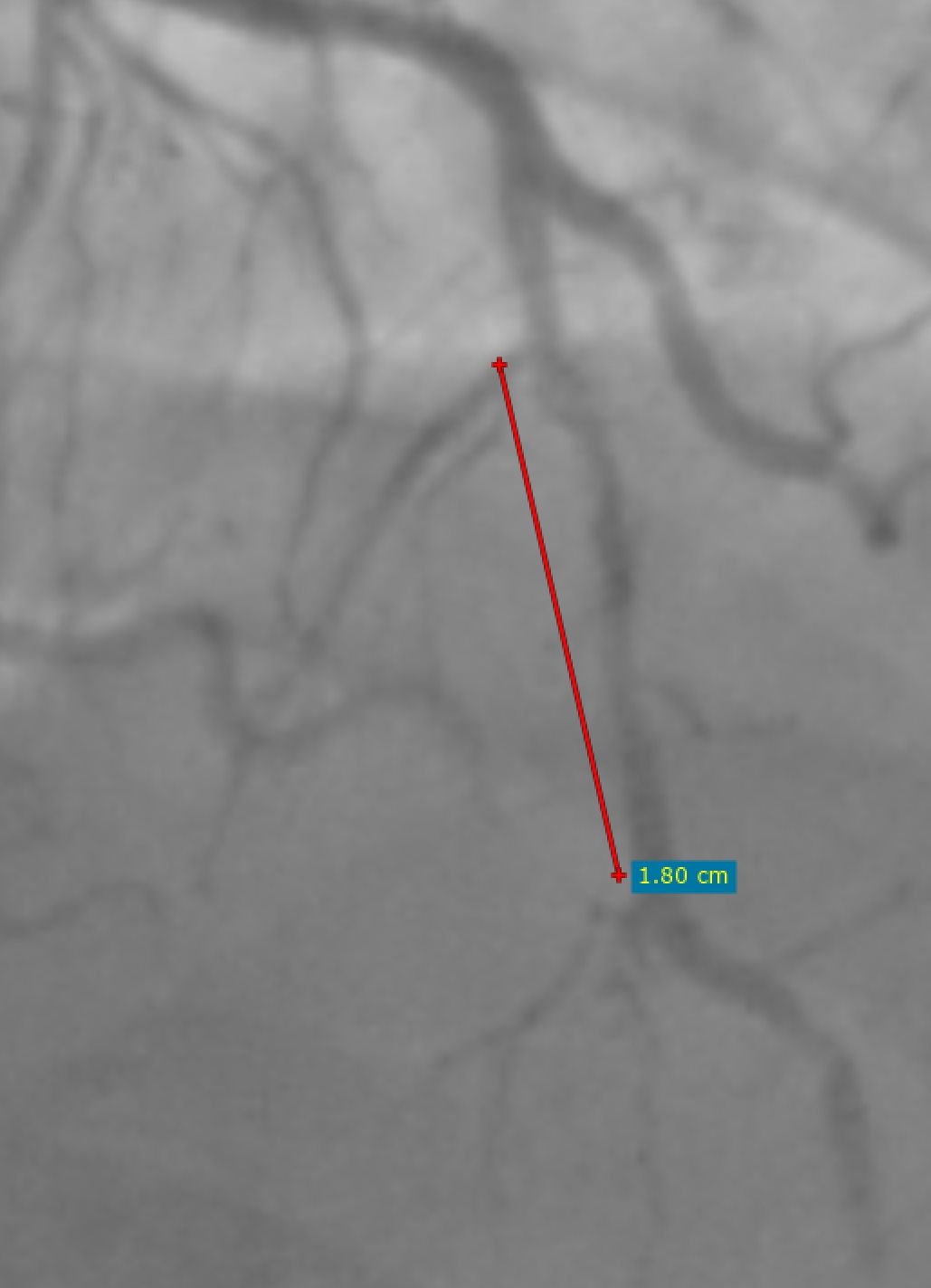
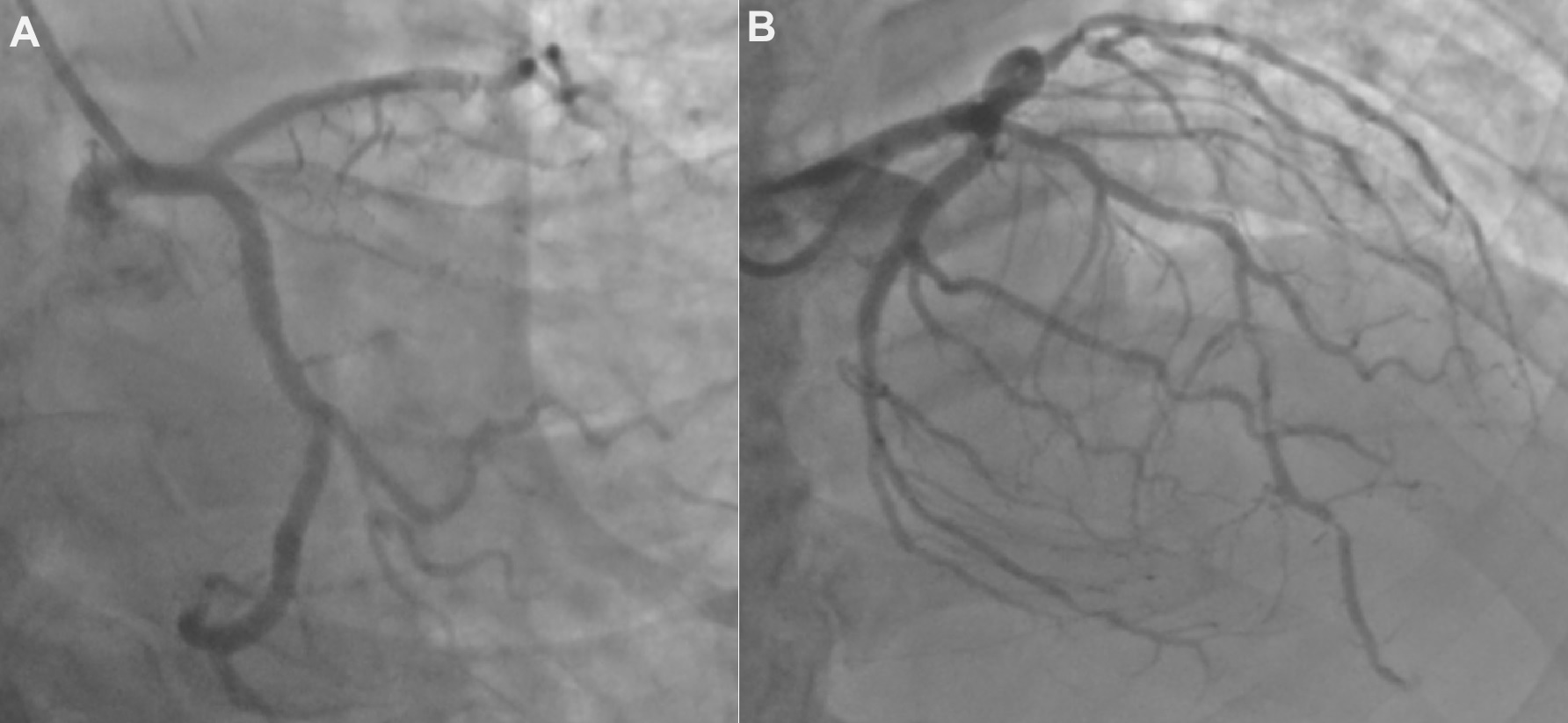
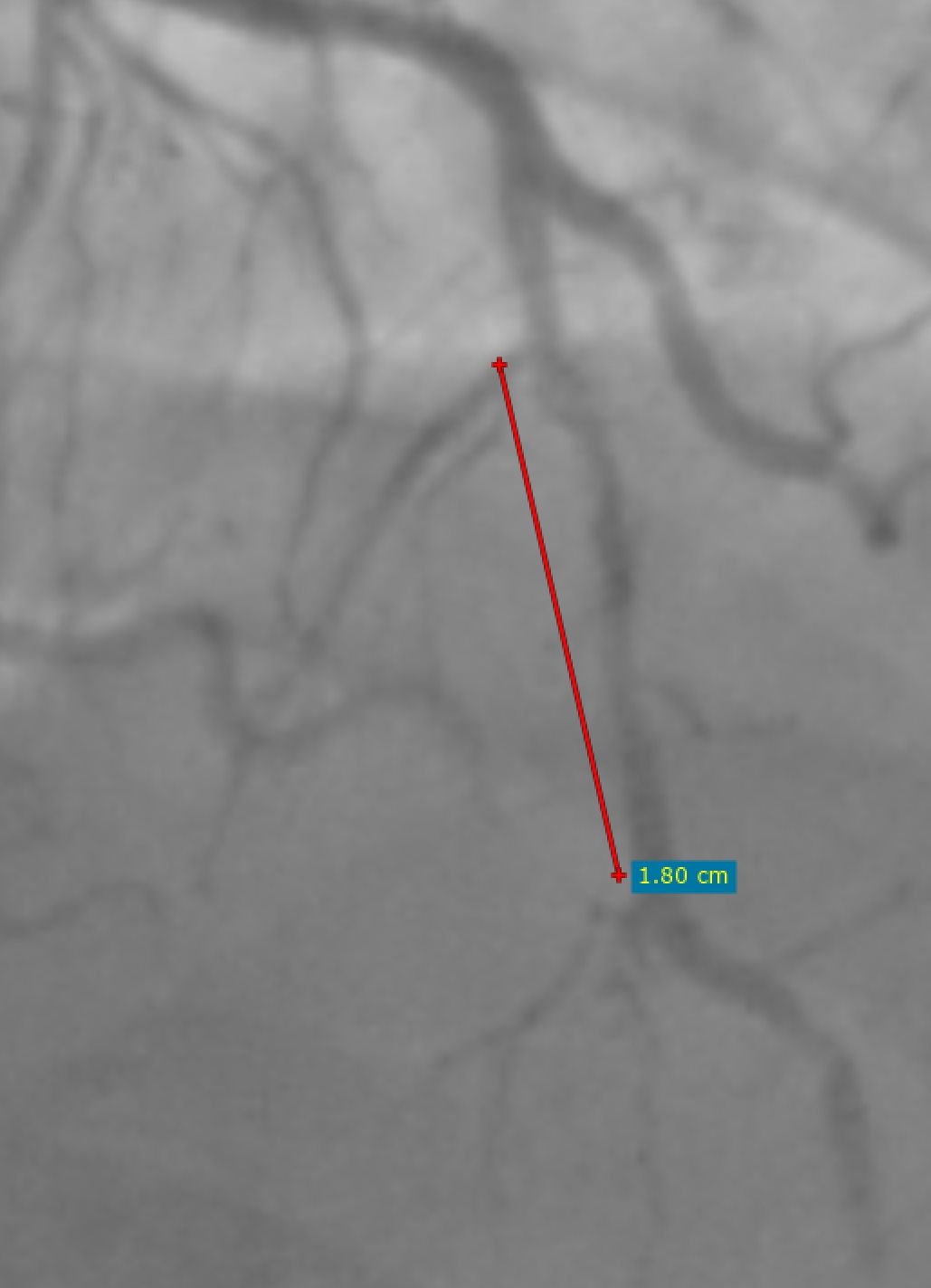
Diagnostic coronary angiogram was done via right radial access, showing severe ostial LAD disease of 80% stenosis with diffused calcifications followed by diffused moderate to severe ISR of the proximal to mid LAD stent 60-90%, mild left circumflex and RCA disease (Figure 3-4). The previous stent size measured 2.25x18mm (Figure 5).
Interventional Management
Procedural Step
We decided to proceed with PCI to LAD with an EBU 3.5 guide initially by performing IVUS, which showed severe ostial LAD disease with MLA of 4.3mm2 with 360 degree of calcification. Distal LM is healthy with vessel size of 4.0mm. Previous stent showed diffused severe ISR and undersized with vessel diameter of 3.0mm. Attempted to predilate stented segment with a 2.5x15mm NC balloon however unable to cross proximal part of stent even with a 10mm balloon, decided for rotational atherectomy from ostial LAD to distal part of stent (Figure 6). Total of 10 runs up to 180K RPM with rotablation done. Serial predilatations with NC balloon up to 2.75mm done. There was difficulty in delivering the first stent 2.75x40mm to cover the previous stent, only able to proceed with guide-extension support (Figure 7). Repeated IVUS run showed still uncracked calcium over the ostial to proximal LAD. Proceeded with IVL 3.5x12mm of up to 60 pulses over the area. Proceeded to stenting up to ostial LAD with a 4.0x44mm stent overlapping the previous stent. Postdilated with 4.0x15mm NC balloon afterwards with good final results (Figure 8).




Case Summary
Post procedure the patient was discharged well with no more chest pain. This is a complex ISR and calcified lesion case which required rotablation of the previous stent in order to put a larger stent, and subsequently IVL to provide effective calcium modification. This case showed the importance of intravascular imaging to properly size the vessel as the previous stent was markedly undersized. Although no large studies to determine the long term outcome of stent ablation, we believe that in some situations, stent ablation via rotational atherectomy is feasible and safe to prepare the diseased vessel for a larger stent.

